-
PDF
- Split View
-
Views
-
Cite
Cite
Hasham Ahmad, Richard Porter, Hakeem Yusuff, Marius Roman, Extracorporeal membrane oxygenation for right ventricular failure following pericardiectomy, European Journal of Cardio-Thoracic Surgery, Volume 56, Issue 3, September 2019, Pages 625–626, https://doi.org/10.1093/ejcts/ezy491
Close - Share Icon Share
Abstract
We report the case of a 61-year-old gentleman who underwent pericardiectomy for constrictive pericarditis. Constrictive pericarditis was diagnosed through echocardiogram, computed tomography chest and cardiac magnetic resonance imaging. An elective decision was made for commencing venoarterial extracorporeal membrane oxygenation (ECMO) immediately postoperatively to prevent significant right ventricular failure (RVF). Postoperatively, the patient remained on ECMO for 4 days in a stable condition, showing no further signs of RVF. Venoarterial ECMO may be of use as an elective adjunct in cases at high risk of RVF following pericardiectomy.
INTRODUCTION
Pericardiectomy for patients with constrictive pericarditis (CP) is not a commonly performed cardiac surgery operation, and there is limited experience in the management strategies [1]. Venoarterial extracorporeal membrane oxygenation (VA-ECMO) is a new method of providing cardiorespiratory mechanical support, with early reports indicating low thresholds in patients developing right ventricular failure (RVF) [2–4].
We report the case of a patient with CP at high risk of developing RVF postoperatively, who was placed electively on VA-ECMO in the immediate postoperative period.
CASE REPORT
The patient presented with worsening breathlessness, decreasing exercise tolerance capacity and weight loss. Medical history included severe pectus excavatum, with reduced left lung volume and mediastinal shift. He underwent a left pleural biopsy, which showed inflammatory changes, with no evidence of malignancy. CP was diagnosed through transthoracic echocardiogram, computed tomography chest and cardiac magnetic resonance imaging (MRI). The patient was considered to be at high risk for developing RVF postoperatively based on a combination of decreased preload (because of CP and the presence of pericardial effusion), a dilated right ventricle (assessed by MRI and tranoesophageal echocardiogram (TOE) parameters) and raised pulmonary vascular resistance (PVR) due to left lung collapse.
Transthoracic echocardiogram
The pericardium appeared bright and thickened. Pericardial collection was measured at 1.6 cm. Respiratory variation and flow reversal into the hepatic vein were noted. The inferior vena cava was normal in size, with <50% collapse changes.
Computed tomography chest
Widespread pleural and pericardial thickening was reported, alongside severe pectus excavatum contributing to the reduction in left thoracic volume.
Operation
ECMO cannulation was performed electively as a preoperative step via the left common femoral vein and right common femoral artery. A phrenic to phrenic excision extending to the diaphragm and neck vessels was performed. Once the constriction of the right ventricle and right atrium was released, these became distended with the elevated right atrial pressures, and the TOE demonstrated a transient deterioration in RV function. The RV dysfunction was quantified through the following parameters: (i) the dilated right ventricle—quantified by the right ventricle/left ventricle ratio = 1.2 (normal value ≤1); (ii) tricuspid annular plane systolic excursion (TAPSE) = 1 cm (normal >1.6 cm in ventilated or 2.4 cm in non-ventilated patients); (iii) a straight septum appearance in the end systole; and (iv) poor radial RV function. The right ventricular function was seen to progressively improve on TOE.
The patient remained on ECMO for 4 days postoperatively. Following successful weaning from ECMO, the decannulation was performed through a surgical cut-down and primary closure. Mildly deranged liver function tests (ALP 185 IU/l and ALT 21 IU/l) and coagulation profile were noted. These normalized prior discharge, whereas ultrasound scans showed no signs of liver failure or liver congestion.
Histology
Both pleural and pericardial biopsies showed non-specific inflammation and diffuse benign fibrosis. There were no features to suggest IgG4 disease.
Cardiac magnetic resonance imaging
There was an increase in the left ventricular/RV volume and decreased end-diastolic pressure when comparing the post-pericardiectomy with the preoperative cardiac MRI. There was marked reduction in thickening surrounding the heart postoperatively (Figure 1).
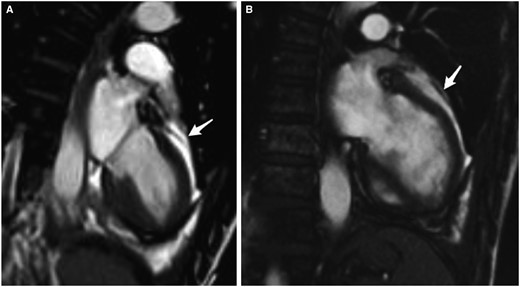
Cardiac magnetic resonance imaging. (A) Prepericardiectomy and (B) post-pericardiectomy. Arrow indicates marked reduction in pericardial thickening post-pericardiectomy.
DISCUSSION
The NICE guidelines state that the use of VA-ECMO in acute heart failure is adequately evidenced; however, there is uncertainty about which patients are likely to benefit from elective VA-ECMO [2]. The current limited evidence on safety shows a high incidence of serious complications [3, 5].
Some aspects are unique in this case: (i) the severe pectus excavatum, reducing the left thoracic volume; (ii) no histological evidence for IgG4-related disease and (iii) the use of VA-ECMO as elective adjunct for definitive surgery. In this case, VA-ECMO allowed the survival and recovery of the patient through the critical postoperative period, without the presence of significant right heart failure. This approach may be considered as a bridge and risk reduction strategy in patients at high risk of developing RV dysfunction following pericardiectomy. The implementation of this approach and threshold should be supported by further randomized controlled trials.
Conflict of interest: none declared.




