-
PDF
- Split View
-
Views
-
Cite
Cite
Youichi Kawahira, Hideki Uemura, Yoshiro Yoshikawa, Toshikatsu Yagihara, Double inlet right ventricle versus other types of double or common inlet ventricle: its clinical characteristics with reference to the Fontan procedure, European Journal of Cardio-Thoracic Surgery, Volume 20, Issue 2, August 2001, Pages 228–232, https://doi.org/10.1016/S1010-7940(01)00805-3
Close - Share Icon Share
Abstract
Objective: To determine the clinical features in patients with double inlet right ventricle (DIRV) and separate atrioventricular (AV) valves in terms of the Fontan procedure. Methods: Surgical procedures were carried out in 31 patients with this rare malformation. Their clinical characteristics were compared with similar features in 45 patients with double inlet left ventricle (DILV), 93 with common inlet right ventricle (CIRV), and 20 with common inlet left ventricle (CILV). Results: Pulmonary atresia with the right and the left pulmonary arteries being confluent was seen in 58% of patients with DIRV, and pulmonary atresia with non-confluent pulmonary arteries in 15% (P = 0.0001). The incidence of these findings was significantly higher when compared with DILV (P = 0.0001). Reflecting these morphologic features, constructions of systemic-to-pulmonary shunts and extensive plasty to the pulmonary arteries were more frequently needed in patients with DIRV than in the others (P = 0.04, 0.0001). The AV valves have become moderately or severely regurgitant in three with DIRV (10%). The Fontan procedure has thus been employed in 21 with DIRV (64%), this incidence being significantly higher than that seen in the CIRV (37%) group (P = 0.01). Survival rate of 95% at 10 years in this group was as excellent as that in the DILV group, and obviously better than that in either CIRV or CILV (P = 0.002). Conclusions: Although multiple palliative procedures might be frequently needed to maintain pulmonary perfusion, the Fontan circulation can be justifiably established in patients with DIRV, and regurgitation across the AV valves was not very common.
1 Introduction
Double inlet atrioventricular (AV) connection to the morphologically right ventricle through separate AV valves (DIRV) is known to be a rare cardiac malformation [1–5]. Although the Fontan procedure has been increasingly employed in patients with univentricular AV connection, this morphologic subset has not been precisely focused on, in terms of establishment of the Fontan circulation. Our present investigation is, therefore, carried out to determine clinical features in patients with this unusual AV connection, particularly in the light of morphologic characteristics and their surgical implications.
2 Patients and methods
Between April 1978 and September 2000, 189 patients with double or common inlet ventricle [6] underwent some surgical interventions, either definitive repair (in 106) or palliative procedures (in 83) at our institute. Those with absent left or right AV connection were excluded. Of these, 31 patients (16%) possessed DIRV with a rudimentary and incomplete left ventricle, while double inlet left ventricle (DILV), common inlet right ventricle (CIRV), and common inlet left ventricle (CILV) were seen in 45 (24%), 93 (49%), and 20 patients (10%), respectively. Atrial arrangement, ventriculoarterial connections, and other morphologic features, were determined in this clinical series of patients by preoperative cardiac imaging as well as intraoperative inspection. The diameter of the AV valves and regurgitation across the valve were also determined on ventriculography. Clinical features were compared between the groups of patients with DIRV and other subsets of the AV connection.
The Fontan circulation was established by atriopulmonary connection in 11 patients before 1987. Between 1987 and 1996, total cavopulmonary connection was employed by the construction of an intraatrial channel in 44, the sinus node being placed within the low-pressured atrial chamber [7]. Since 1996, the extra-cardiac Fontan procedure has been our preference to establish total cavopulmonary connection [8], this operative option also making the sinus node sit within the low-pressured atrial chamber. This procedure was chosen for the remaining 28 patients.
A set of measured values were described by their average and standard deviation. The chi-square test or Fisher's exact test was used to analyze proportional values and the steel test was additionally used as a multiple comparison. Analysis of variance with Fisher's PLSD test was used to compare the parametric values. For the analysis of survival, the Kaplan–Meier method and the log-rank test were employed.
3 Results
3.1 Morphologic features
Visceral heterotaxy was less common in patients with DIRV when compared to those having common inlet AV connection (P = 0.0001) (Table 1 ). Ventricular orientation was of d-loop pattern in 68% of DIRV and in 40% of DILV, while it was of l-loop pattern in 32% of DIRV and in 60% of DILV. There was a statistical difference between these two groups (P = 0.017). Reflecting differences in ventriculoarterial connections between the four groups, findings of pulmonary atresia, as well as the non-confluent pulmonary arteries, were more frequent in those with DIRV than in those with DILV (P = 0.0008, 0.03) (Table 1).
Morphologic findings in 189 patients with double inlet or common inlet ventriclea
3.2 Palliative surgical procedures
Intimately related to the morphologic features of the pulmonary pathway, palliative surgical procedures were more frequently needed in the group of patients with DIRV when compared with other morphologic features (P = 0.0003) (Table 2 ). Construction of systemic-to-pulmonary shunts, particularly bilateral or multiple procedures, was common in those with DIRV (P = 0.0001), and the number of shunts was significantly greater in DIRV than in CIRV (1.2±1.0 versus 0.6±0.7 times) (P = 0.0001). Extensive plasty to the pulmonary arterial tree was also more frequently needed in this setting (P = 0.0001). The number of such procedures was significantly greater in patients with DIRV (0.8±0.9 times) than in those with DILV (0.2±0.4 times), those with CIRV (0.1±0.2 times), and those with CILV (0.2±0.4 times) (P = 0.0001). The overall number of palliative procedures onto the pulmonary arteries was greater in DIRV (2.1±1.3 times) than in DILV (1.3±0.8 times), CIRV (0.9±0.8 times), and CILV (1.1±1.1 times) so as to establish an efficient pulmonary circulation prior to the Fontan procedure. Banding of the pulmonary trunk was needed in five having DIRV with mild pulmonary stenosis (Table 2). Reconstruction of the obstructed aortic arch was needed in two with DIRV. Both of these had the feature of double outlet right ventricle, and subaortic stenosis was obvious. The Damus anastomosis was carried out concomitantly with the bidirectional Glenn procedure, which was followed by the staged establishment of the Fontan circulation with complete success except in one. The presence of totally anomalous pulmonary venous connection was not uncommon in the setting of CIRV and CILV, most likely related to visceral heterotaxy, but was rare in patients with DIRV (P = 0.02) (Table 2).
3.3 Clinical features of the AV valves
Catheterization prior to the Fontan procedure demonstrated that the right-sided AV valve was regurgitant in three with DIRV (10%). The orifice of the valve was closed at the time of the Fontan procedure. Preoperative AV regurgitation in this setting was not as frequently seen as in those with common inlet ventricle (Table 3 ). In another patient, regurgitation progressed after the Fontan procedure. Reoperation was eventually carried out 8 years after the initial Fontan procedure, for closure of the right-sided orifice and plasty to the left-sided valve.
Regurgitation across the AV valves and establishment of the Fontan procedurea
On ventriculography prior to the Fontan procedure, orificial diameter of the right-sided AV valve was 77±26% of the anticipated normal value for the tricuspid valve [9]. That of the left-sided one was 96±22% of the anticipated normal value for the mitral valve (Fig. 1 ). In the three patients undergoing closure of the regurgitant right-sided valve, orificial size of the left-sided valve was considered to be sufficiently large for supporting the systemic circulation.
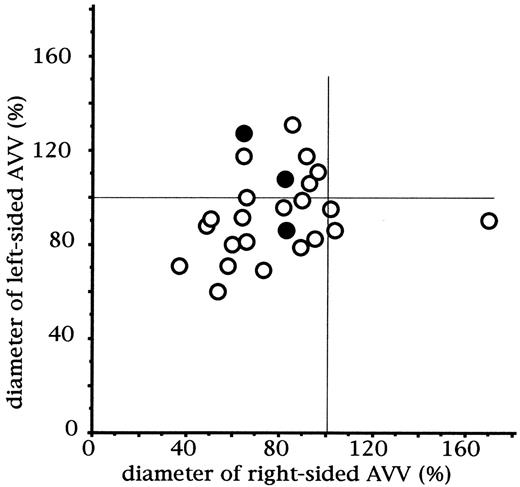
Diameter of the right-sided and the left-sided AV valves in patients with DIRV. Measurement was carried out on ventriculography prior to the Fontan procedure and standardized by the anticipated normal value. The black dots indicate values derived from patients having moderate or severe regurgitation across the right-sided AV valve. AVV, atrioventricular valve.
3.4 Establishment of the Fontan procedure
Of 31 patients with DIRV, 21 (65%) have undergone the Fontan procedure so far. Atriopulmonary connection was employed in four, and total cavopulmonary connection in 17. Types of the Fontan procedure did not differ between the four groups (P = 0.08) (Table 3). The Fontan procedure was carried out at the age of 5.7±3.1 years in DIRV with no significant differences from DILV (5.0±4.0 years), CIRV (5.1±3.9 years), and CILV (5.5±3.7 years) (P = 0.93). Another two patients are currently candidates waiting for the Fontan procedure. The rate of the Fontan completion at present does not differ between the four groups except for CIRV, the subset appearing as an unfavorable group (P = 0.01) (Table 3).
Survival rate after the Fontan procedure in DIRV was almost as excellent as that in DILV, 95% at 10 years (Fig. 2 ). Survival rates in DIRV and DILV were statistically higher than those in CIRV and CILV (P = 0.002). Cause of early death in one with DIRV was mediastinitis. No episode of arrhythmia has been noted subsequent to the Fontan procedure in patients with DIRV.
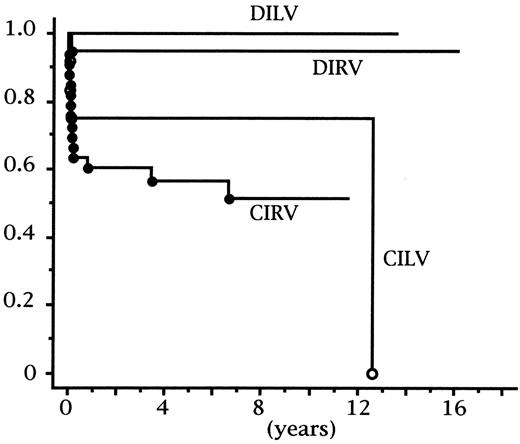
Actuarial survival rate after the Fontan procedure. Survival rate at 10 years was 95% in patients with DIRV, 100% in those with DILV, 75% in those with CILV, and 51% in those with CIRV. Statistical difference was noted between these groups by the log-rank test (P = 0.002). DIRV, double inlet right ventricle; DILV, double inlet left ventricle; CIRV, common inlet right ventricle; CILV, common inlet left ventricle.
On catheterization 1 year after the Fontan procedure, cardiac index was calculated as 2.3±0.3 l/min/m2 in DIRV, which did not significantly differ from that in DILV (2.8±0.5 l/min/m2), CIRV (2.6±0.6 l/min/m2), and CILV (2.5±0.8 l/min/m2) (P = 0.67).
4 Discussion
Among hearts with univentricular AV connection, the morphologically left ventricular type is the most frequent [10], is the easiest to diagnose angiographically [11,12], and, from the surgical viewpoint, is most amenable to definitive repair [13,14]. DIRV, defined as ventricular morphology in which both atria empty, entirely or predominantly into the morphologically right ventricle [6], has been reported to be relatively rare [10,15]. Although some angiographic findings have been reported [16], they do not clearly illustrate its clinical significance for the Fontan operation, for example, in a view of function of the AV valve, growth of the pulmonary arteries, and ventricular function.
DIRV has been reported to be rare, being found in less than 5% of the series of patients reported [10,15,17]. Shiraishi and Silverman [2] reported DIRV in one patient (2%) of 50 patients with double inlet or common inlet ventricle. In another report from the East, Wang et al. [3] reported that the incidence of patients with a dominant morphologically right ventricle in the Chinese population was much higher than that reported in the West, and that both atria were connected to the dominant right ventricle in 60% of all patients with double or common inlet ventricle. Surprisingly, however, only one patient of their series (1.7%) possessed separate AV valves. In our clinical series, encounter with DIRV was much more frequent than previously reported in the East as well as in the West. This might be partly because of the difference in the nature of the cohort of materials; that is, hearts within the living patients and the post mortem specimens.
As for the ventricular topology in hearts with DIRV, it has been reported that the rudimentary and incomplete morphologically left ventricle was usually located left-posteriorly to the dominant morphologic right ventricle (d-loop). It has been reported also that double outlet right ventricle is the commonest ventriculoarterial connection in DIRV [18]. In our current series, solitary outlet of the aorta from the dominant right ventricle was common, and ventricular l-loop was not extremely rare.
Apart from such inconsistencies in the morphologic aspect, precise recognition of pulmonary arterial anatomy proved to be of clinical importance in the DIRV. Although its embryological background remains unknown, multiple procedures, either surgical or interventional, might be needed, anyway, as preparations aiming toward the non-cyanotic Fontan circulation. It was not hopeless at all to find that with appropriate previous palliative procedures, achievement of the Fontan procedure can be quite successful, its results being better than expected in the short and the long term. Since the separate AV valves in DIRV did not become regurgitant frequently even with the construction of multiple shunts, the dominant ventricle would be able to tolerate the volume load produced by an increase of pulmonary blood flow.
This circumstance is obviously different from that of patients with common inlet ventricle in the setting of visceral heterotaxy. The common AV valve guarding univentricular AV connection unequivocally possesses the underlying structural features intimately related to the regurgitation across the valve [19,20]. Such morphologic abnormalities, particularly abnormal structures of the papillary muscles and tendinous cords can have a deleterious impact on the ventricular function. In this respect, hearts with DIRV may have an advantage over those with CIRV, since there are two AV valves present and the architecture of the valves and their tension apparatus can be functionally less fragile compared to similar features of the CIRV. To determine this hypothesis, more precise morphologic investigation, as well as more detailed functional evaluation in clinical patients, is needed. When ventricular function is to be compared between groups of patients with the dominant left and right ventricle, it should be reminded that the ejection fraction of the ventricle is greater in patients with the dominant left ventricle than in those with the dominant right ventricle [7].
In conclusion, although multiple palliative procedures might be needed frequently for maintaining pulmonary perfusion, the Fontan circulation could be justifiably established in patients with DIRV, and regurgitation across the AV valves was not as common as seen in the setting of common inlet ventricle.
Dr W. Daenen (Leuven, Belgium): Can I ask you, what was the incidence of fenestrations in these patients? Was it high or was it routinely used?
Dr Kawahira: In a few patients fenestrated Fontan was carried out.
Dr Daenen: Only a few?
Dr Kawahira: Yes.




