-
PDF
- Split View
-
Views
-
Cite
Cite
Giulio Rizzoli, Laura Schiavon, Pierantonio Bellini, Does the use of bilateral internal mammary artery (IMA) grafts provide incremental benefit relative to the use of a single IMA graft? A meta-analysis approach, European Journal of Cardio-Thoracic Surgery, Volume 22, Issue 5, November 2002, Pages 781–786, https://doi.org/10.1016/S1010-7940(02)00470-0
Close - Share Icon Share
Abstract
Objectives: Does the use of bilateral internal mammary artery (IMA) grafts provide incremental benefit relative to the use of a single IMA graft? Methods: Meta-analysis by qualitative and quantitative protocol of the studies published in the literature in the last 15 years. Only eight, out of 149 observational studies found, met our criteria: surgical results of bilateral versus single IMA, patient age range from 20 to 89 years, exclusion of emergency and diabetic patients, study group larger than 100 patients, minimal follow-up time. The final sample size included 16 362 patients. Results: Late survival was evaluated at 5 and 10 years. The hazard ratio (HR) was calculated from seven studies, the difference of survival was from six and five studies, respectively. The effect size was summarized using a random effect model, suggested by the results of statistical test for homogeneity of the HR (P<0.05) and of the survival difference at 5 (P<0.05) and at 10 years (P<0.05). The bilateral IMA estimate of combined HR was 0.79 (95% confidence limits, C.L.=0.66÷0.91). The combined difference of survival probability at 5 years was 0.014 (95% C.L.=−0.03÷0.06) and at 10 years was 0.07 (95% C.L.=0.003÷0.170). Conclusion: There is significant evidence in favor of decreasing death risk of bilateral versus single IMA procedure.
1 Introduction
Use of left internal mammary artery to graft left coronary stenosis was reported since the early 1980s [1]. Follow-up of surgical results has definitely shown that internal mammary graft has longer disease free duration, while saphenous vein graft are prone to develop severe atherosclerotic lesions within 10 years [2]. This causes longer survival, freedom from recurrence of angina, infarction and reoperation [3]. Additional survival benefit using both internal mammary arteries (IMAs) remains uncertain. However the trend toward arterial revascularization has steadily increased in recent years [4], therefore we emphasize the question if bilateral IMA graft is better than single IMA graft [5].
We reviewed the pertinent literature of the last 15 years to point out a possible survival difference between patients with two versus one mammary artery bypass and applied the rules and techniques suggested for research synthesis by the methodological guidelines for systematic literature reviews of randomized studies [6], with the suggested methodological safeguards for observational studies [7].
2 Methods
Meta-analysis of the bilateral and single IMA studies was organized making the below mentioned steps:
definition of outcomes of interest;
strategy of literature research and selection of the studies according to preset criteria;
evaluation of the study quality;
extraction of the effect size in each study;
quantitative summarization of the studies, according to a homogeneity test.
2.1 Definition of outcomes of interest
Primary outcome was late survival results evaluated at 5 and 10 years of follow-up. Secondary outcomes were reoperation, recurrence of angina and infarction.
2.2 Strategy of literature research and selection of the studies according to preset criteria
Studies of the past 15 years were identified through MEDLINE and EMBASE without any language constraint. Medical subjects headings were used to scan abstract titles and subjects in the databases, using the key words: ‘bilateral IMA’, ‘coronary artery bypass grafting and ((thoracic arteries) in MESH)’, ‘single versus bilateral IMA’. Visual revision of the literature listed in retrieved articles was further accomplished. Paper selection was done including studies with:
intra-institutional comparison of surgical results of bilateral IMA versus single IMA;
exclusion of higher risk patients operated on emergency base and of patients with clinical diabetes;
large operative age range including ages from 20 to 89 years;
study group larger than 100 patients;
follow-up time beyond the postoperative period.
These criteria evidenced that sufficient information were available for the primary outcome (survival) but were lacking for the secondary outcomes (reoperation rate, angina return, infarction).
2.3 Evaluation of the study quality
All the retrieved articles are observational studies. They have a large heterogeneity in methodology (study design, statistical analysis) and in presentation of results. Therefore we added to the clinical randomized studies criteria proposed by Chalmers [8] a study scoring protocol according to four different views: study description, protocol, statistical analysis, results presentation.
Subsequently we stratified an upper (1st group) and lower (2nd group) rank category selecting the median score as a cutpoint.
2.4 Extraction of the effect size
The most appropriate effect index to evaluate time related effect of surgical procedures was the hazard ratio (HR) and its 95% confidence limits (C.L.). The extraction of this index from statistically heterogeneous studies was performed according to the techniques suggested by Parmar [9]. An HR less than 1 indicates better results of bilateral IMA because of larger reduction of late mortality.
The difference of probability of survival of the two techniques, evaluated at 5 and 10 years, was also calculated and the joint survival probability difference was reported with its C.L.
2.5 Quantitative summarization of the studies
Summary of the HR of the selected studies required a prior statistical test for homogeneity (Q), to verify the hypothesis that the effect sizes are equal in all studies. If the Q statistic was greater than the critical value of chi square (P<0.05 at k-1 degree of freedom, were k is the number of the selected studies) the observed variance of the study effect size is significantly greater. This provides evidence of heterogeneity among the studies and requires a study combination based on a random effect model. In the reversed case, we would have applied a fixed effect model.
The method of DerSimonian and Laird [10] was used and the analysis was performed with the Statistical Package FAST*PRO, specifically designed for meta-analysis by the supporters of Confidence Profile Method [11].
3 Results
According to our literature research strategy we identified 149 studies. A total of 127 were found by means of computerized databases, the remaining by reviewing the printed references.
Out of 149, 66 studies were published in Japanese and we were not able to read them limiting our analysis to 83 English written studies. Among these only nine reported an intra-institutional comparison of the IMA surgical techniques. Each study was scored independently by two reviewers (agreement by the Cohen index, k=0.62). These nine studies fulfilled our selection criteria and their quality was further evaluated (Table 1) . According to our scoring system, four studies were classified in the upper rank and included 13 557 patients [4,12–14], four in the lower rank [15–18] including 4819 patients and the remaining study [19] was dropped because it did not pass our quality criteria. When analyzing the HR and its C.L. we were able to obtain this effect only in seven studies [4,12–17] and 15 299 patients, excluding Morris's study [18]. The heterogeneity test calculated a chi square of 20.09 (P<0.05) and supported the hypothesis of heterogeneity among the seven studies. The random effect model estimation of combined HR was 0.79 (95% C.L.=0.66÷0.91, P<0.05). Studies in the upper rank (1st group) had a HR of 0.72 (95% C.L.=0.61÷0.85, P<0.05), whereas studies in the lower rank (2nd group) had a HR of 1.18 (95% C.L.=0.77÷1.59, P=ns) (Table 2) . As suggested by Kirklin et al. [20] we plotted the HRs on a transformed scale (if HR>1 then plotHR=2-(1/HR), else plotHR=HR) that is equal in distance to the right and left of the identity hazard (1.0) (Fig. 1 , Table 2) so that a HR of 0.5 should be at an equal distance to the left from 1.0 as is 2.0 to its right. Difference of survival at 5 years was available in six studies [4,13–16] including a total of 12 473 patients. The heterogeneity Q test was 11.22 (P<0.05) and the combined random estimate was 0.014 (95% C.L.=−0.03÷0.06, P=ns) (Fig. 2 , Table 3) . Difference of survival at 10 years was available in five studies [4,12–13,15–16] with a total of 13 871 patients. The heterogeneity Q test was 45.88, (P<0.05). The combined random estimate was 0.07 (95% C.L.=0.003÷0.170, P<0.05) (Fig. 3 , Table 4) .
Summary of included studies (bilateral IMA – BIMA; single IMA – SIMA)
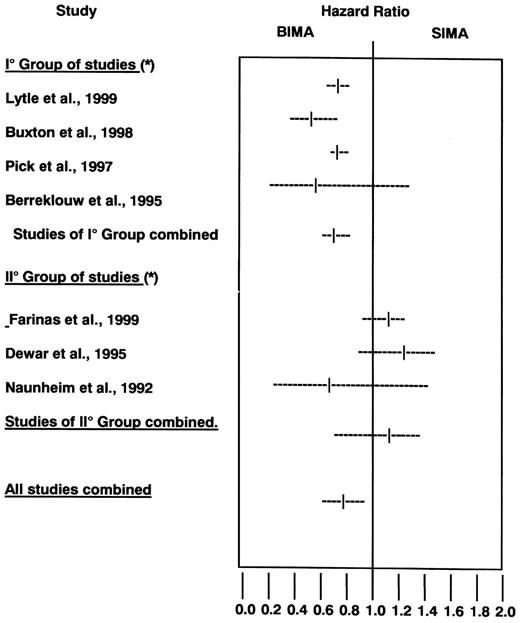
Summary of HR and 95% confidence limits from observational studies. BIMA=bilateral IMA graft, SIMA=single IMA graft. *=see Table 1.
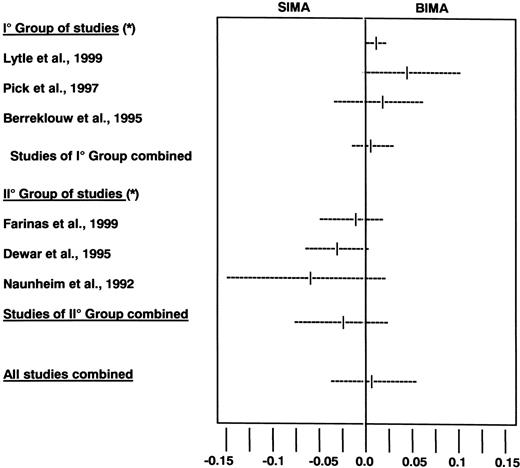
Summary of differences of survival probability at 5 years and 95% C.L. from observational studies. BIMA=bilateral IMA graft, SIMA=single IMA graft. P=NS. *=see Table 1.
Bilateral IMA versus single IMA, difference of survival at 5 years
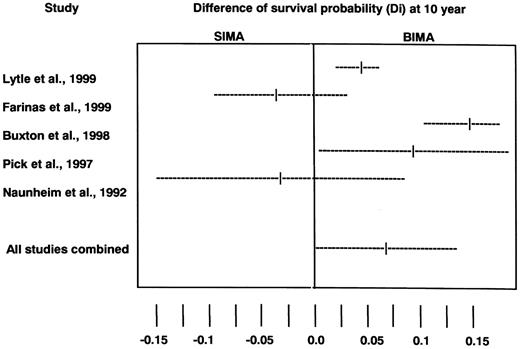
Summary of differences of survival probability at 10 years and 95% confidence intervals from observational studies. P<0.05, BIMA=bilateral IMA graft, SIMA=single IMA graft.
Bilateral IMA versus single IMA, difference of survival at 10 years
4 Discussion
Use of bilateral IMA versus single IMA to perform aorto-coronary bypass grafts in ischemic heart disease was the subject of a long debate among surgeons [21]. It has been demonstrated that left IMA bypass to the anterior descending artery has a better long-term survival [2] because of the favorable properties of arterial conduits as compared to venous conduits [3]. Therefore the syllogism: if single IMA is good, bilateral IMA could be even better! This change requires some modifications in long established operative routines (old habits die hard) and exposes to some specific complications [22]. Because treatment decisions must be based on available evidence and bilateral IMA grafting has not been a common operation in our as well as in most institution [21], we have performed a meta-analysis of the surgical series comparing surgical results of single versus bilateral IMA graft within their own institution.
No randomized data exist comparing bilateral IMA and single IMA and in non-randomized comparison patient and institution-related factors makes analysis and comparison difficult. Therefore the need of study selection. Nine observational studies satisfied our preset criteria [4,12–19]. Only eight of these studies were judged (by two independent raters) as eligible for the meta-analysis. We were aware that strict criteria reduced the total information, nonetheless they enhanced the most valued ‘result comparability’.
Accordingly we limited literature search to the last 15 years to exclude early operative era and ‘learning curve’ experiences and we decided to fix the ‘numerosity’ criteria to a moderately large ‘N’ (100 patients) to be confident in the reported results and to reduce the distortion sources.
In fact it has been stated that meta-analysis of non-randomized studies presents methodological difficulties and the results are not reliable [23]. We share the different opinion that some numerical information are better than none, therefore we utilized the methodological adjustments proposed by the Meta-analysis of Observational Studies in Epidemiology Group [7].
In the time domain the HR is one of the most appropriate index to compare late results of different techniques [9]. This ratio shows a 20% decrease of death risk of bilateral IMA procedure versus single IMA. Furthermore, if we look at the survival probability difference, there is a trend toward an increase difference at 10 years (7.0%) as compared to 5 years (1.4%).
Despite the scarcity of eligible studies our effective sample size adds up to 16 362 patients (in eight retained studies) and this gives support to our results. Although somewhat lower, patients number was nonetheless large when extracting the hazard index from seven studies and the survival difference at 5 (six studies) and 10 years (five studies).
We introduced restriction criteria to mitigate the effect of concomitant variables excluding studies with small samples or studies analyzing specific patient's cohorts as diabetics, urgent operations, limited age ranges and limited follow-up.
While emergent operations are an obvious source of confounding, because related to higher operative risk and prevalence of simpler operative techniques, the exclusion of diabetic patients is not equally obvious. Nonetheless in most series the prevalence of diabetic patients is much higher in single IMA patients than in bilateral IMA, because of the fear of sternal wound complication [24] and therefore diabetes, which is well known risk factor for late death [12,13,15], may equally confound ‘an apple to apple’ comparison of the results of the two techniques. A single study examined propensity matched patients in regard to diabetes and left ventricular function and showed improved survival with the use of bilateral IMA in both groups [5].
It was not possible to model the source of variability among studies by stratification of concomitant variables and it was difficult to obtain effect sizes stratified for well known incremental risk variables as the extension of disease and ejection fraction. We were therefore forced to limit our heterogeneity test on study rank stratification.
Despite our attention to enhance the homogeneity of the studies, the absence of generalized and commonly shared guidelines for the set-up and data reporting of the observational studies also disturbed our meta-analysis.
In conclusion we believe that bilateral IMA treatment can generally offer better long term results than single IMA.
Because of scarcity and poorness of information concerning complication rates and symptom's relief, our focus was merely on survival. There is need of further observational studies on secondary outcomes and of establishing common guidelines for conducting and reporting on observational studies.
Taking studies performed in different countries on heterogeneous groups of patients with different selection criteria, follow-up strategies and statistical analysis and combining them may seem hazardous. Nonetheless, in the absence of well controlled randomized studies this is a suggested approach to search for the ‘best evidence’ [25].
We are aware that, while we were completing our paper, a similar study on the same subject has been published in Lancet with a similar study selection and similar estimate of the combined HR which was 0.79 in our study and 0.81 in the Lancet study [26]. To limit the analysis to this sole effect size can been criticized because it has been demonstrated that the hazard is not constant and is increasing in the course of time [5], therefore we also presented data on 5 and 10 years survival difference, which is more familiar to surgeons and gives support to the former effect. We nonetheless stress that these results obtained independently at different places by different persons, add validity to the statistical techniques and the results of both studies.
Supported by Ministry of University and Scientific Research (MIUR) 60% funds.




