-
PDF
- Split View
-
Views
-
Cite
Cite
Inderjeet Bhatia, Daniel Tai-Leung Chan, Simon Chi-Cheung Lam, Timmy Wing-Kuk Au, Feasibility of novel transapical off pump beating heart mitral valve repair in a patient with dextrocardia and situs inversus, European Journal of Cardio-Thoracic Surgery, Volume 58, Issue 2, August 2020, Pages 392–394, https://doi.org/10.1093/ejcts/ezaa059
Close - Share Icon Share
Abstract
We present a case to demonstrate the feasibility of transapical beating heart mitral valve repair in a patient with dextrocardia. This minimally invasive technique provides simple, safe and satisfactory mitral repair. The surgical technique, outcome and prognosis are not affected by the condition.
CASE DESCRIPTION
A 61-year-old gentleman, known to have Kartagener syndrome involving dextrocardia with situs inversus and bronchiectasis (Fig. 1A), presented with progressive breathlessness and was in New York Heart Association functional class III. Transthoracic echocardiogram showed severe mitral regurgitation with the dilated left ventricle. Preoperative transoesophageal echocardiography (TOE) showed an anterior leaflet prolapse at the A1/A2 area, leaflet to annulus ratio of 1.27 (2.5 + 2.2/3.7 cm) (Fig. 1B). Spirometry results demonstrated that his forced expiratory volume in 1 second and forced vital capacity were 52% and 54% of predicted, respectively. His medical history included diabetes mellitus, hyperlipidaemia, pulmonary tuberculosis and ischaemic heart disease with stenting done 2 years ago. His calculated EuroSCORE II was 0.8%.
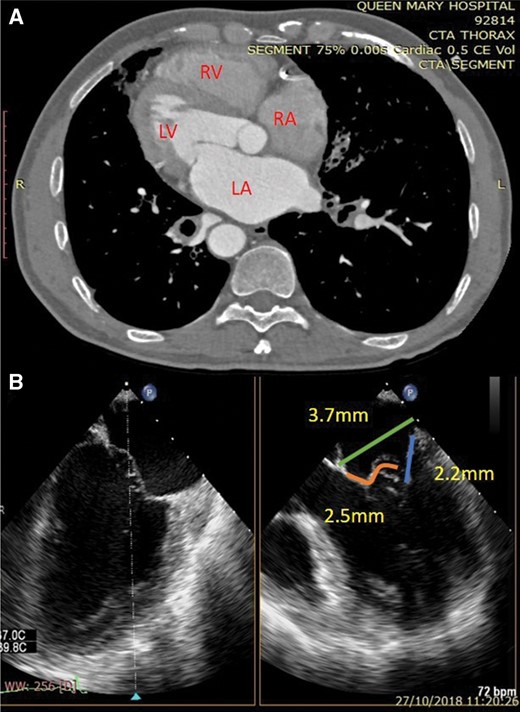
(A) Computed tomography thorax showing dextrocardia with LV apex towards the right side. (B) Preoperative transoesophageal echocardiography biplane view showing mitral valve measurements. LA: left atrium; LV: left ventricle; RA: right atrium; RV: right ventricle.
The patient was put under general anaesthesia with usual monitoring. Femoral arterial and venous sheaths were inserted for quick initiation of cardiopulmonary bypass (CPB) if required, and the CPB machine was on stand-by in the operating theatre. The positions of the surgical team and the equipment were reversed compared with the standard setting (Fig. 2A). A 5-cm right thoracotomy through the 5th intercostal space was performed and an apical entry site was identified by finger palpation and TOE. The NeoChord DS 1000 system (NeoChord, Inc., St. Louis Park, MN, USA) was introduced into the left ventricle cavity of the beating heart. The rest of the procedural details have been described previously [1, 2]. Procedural TOE is shown in Video 1. The implantation procedure was repeated to distribute 6 neochordae to the prolapsing segments. The final evaluation with TOE showed mild central residual mitral regurgitation (Fig. 2B). The total procedure time was 3 h, and 1 unit of packed red blood cells was transfused. The patient was extubated after 5 h and the rest of his postoperative course was uneventful. He was discharged on the 7th postoperative day and showed symptomatic improvement after 1 month. Seven months after the procedure, the patient was asymptomatic and follow-up transthoracic echocardiogram showed mild residual mitral regurgitation (effective regurgitant orifice area of 0.15 cm2), with the reverse remodelling of the left ventricle (preoperative vs follow-up: left ventricular internal dimension at end-diastole, 5.1 vs 4.7 cm) (Video 1).
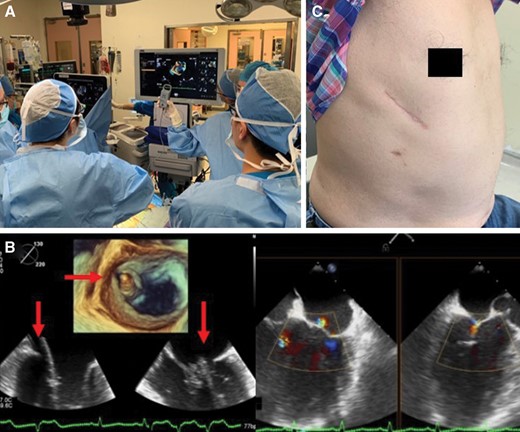
(A) Operating theatre showing the reversed position of surgeons on the right and the main monitor on the left. (B) Intraoperative 2- and 3-dimensional transoesophageal echocardiography showing the device (arrows) grasping the prolapsed segment and mild central regurgitation at the end of the procedure. (C) Right thoracotomy scar at follow-up.
Transoesophageal echocardiography showing preoperative prolapse, intraoperative procedure, final result and follow-up transthoracic echocardiogram.
DISCUSSION
Dextrocardia with situs inversus occurs in 1 per 10 000–50 000 births. We report here the first ever case of transapical beating heart mitral valve (MV) repair using the NeoChord DS 1000 system in a patient with this condition.
MV surgery via sternotomy or thoracotomy in dextrocardia has been reported in a few studies. As cardiac malposition resulted in visualization difficulties, intensive surgical preplanning and potentially risky procedural modifications or improvisations were needed to obtain sufficient exposure to the MV [3–5]. Minimally invasive techniques are seldom undertaken in such cases as these are technically challenging. Only one previous report has been published [3].
Transapical implantation of artificial chordae in a beating heart under TOE guidance with the NeoChord DS1000 device is a minimally invasive surgical technique to treat MV prolapse. It has been performed in more than 1300 patients worldwide. In patients with a suitable anatomy, this procedure has excellent results [1, 2].
Due to his comorbidities and the anticipated technical difficulties, he was considered as a high-risk surgical candidate and thus the alternative option of NeoChord procedure was considered. Although he was only the 15th case of the NeoChord procedure at our centre, we were confident with the procedure as we had performed other challenging cases before taking on this case.
As in any case of a NeoChord procedure, preoperative TOE assessment is the most important test and a calculated leaflet to annulus ratio >1.2 is needed to predict good coaptation after new chordae [1].
The procedure was performed in a standard operating theatre with routine monitoring and general anaesthetic set-up. Equipment that required reverse positioning was minimal and, therefore, did not cause confusion to the surgical team.
The most challenging part of the NeoChord procedure in dextrocardia is performing the TOE. An experienced echocardiologist is required since the angle to acquire desired images is reversed. In order to avoid confusion, we kept the same ‘lateral’ and ‘medial’ label for communication as in normal cases throughout the procedure, although that was not true anatomically.
In dextrocardia, the NeoChord procedure does not require modification in surgical technique compared with open surgery and offers an excellent alternative to conventional surgery.
Conflict of interest: none declared.




