-
PDF
- Split View
-
Views
-
Cite
Cite
M. Davydov, I. Stilidi, V. Bokhyan, G. Arzykulov, Surgical treatment of esophageal carcinoma complicated by fistulas, European Journal of Cardio-Thoracic Surgery, Volume 20, Issue 2, August 2001, Pages 405–408, https://doi.org/10.1016/S1010-7940(01)00796-5
Close - Share Icon Share
Abstract
Objectives: The locally advanced esophageal carcinoma can be complicated by fistulas. According to published data, the incidence rate of malignant esophageal fistulas is about 13%. The range of treatment modalities proposed by different authors varies from palliation to active and, if possible, radical surgical interventions. In the present study, we investigated combined esophagectomies as a radical treatment of the malignant esophageal fistulas. Methods: Thirty-five patients (aged 28–67) with malignant esophageal fistulas of different localizations were operated over a period from 1990 to 2000. The tumor was located in the upper, middle and lower thoracic esophagus in four, 20 and 11 cases, respectively. The malignant fistula with the mediastinum, pleural cavity, lungs, bronchi and trachea was observed in 21, two, five, four and three cases, respectively. Subtotal esophagectomy and esophagogastroplasty were performed in 18 patients; subtotal esophagectomy with intrapleural coloesophagoplasty was performed in one case; proximal gastric and lower thoracic esophageal resection from the left-side abdominothoracic approach was performed in three cases. Esophagogastric bypass anastomoses were formed in ten patients. Gastrostomy was performed in three patients. Results: The complication rate was 40% (14 out of 35); the postoperative mortality was 14.3% (five out of 35). In patients after esophageal resection, the mortality rate was 13.6% (three out of 22). With a median survival of 13 months (range, 3–31), the 2-year survival rate was 21% after combined esophagectomies. Conclusions: The goal of surgery for esophageal cancer with various fistulas is to completely resect the primary tumor and involved adjacent structures with clear surgical margins and extended two-field lymphadenectomy. The importance of performing a complete resection is stressed by the absence of 1-year survivors among patients who underwent bypass surgery or gastrostomy. We consider that en-bloc combined resection of esophageal cancer complicated by fistula can be done with a low mortality.
1 Introduction
The advanced esophageal carcinoma can be complicated by fistulas. Pathological communication between the esophagus and adjacent structures caused by the neoplastic process is also called a malignant esophageal fistula [1]. According to published data, the incidence rate of malignant esophageal fistulas is about 13% [2]. The range of treatment modalities proposed by different authors varies from palliation to active and, if possible, radical surgical interventions.
Several reports emphasize the possibility of an en-bloc resection of the esophagus and involved organs as the radical surgical treatment in order to improve the survival and quality of life [3,4].
In the present study, we investigated combined esophagectomies as a radical treatment of the malignant esophageal fistulas.
2 Materials and methods
Between 1990 and 2000, 35 patients (27 men; eight women), with a median age of 52 years (range, 28–67) underwent surgical treatment of esophageal cancer with malignant esophageal fistulas.
2.1 Preoperative assessment
Every patient had an esophagoscopy, bronchoscopy and polypositional X-ray examination. The precise location of the fistula and gastric involvement were assessed by contrast study. The obligatory diagnostic investigation consisted also of a CT scan of the thoracic organs and ultrasonography (US) abdominal investigation. The tumor was located in the upper, middle and lower thoracic esophagus in four, 20 and 11 cases, respectively. The malignant fistula of the esophagus with the mediastinum (chronic perforation of the esophagus), pleural cavity, lungs, bronchi and trachea was observed in 21, two, five, four and three cases, respectively (Table 1) .
Abscessing pneumonia as a result of aspiration pneumonia was found in ten patients, while all of the others had purulent bronchitis. All patients received intensive preoperative care.
2.2 Operative procedure
All patients underwent surgical treatment. As a rule, tumors were approached through laparotomy and right thoracotomy. Subtotal esophagectomy and esophagogastroplasty with esophagogastric anastomosis in the right hemithorax cupola (Lewis procedure) were performed in 18 patients. Subtotal esophagectomy from a laparotomic and right-side thoracotomic approach with intrapleural esophagocoloplasty was performed in one case. Proximal gastric and lower thoracic esophageal resection from the left-side abdominothoracic approach was performed in three cases. Esophagogastric bypass anastomoses were formed due to involvement of the aorta of the right auricle. Gastrostomy was performed in three patients because of a very poor respiratory function and serious cardiac pathology (Table 2) .
All of the 18 subtotal esophagectomies were combined with the en-bloc resection of the involved adjacent organs (Table 3 ; Fig. 1) . In cases of resection of the six tracheal rings, the intrathoracic circular tracheal anastomosis was formed.

An en-bloc subtotal esophagectomy and right pneumonectomy was done. The esophagogastroplasty has been performed in the right pleural cavity.
In one case, the proximal gastric and lower esophagus resection was combined with the resection of the left lower lobe, and combined with that of the right one in one more case.
Surgery with intrapleural coloesophagoplasty was combined with en-bloc right lower bilobectomy and pericardial resection.
Standard (2S) or extended two-field (2F) lymphadenectomies were done in six and 26 cases, respectively.
3 Results
3.1 Mortality and morbidity
There were five in-hospital deaths (14.3%). In patients after esophageal resection, the mortality rate was 13.6% (three out of 22). Two patients died of abscessing pneumonia (one of them had myocardial infarction) and one of empyema, mediastinitis as a result of esophagogastric anastomosis failure. After esophageal bypass surgery and gastrostomy, one patient died of bleeding of a tumor and one of pneumonia. The postoperative morbidity rate was 40% (14 out of 35). There were seven pneumonias, one myocardial infarction, four pleural empyema and mediastinitis (in one case as a result of anastomosis failure), one tumor bleeding and one wound infection.
3.2 Pathology
Sixteen patients had stage III esophageal cancer, six had stage IY according to the 1987 UICC staging system [5]. Lymph nodes were negative on surgical specimens in three patients; 19 patients had N1 disease. Six patients had metastases in intraabdominal, non-regional lymph nodes. The tumors were well differentiated squamous cell carcinoma in ten cases, poorly differentiated in eight and undifferentiated in four. The resection margins were confirmed histologically to be tumor free in all patients.
3.3 Survival
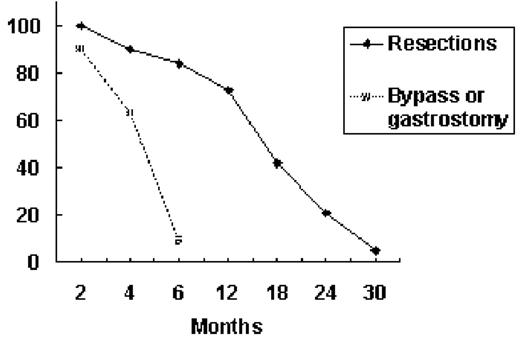
The median survival was 13 months (range, 3–31) for the resection group and 3 months (range, 1–6) for bypass and gastrostomy patients (Fig. 2) .
Sixteen patients from the resection group died due to distant metastases and had no dysphagia, and only three patients developed local recurrence. Prognostic factors for esophageal carcinoma complicated with fistulas are similar to those of other carcinomas and include the depth of esophageal wall invasion and lymph node metastases.
4 Discussion
Locally advanced esophageal carcinoma can be complicated by fistulas in about 13% of cases [2]. The treatment-related (esophageal brachytherapy and chemotherapy) esophageal fistula rate is 14% [6].
The range of treatment modalities proposed by different authors varies from palliation to active and, if possible, radical surgical interventions.
Plastic-covered metallic endoprostheses and self-expanding covered or uncovered metal stents offer effective treatment for perforations and fistulas in patients with esophageal malignancy [7–14]. Nevertheless, this procedure has some complications: stent twisting; stent migration; tumor ingrowth; tumor overgrowth; food impaction; fracture of stent wires; benign strictures at stent edges; tumor bleeding; gastrointestinal tract hemorrhage; secondary fistulas and others [9,15]. According to published data, the rate of early major complications is 17–23%; the mean survival is about 80 days [7,8,10,16].
Proponents of active surgical treatment recommend combined resections or, if this is impossible, various types of bypass operations as an alternative to gastro- and jejunostomy. Radical treatment of esophageal carcinoma complicated by fistulas is a real challenge. Zhang et al. published the results of six successful simultaneous esophagectomies with pulmonary resection of various volumes in patients with malignant esophageal fistulas [4]. Saitoh et al. successfully completed the combined surgery with post operative chemo- and radiation therapy in two patients. In 2 years, both patients were alive and free from recurrences [3].
The goal of surgery for esophageal cancer with various fistulas is to completely resect the primary tumor and involved adjacent structures with clear surgical margins and extended two-field lymphadenectomy. The importance of performing a complete resection is stressed by the absence of 1-year survivors among patients who underwent bypass surgery, gastrostomy or stent implantation. We consider that en-bloc combined resection of esophageal cancer complicated by fistulas can be done with a low mortality. This management can be recommended if the patient is in a satisfactory condition, has good respiratory, cardiac and renal function. In cases of unresectable organ involvement, a bypass procedure should be done.
References
- lung
- esophageal cancer
- pathologic fistula
- gastrostomy
- anastomosis, surgical
- bronchi
- esophageal fistula
- esophagectomy
- lymph node excision
- surgical procedures, operative
- survival rate
- survivors
- mediastinum
- mortality
- neoplasms
- palliative care
- pleura
- trachea
- lymph node dissection
- bypass
- esophageal carcinoma
- esophageal reconstruction
- surgical margins
- thoracic esophagus




