-
PDF
- Split View
-
Views
-
Cite
Cite
Konstantinos Spiliotopoulos, Ourania Preventza, Kim I de la Cruz, Joseph S Coselli, Management of expanding aortic arch aneurysm after hybrid endovascular and debranching repair, European Journal of Cardio-Thoracic Surgery, Volume 54, Issue 1, July 2018, Pages 185–186, https://doi.org/10.1093/ejcts/ezx502
Close - Share Icon Share
Abstract
Hybrid procedures are used to treat aneurysms of the transverse aortic arch (TAA), combining debranching of the brachiocephalic vessels with endovascular approaches. Continued enlargement of the aneurysmal sac is a late complication. A 60-year-old man presented with an expanding transverse aortic arch aneurysm after prior hybrid repair and underwent left posterolateral thoracotomy, partial excision of the previous stent graft and replacement with an interposition graft.
INTRODUCTION
TAA aneurysms constitute approximately 10% of thoracic aortic aneurysms. Hybrid treatments have recently emerged. Postoperative enlargement of the aneurysmal sac without an identifiable endoleak (i.e. Type V endoleak/endotension) has been observed with endovascular aortic repair [1, 2].
CASE DESCRIPTION
A 60-year-old man presented with recurrent chest and neck pain and nausea 3 years after TAA aneurysm repair elsewhere with median sternotomy, supra-aortic debranching of the innominate and left common carotid arteries, extra-anatomic bypass to the ascending aorta via a Dacron graft and endovascular exclusion of the arch aneurysm.
Chest computed tomography angiography (CTA) revealed an 8.7-cm aneurysm of the aortic sac around the previously implanted stent graft (Medtronic Valiant, size not specified in medical records) at the distal transverse aortic arch (TAA) and proximal descending thoracic aorta (Fig. 1A, see Supplementary Material).
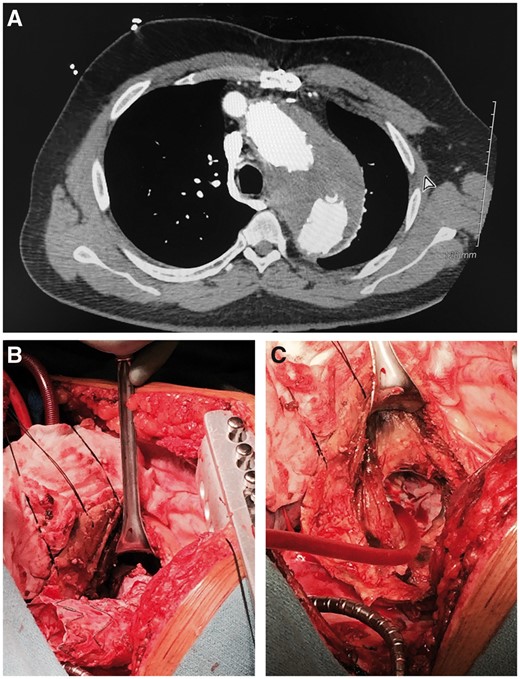
(A) Preoperative chest computed tomography angiography: aneurysm. (B) Stent graft firmly adhered. (C) Part of stent graft.
RESULTS
The patient was haemodynamically stable and underwent an urgent left posterolateral thoracotomy through the 5th intercostal space with cardiopulmonary bypass via the left common femoral artery and vein, and a spinal drain was used. A left inferior pulmonary vein cannula was placed and Y-connected to the left common femoral vein cannula, to augment the volume of the venous return and decompress the left ventricle. Hypothermic circulatory arrest at 22°C was employed. The proximity of the aneurysm and the stent graft to the previous debranching aortic conduit and the large size of the aneurysm precluded the placement of a proximal clamp.
The original stent graft was intact with no defects or kinks but densely adhered to the aortic arch wall, making full extraction unsafe; there was no evidence of infection, and access to the proximal part was limited (Fig. 1B). Therefore, partial extraction of the stent graft was performed by resecting it approximately 2 cm from its proximal end (Fig. 1C). We then resected the aneurysm, extracted the distal portion of the stent graft and replaced it with a 28-mm woven Dacron interposition graft with an 8-mm side branch (Fig. 2A), which was sewn end-to-end directly onto the salvaged proximal portion of the stent graft, with sutures placed through both the stent graft and the adherent aortic wall to ensure haemostasis (Fig 2A and B), as described elsewhere [3].
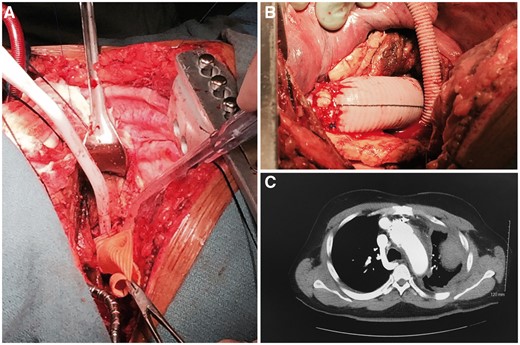
(A) Proximal anastomosis. (B) Distal anastomosis. (C) Postoperative chest computed tomography angiography: successful repair.
The patient’s postoperative course was uneventful; he was discharged from hospital on postoperative day 11 and had a successful repair (Fig. 2C).
DISCUSSION
The standard of care for TAA aneurysms is open repair with a Dacron graft and reimplantation of the brachiocephalic vessels, either separately or as an ‘island’ patch and carries increased morbidity and mortality, although progress has been made [4].
Hybrid procedures for the management of TAA aneurysms are predominantly intended for high-risk patients with significant comorbidities or prior open aortic surgery. However, the risk of stroke is still higher than for DTA TEVAR procedures [5]. Early morbidity and mortality rates remain low, but there is limited information regarding long-term outcomes and durability; they are prone to Type IA endoleaks, which can cause expansion of the existing aneurysmal sac, because of the compromised proximal landing zone and the significant curvature of the aortic arch, which increases the blood flow-induced shear stress and radial force in this segment.
Herein, no Type I, II or III endoleak was identified. Instead, a Type V endoleak/endotension was consistently suggested as the culprit. A high left posterolateral thoracotomy was performed as the main aneurysmal sac was located in the left chest and to avoid re-entry through a median sternotomy, which could increase the risk of inadvertent injury to the heart and vasculature. We chose not to address this enlarging aneurysm by implanting another endovascular stent graft due to lack of Type I endoleak evidence.
SUPPLEMENTARY MATERIAL
Supplementary material is available at EJCTS online.
Conflict of interest: Joseph S. Coselli participates in clinical research trials for Bolton Medical; consults for, receives royalties and a departmental educational grant from, and participates in clinical trials for Vascutek Terumo and consults and participates in clinical trials for Medtronic, Inc. and WL Gore & Associates. Ourania Preventza consults for Medtronic, Inc. and W.L. Gore and associates. Other authors have no conflicts to disclose.




