-
PDF
- Split View
-
Views
-
Cite
Cite
Dmitry Pevni, Amir Kramer, Yosef Paz, Oren Lev-Run, Chaim Locker, Menachem Matsa, Itzhak Shapira, Rephael Mohr, Composite arterial grafting with double skeletonized internal thoracic arteries, European Journal of Cardio-Thoracic Surgery, Volume 20, Issue 2, August 2001, Pages 299–304, https://doi.org/10.1016/S1010-7940(01)00832-6
Close - Share Icon Share
Abstract
Objectives: Composite arterial grafting is a surgical technique for arterial myocardial revascularization, in which free arterial conduits are proximally anastomosed end-to-side to an intact internal thoracic artery (ITA). This report describes technical aspects and results of composite grafting using bilateral skeletonized ITAs. Methods: From April 1996 to February 1999, 1057 patients underwent coronary artery bypass grafting (CABG) using bilateral skeletonized internal thoracic arteries. In 600 of them (57%), composite arterial grafting was performed. There were 452 men and 148 women. The mean age was 69±7 years. Two-hundred and six patients (34%) were diabetics, 84 (14%) had severe left ventricular dysfunction (ejection fraction of ≪35%), and 26 (4.3%) underwent emergency operations. In 574 patients, the right ITA was used as a free graft connected to the in-situ left ITA. In 26, the free left ITA was attached to the in-situ right ITA, and in 38, mini-composite grafts (free distal left ITA on the left ITA, or free distal right ITA on the right ITA) were constructed. The average number of grafts was 3.0/patient (range, 2–6). Results: The operative mortality was 2.8% (n = 17), and there were ten (1.7%), deep sternal wound infections. The mean follow-up was 25 months (range, 14–36 months). The 3-year survival was 92.5%. Ninety-seven percent of the surviving patients were angina-free. Conclusions: We currently perform this surgery routinely in most patients referred for CABG, and regard bilateral skeletonized internal thoracic arteries as the most appropriate arterial conduits for the composite technique.
1 Introduction
Several important studies published in the last few years have reported survival benefits after bilateral internal thoracic artery (ITA) grafting when compared with single ITA grafting [1–3]. In a report from the Cleveland Clinic, in addition to survival benefits, the use of bilateral ITA was associated with greater freedom from reoperation and from coronary angioplasty [1].
Until recently, the routine use of bilateral ITA was infrequent, despite excellent results and low mortality and morbidity [4–7]. The pedicled right ITA is less useful than the left ITA, as it will not always reach the right coronary artery (RCA) branches without tension, leading to its use predominantly as a free graft, with a lower patency rate when attached to the ascending aorta [8]. Another reason for cautious use of bilateral ITA was related to the increased risk of sternal wound infection [6,7].
A surgical technique was recently developed, where the ITA is dissected as a skeletonized vessel [9,10]. The skeletonized artery is isolated gently with scissors and silver clips, without the use of cauterization. The advantage is that the dissected artery is particularly long, and its spontaneous blood flow is greater than in a pedicled ITA [11,12], allowing the use of both ITAs as grafts to practically all coronary vessels requiring surgical revascularization.
Another advantage of using the skeletonized ITA is the preservation of collateral blood supply to the sternum, enabling more rapid healing, and decreasing the risk of infection [13–15].
The bilateral skeletonized ITA technique was adopted in our service as the preferred method for myocardial revascularization. The routine use of saphenous vein graft (SVG) was stopped in 1996, and vein grafts are currently used as a third optional graft (the second is the right gastroepiploic artery (RGEA)), or in emergencies, coronary artery bypass grafting (CABG).
The composite arterial grafting technique is a surgical technique whereby a free artery (usually the right ITA) is connected end-to-side to an in-situ ITA. The patency rate of the free graft in this arterial arrangement is similar to that of the in-situ ITA [16].
Between April 1996 and February 1999, 600 consecutive patients underwent CABG by means of bilateral skeletonized ITA, using the composite arterial grafting technique. In this report, we describe our results and technical experience in this subgroup of patients who received composite grafts.
2 Materials and methods
Four-hundred and fifty-two men and 148 women underwent CABG using the composite arterial grafting technique by means of bilateral skeletonized ITA. They comprised 57% of the 1057 consecutive patients who underwent CABG surgery with bilateral skeletonized ITAs during this period. The patients’ preoperative and operative characteristics are listed in Table 1 .
The mean age was 67±9 (range, 36–86) years. Severe chronic obstructive pulmonary disease (COPD) was found in 50 (8.3%), diabetes mellitus in 206 (34.3%) patients (16 insulin-dependent and 190 non-insulin-dependent). Four-hundred and sixteen patients (69%) had three-vessel and 184 (31%) had two-vessel disease.
2.1 Indications for the composite graft arrangement
We prefer the use of bilateral ITA as in-situ grafts for myocardial revascularization. The two ITAs in combination with the RGEA give us three sources of blood supply. We believe that more blood sources are associated with improved long-term outcome. The cross arrangement (right ITA to left anterior descending artery (LAD) across the midline and left ITA to circumflex marginals (Fig. 1) ) is based on the assumption that the patency rate of the right ITA on the LAD is similar to that of the left ITA on the LAD [16].
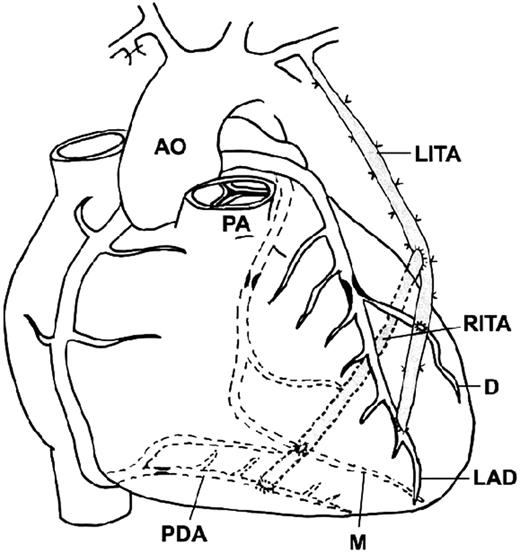
The ‘cross’ arrangement: right ITA to LAD, diagonal artery (small Y-graft) and left ITA to marginal artery.
We do not use the cross technique in cases with a short right ITA, very long ascending aorta, enlarged right ventricle, too distal or unpredictable LAD anastomotic site, and in cases with a high probability of future reoperations (for example, combined aortic valve replacement and CABG).
When the distal right ITA bifurcation cannot loosely reach the LAD, we favor the composite arterial grafting technique; we use the right ITA as a free graft, and a T-shaped [17], or if more suitable, a Y-shaped anastomosis, at the level of the main pulmonary artery is prepared, before connection to cardiopulmonary bypass (CPB; Fig. 2) .
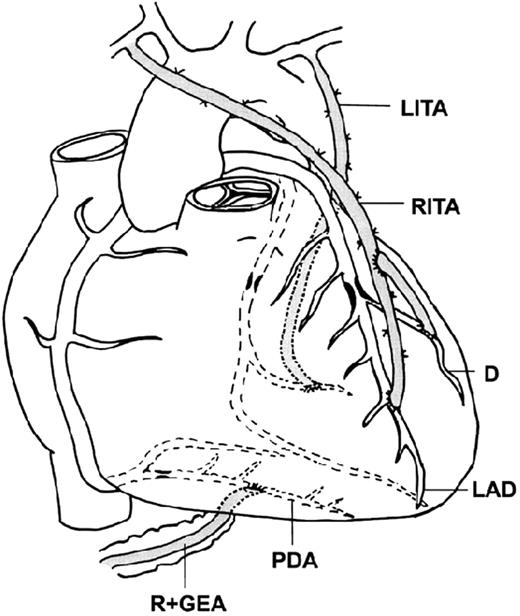
A composite graft. A free right ITA is connected end-to-side to an in-situ left ITA.
2.2 Surgical technique
The ITAs were harvested as skeletonized vessels [9,10]. Throughout the dissection, the ITA is sprayed with warm diluted papaverine solution to minimize spasm. Care is taken to keep well away from the ITA when using the cautery, even in the low setting. To obtain maximal ITA length, diameter and flow, it might be necessary to divide the internal thoracic vein to obtain satisfactory exposure of the most proximal collateral branches. Heparin is administered before distal ITA division. The skeletonized vessel is then put in a small syringe filled with 1:30 papaverine saline solution. This bath of warm papaverine is good enough to relax any spasm produced during dissection without the risk of endothelial damage caused by other antispastic maneuvers, such as intraluminary papaverine injection or mechanical dilatation.
Operations were performed with CPB. The myocardial preservation technique involved intermittent mild hypothermic cardioplegia (30–32°C).
The proximal composite anastomosis of free right ITA on the left ITA might, at times, be performed on bypass, after constructing all distal and sequential right ITA anastomoses. This is the safest way to precisely determine the location of the composite anastomosis without compromise to left ITA flow to the LAD.
2.3 Sequential grafting with skeletonized ITA
Sequential grafting is essential for complete arterial revascularization with composite grafts. Diamond-shaped side-to-side anastomosis and terminal T-shaped anastomosis for branches of the circumflex and RCA would be our preferred approach. This approach carries the advantage of sparing ITA length using the shortest possible ITA segments between anastomoses (Fig. 2).
The parallel side-to-side anastomosis is preferred for the intramyocardial coronary artery or for vessels buried inside a deep layer of epicardial fat. Constructing a diamond-shaped anastomosis in these cases exposes the ITA to the risk of seagull-wing kinking [18]. The parallel sequential technique in these situations may also be used for LAD–diagonal sequential grafting with the left ITA.
2.4 Other types of composite arrangements
To date, injury to the ITA requiring a revision of the original operative plan occurs in less than 5% of our patients, and in most, except for very few cases, the operation can still be based on both ITAs.
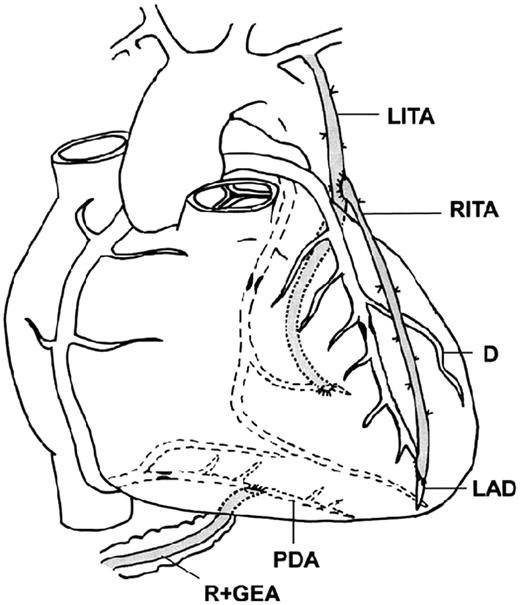
If injury is caused to the proximal right ITA, the operation can still be based on constructing a composite graft, where the free graft of the right ITA is anastomosed end-to-side to the in-situ left ITA. The operative plan is changed here only when our original plan was to use the ‘cross’ technique. However, if the proximal left ITA is injured, and can no longer be used as an in-situ graft, a reverse composite graft can then be constructed, where the free left ITA is connected end-to-side to the in-situ right ITA. This arrangement of free left ITA on in-situ right ITA can also be used when the spontaneous free flow of the left ITA is inadequate.
Despite the extra length obtained with skeletonized ITA harvesting, the left ITA may sometimes not reach the distally located anastomotic site on the LAD. In this case, a composite graft may be constructed where the in-situ left ITA is connected to a marginal branch of the circumflex, a free right ITA is anastomosed end-to-side to the left ITA, and its distal end is connected to the LAD (Fig. 3) .
Another variation of composite grafting is the small Y-graft, wherein a small distal section of an ITA is anastomosed end-to-side to a more proximal part of the same artery (Fig. 1).
2.5 Our approach to diagonal grafting
In cases which require revascularization of both the diagonal and circumflex system, the left ITA is anastomosed to the LAD, and the diagonal is one of the vessels supplied by the free right ITA (sequential grafting). When the diagonal is intramyocardial or buried deep in fat tissue, it is sometimes necessary to use the reverse Y-composite anastomosis to prevent seagull kinking [18]. In these cases, the diagonal sequential anastomosis is constructed as a parallel and not as a diamond-shaped anastomosis.
When grafts to marginal branches of the circumflex are not needed, it is possible to use the left ITA for sequential LAD–diagonal, or preferably, to use the left ITA as a small Y-graft for LAD–diagonal anastomoses.
2.6 The RCA
The ITA grafted to the RCA has a low patency rate [2,5]. Arterial anastomosis on this calcified or fibrotic vessel tends to close, and we therefore prefer the more distally located posterior descending artery (PDA) for ITA anastomosis.
It is possible to reach the PDA with a right ITA on a left ITA composite graft (Fig. 2). When no graft to the posterior wall of the heart is necessary (the circumflex region), the right ITA may also encircle the apex of the right ventricle on its course to the PDA anastomotic site.
The right ITA may not be long enough to reach the PDA. In this case, we favor the use of the RGEA as our graft of choice for the PDA. When the PDA is unsuitable for RGEA grafting, such as in cases with a potential for high competitive flow in the RCA, we prefer the SVG for revascularization of the RCA system.
To decrease the risk of spasm of the arterial grafts, all patients were treated with high-dose intravenous infusion of isosorbide dinitrate (Isoket 4–20 mg/h) during the first 24–48 h postoperatively [15]. The systolic blood pressure was maintained above 100–120 mmHg. From the second postoperative day, the patients whose gastroepiploic artery was used were treated with calcium channel blockers (Diltiazem 90–180 mg/day orally) for at least 3 months.
2.7 Statistical analysis
The data are expressed as means±standard deviation or proportions. The χ2 test and two-sample t-tests were used to compare discrete and continuous variables, respectively. Multivariate logistic regression analysis was used to predict unfavorable outcome events by various risk factors. Odds ratios (OR) and 95% confidence intervals (CI) are given. Postoperative survival is expressed by the Kaplan–Meier method. All analyses were performed by SPSS 7.5 software.
3 Results
The 600 study patients received 1–6 grafts (mean 3.0) each. The average CPB time was 84±32 min, and the aortic cross clamping time was 71±25 min.
In 574 patients, the right ITA was used as a free graft connected to the in-situ left ITA; in 26, the free left ITA was attached to the in-situ right ITA; the small Y-graft was constructed in 38 patients. The RGEA was used in 116 patients (19.3%), and vein grafts were used in 48 (8%).
The operative mortality (hospital plus 30-day postoperative mortality) was 2.8% (n = 17). The mortality of urgent and elective cases was 2.4% (14 of 574) and that of emergency operations was 11.5% (three of 26). Our definition of ‘emergency operation’ is based on STS guidelines and this included patients with ongoing angina, failed percutaneous transluminal coronary angioplasty (PTCA), acute evolving myocardial infarction, pulmonary edema and cardiogenic shock. In patients with cardiogenic shock who were not stabilized after aortic balloon counterpulsation (intra-aortic balloon pump; IABP), we usually use one ITA and vein grafts. In emergency patients who had been stabilized with IABP and were operated upon within 12 h, we harvested bilateral ITAs. Preoperative use of IABP (OR, 21.0; 95% CI, 3.82–315.42) and failed PTCA (OR, 3.65; 95% CI, 0.96–13.87) emerged as independent predictors of operative mortality. Neither gender nor age were independent predictors of operative mortality. Age was used as a continuous variable and we also arbitrarily established 70 years as our cut-off point. There were seven (1.2%) perioperative myocardial infarctions (CPK MB elevation of more than 50 mU/ml associated with new Q wave or ST–T changes), and 12 (2%) patients sustained strokes. Deep (sternal) wound infection occurred in ten (1.7%) patients. Neither diabetes (1.9%; P = 0.17) nor advanced age (≫70; 1.7%; P = 0.264) were independent predictors of untoward events. COPD (OR, 8.7; 95% CI, 2.3–32.8) and failed PTCA (OR, 4.48; 95% CI, 1.07–18.63) were independent predictors of sternal infection. Postoperative follow-up (14–36 months) was available in 571 (98%) patients by telephone survey. The 1- and 3-year survival rates (Kaplan–Meier) were 94.8 and 92.5%, respectively, only 14 of the surviving patients (2.4%) reported the return of angina. Forty-one patients underwent postoperative cardiac catheterization during the follow-up period (between 1 week and 28 months; mean, 14 months after operation), 30 because of chest pain, six had positive thallium SPECT scan, and the remainder consented to elective catheterization within the framework of learning to use the composite technique. Of the anastomoses, 103 (95.4%) were patent and five occluded (4.6%). In two of these five, technical problems were noted in the site of composite (free right ITA on in-situ left ITA) anastomosis.
4 Discussion
This study addresses the results of early and mid-term composite arterial grafting with bilateral skeletonized ITAs. The report is based on a relatively large number of patients operated upon over a short period, and focuses mainly on the technical aspects of this revascularization technique.
The ITA is currently the conduit of choice in CABG because of superior graft patency [19,20]. The right and left ITA are comparable with regard to size, flow capacity and patency [21]. However, the pedicled right ITA is less useful, as it will not routinely reach the target anastomotic sites on the right or left coronary vessels, leading to its use primarily as a free graft attached to the aorta, with a lower patency rate [8,16]. The so-called T-graft was first utilized by Mills [22] and Sauvage et al. [23]. Complete arterial revascularization was achieved in these series with two conduits, in which the right ITA is usually grafted to the in-situ left ITA and directed to the lateral and posterior aspects of the left ventricle, while the left ITA is directed to the anterior surface of the heart. Tector et al. [17] expanded the use of this technique. Dion et al. [24] demonstrated a better patency rate for free right ITAs arising as composite grafts from the in-situ left ITAs when compared with those attached to the aorta.
Our results showed that the skeletonized ITA is an ideal conduit for the composite arterial technique. The extended length obtained with skeletonization [12], and the extra length gained by constructing the proximal right ITA on the left ITA, improved the versatility of the procedure. However, despite this improved versatility, in many patients (particularly those with cardiomegaly), it seemed safer to use a third conduit (RGEA or vein graft) for revascularization of the RCA system.
During the 3-year period of our study, we never encountered ‘hypoperfusion syndrome’ (low cardiac output syndrome with temporary EKG abnormalities). This may be related to the improved spontaneous flow of the skeletonized arteries [11,25], and the excellent blood flow reserve of the proximal ITA, which is 2–3-fold larger than the flow required for complete arterial revascularization [26].
A third advantage of the skeletonized dissection is the preservation of sternal collateral blood supply. This advantage may explain the relatively low occurrence of sternal infections in the subgroups of old and diabetic patients, who are usually at increased risk of sternal wound infection when the bilateral ITAs are harvested as pedicles [6]. Our results are even more conclusive, taking into account the fact that 206 of our patients were diabetics, and 246 of them were aged 70 years or older.
In conclusion, we routinely perform complete arterial revascularization with bilateral skeletonized ITA in most of the patients referred for CABG. In our opinion, bilateral skeletonized ITAs are the most appropriate arterial conduits for the composite technique.




