-
PDF
- Split View
-
Views
-
Cite
Cite
Amer Harky, Hewran A Mohammad, Megan Garner, Muhamed S Alani, Fistula of right internal thoracic artery as a rare cause of chest pain, European Journal of Cardio-Thoracic Surgery, Volume 53, Issue 3, March 2018, Pages 684–685, https://doi.org/10.1093/ejcts/ezx327
Close - Share Icon Share
Abstract
Variation in the origin of the internal thoracic arteries has been previously described and reported in the literature; however, there has been no report of an anomalous termination of the right internal thoracic artery into the pulmonary vein persisting and presenting in adult life. We report the case of the right internal thoracic artery originating from the first part of subclavian artery but terminating into the right superior pulmonary vein that presented during the third decade of life.
CASE REPORT
A 38-year-old man with no significant medical history presented with repeated episodes of chest pain for more than 1 year. The chest pain was sharp in nature with radiation to shoulders. There was no particular inducing or relieving factors.
On admission, electrocardiography showed normal sinus rhythm, transthoracic echocardiography showed normal ventricles and valves and chest radiography was unremarkable. An elective extended coronary angiogram showed a tortious, dilated ectatic right internal thoracic artery (ITA) to the right superior pulmonary vein (Fig. 1, Videos 1 and 2) with otherwise normal coronary arteries. Because of the recurrent and disturbing nature of the chest pain, the patient underwent elective correction of this anomaly. The patient underwent a right anterior minithoracotomy, the anomalous vessel was identified, the proximal and the distal ends were ligated and the right ITA was divided (Fig. 2). The patient’s postoperative course was uneventful and was discharged in good health on Day 3 post-surgery. The patient did not experience any chest pain during in-hospital period and at 1-year follow-up in clinic.
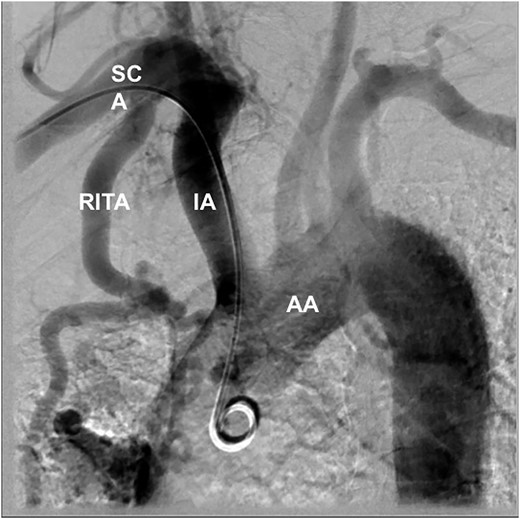
Extended coronary angiogram showing the RITA terminating into the pulmonary vein, SCA, BA and AA. AA: aortic arch; BA: brachiocephalic artery; RITA: right internal thoracic artery; SCA: subclavian artery.
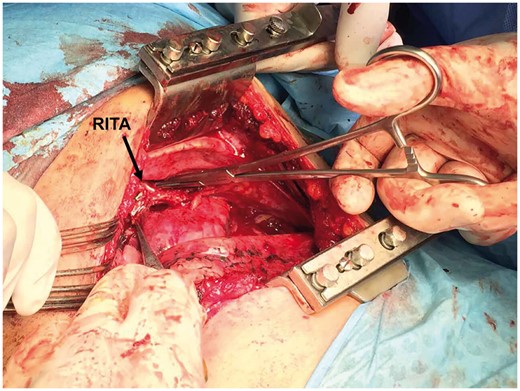
Intraoperative image showing a large RITA. RITA: right internal thoracic artery.
Extended coronary angiogram showing the right internal mammary artery terminating into the pulmonary vein.
Extended coronary angiogram showing the right internal mammary artery terminating into the pulmonary vein.
DISCUSSION
The internal thoracic artery arises from the first part of the subclavian artery in most cases. It then passes behind the costal cartilages of the upper 6 ribs and terminates into 2 branches, the musculophrenic and the superior epigastric arteries, most commonly at the level of the sixth intercostal space [1]. Henriquez-Pino et al. [2] encountered the presence of a third terminal, diaphragmatic ITA branch in 7% of cases, whereas trifurcation of the artery was also found in 12.5–61.3%, including a xiphoid branch.
On the other hand, fistulous connections between the pulmonary vessels and the systemic arteries, such as the ITAs, are rare [3] and often asymptomatic. Arteriovenous fistulae of the ITAs have previously been split into 3 groups based on their anatomical connections. First, there are fistulae connected to the internal thoracic vein, vena cava or innominate vein; second, those which connect to the pulmonary circulation and finally those which connect to the vitelline venous system [4]. These fistulae can be either congenital or acquired due to trauma or infection. In the case of congenital fistulae, it is thought that these connections occur due to accessory bronchial arteries arising from the ITA [5].
Detecting systemic vessel to pulmonary vein anomalies may be challenging as it may not produce a detectable shunt during right heart catheterization. Instead, these are usually detected on coronary angiography, which is the gold standard for identifying such lesions as it allows determination of the anatomy of the feeding and draining vessels [3]. In addition, it will demonstrate any pulmonary parenchymal involvement. During the pulmonary angiogram, the increased flow may produce dilatation and tortuosity of the draining vessel.
We believe this is the first reported case of an anomalous right ITA terminating into the right pulmonary vein. Angiography is the gold standard for diagnosis of such anomalies. In patients presenting with chest pain with a normal coronary angiography, one should consider whether arterial anomalies maybe responsible for their presenting symptoms.
Conflict of interest: none declared.
REFERENCES
Author notes
Amer Harky, Hewran A. Mohammad, Megan Garner and Muhamed S. Alani contributed equally into writing this article.




