-
PDF
- Split View
-
Views
-
Cite
Cite
N. Luciani, E. Lapenna, M. De Bonis, G.F. Possati, Mediastinitis following graft replacement of the ascending aorta: conservative approach by omental transposition, European Journal of Cardio-Thoracic Surgery, Volume 20, Issue 2, August 2001, Pages 418–420, https://doi.org/10.1016/S1010-7940(01)00789-8
Close - Share Icon Share
Abstract
A 57-year-old patient underwent prosthetic replacement of a previously implanted ascending aorta graft and developed a periprosthetic purulent collection 1 month later. He was successfully treated by debridement of infected tissues, antiseptic irrigation and transposition of an omental flap. The postoperative course was uneventful. A chest computed tomography scan performed 15 months later showed no signs of perigraft infection. Prompt conservative surgical treatment including omental transposition can be effective in the treatment of mediastinitis following graft replacement of the ascending aorta.
1 Introduction
Mediastinitis following graft replacement of the ascending aorta is a serious challenge to surgeons and is associated with a high mortality rate. If graft infection is suspected, the ideal treatment is to remove the prosthesis and to replace it with a homograft. When such a procedure seems to be too risky, a conservative approach can be attempted.
We report on a patient who incurred periprosthetic purulent collection 1 month after a redo-operation for prosthetic replacement of a previously implanted ascending aortic graft. This infection was successfully treated by intensive debridement, irrigation and omental transposition.
2 Case report
A 57-year-old man treated in 1995 by graft replacement of the ascending aorta with commissures resuspension for a type A acute aortic dissection was readmitted in November 1997 for severe aortic valve regurgitation due to prolapse of leaflets and severe left ventricular (LV) dysfunction. He underwent aortic valve replacement with a 23 mm Carbomedics mechanical valve and prosthetic replacement of the previous ascending aortic graft with a 32 mm woven Dacron tube. The postoperative course was uneventful and he was discharged 8 days after the operation. One month later, the patient complained of some drainage from the sternotomy wound and was therefore readmitted to our department. He had an increased white blood cell count, a rising temperature but negative blood cultures. A chest computed tomography (CT) scan revealed a collection localized in the anterior mediastinum all around the ascending aorta tube graft (Fig. 1) . The patient was placed on a regimen of broad-spectrum antibiotics and 2 days later he was taken to the operating theatre. Pus was found surrounding the ascending aortic graft. No anastomotic leaks, false aneurysm, graft deformity or suture rupture were present. The proximal and distal suture lines were not exposed and appeared to be completely covered by autogenous tissue. We decided to adopt a conservative strategy and to leave the prosthesis in situ. All adjacent infected and necrotic tissues were debrided. The skin incision was extended down to the umbilicus, the peritoneum was opened and the greater omentum was mobilized off the transverse colon. A segment of it was carefully isolated preserving the gastroepiploic arterial blood supply. The omental flap was then transposed into the thoracic cavity through a small tunnel created in the diaphragm and used to fill the dead space of the anterior mediastinum and to surround the ascending aorta prosthetic graft. An irrigation tube and two chest drains were inserted and the chest was closed. Local irrigation with 1% solution of polyvinylpyrrolidone-iodine was used for 2 days. Cultures from the infected tissue grew Staphylococcus haemolyticus, and therefore the patient received specific intravenous antibiotics for 3 weeks. He recovered slowly but without any complication. On the fourth postoperative week he was eventually discharged home. Chest CT scans performed 1, 3 and 15 months later showed no perigraft fluid and no signs of persistent perigraft infection. At a follow-up of 2 years the patient is doing well, with no fever, a normal white blood cell count and negative blood cultures.
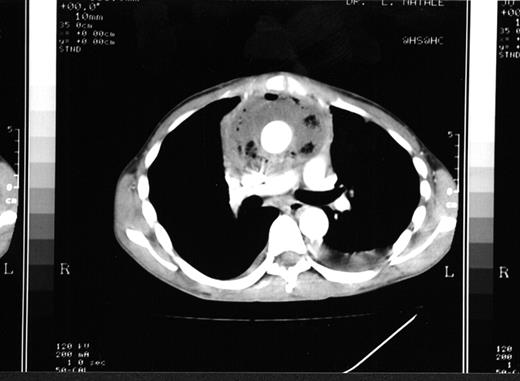
CT scan showing mediastinitis with a large periprosthetic collection surrounding the aortic prosthetic graft.
3 Comment
Infectious mediastinitis after cardiac operation is of great concern to cardiac surgeons. If an aortic graft prosthesis is present, the problem becomes even more difficult because of the high mortality rate and the difficult management of this complication. In this difficult setting every patient is a single case on its own and it is not possible to set a rule that can be followed for all of them as a group. However, once a prosthetic aortic graft becomes infected, radical excision and replacement by a homograft represents the ideal treatment. The therapeutical option of an extraanatomic bypass procedure, although widely used in the management of peripheral vascular prosthetic infections, has a limited application in surgery of the ascending aorta for evident anatomical reasons. When mediastinitis complicating prosthetic replacement of the ascending aorta is not associated with graft infection, a more conservative approach can be followed. A conservative strategy can also be attempted whenever a radical surgical treatment would be contraindicated or too risky for whatever reason.
In the case reported here we could not be sure that the graft was really colonized: indeed preoperative blood cultures were negative and, despite the huge purulent collection surrounding the aortic graft, this was functioning satisfactorily without evidence of anastomotic leak, false aneurysm, erosion or prosthetic deformity. The suture lines were not exposed and were completely covered by autogenous tissue which reduced the risk of sudden rupture. Moreover, we considered it to be highly risky to perform a radical approach involving graft resection and re-grafting in such a patient, who was already submitted twice to aortic root surgery, still recovering from the previous major surgical procedure and presenting a very depressed LV function. We therefore decided to manage this threatening complication conservatively.
The conservative approach is based on prompt reoperation, complete debridement of infected and necrotic tissues surrounding the prosthetic material and specific systemic antibiotics for some weeks. Coselli et al. [1] recommend a lifelong suppressive oral antibiotic therapy following the in situ operation. Knight et al. [2] and Kwaan and Connolly [3] suggest performing, after local debridement, a continuous antiseptic irrigation of the graft bed with polyvinylpyrrolidone-iodine solution. Other surgeons prefer using pedicled flaps of omentum or pectoral muscles to fill the dead space around the graft [1,4]. Thoracic omentoplasty in managing mediastinitis after cardiac surgery is a proven procedure [5]. However, reviewing the literature, we found that in just five patients with mediastinitis complicating replacement of the ascending aorta the prosthesis was left in situ and surrounded by a well vascularized transposed pedicled flap of the greater omentum [1,4,6]. The role of the omentum in containment of infections is well recognized [5,6] as is its neovascularization potential which leads to a higher oxygen supply to the infected area intensifying the immunologic processes and enhancing the antibiotics concentration. Moreover, the omental tissue absorbs wound secretions eliminating the substrate for bacterial growth and decreases the potential for reinfection by filling the retrosternal dead space [5]. In conclusion, mediastinitis in the presence of an ascending aorta prosthesis remains a serious, potentially lethal complication. Intensive debridement of the infected tissue, local antiseptic irrigation and omental transposition can be effective in controlling the infection. This conservative strategy can be very useful when there is no evidence of graft infection. Should a prosthesis infection be suspected, such a conservative approach can be attempted only if the risk of prosthetic resection and re-grafting seems to be too high. In this case, however, careful patient monitoring and follow-up must be adopted keeping in mind that the conservative approach is likely to be less effective than the radical one.




