-
PDF
- Split View
-
Views
-
Cite
Cite
Angela Montijano, Salvador Espinosa, José M. Melero, Miguel Such, Delayed mitral regurgitation following transmyocardial revascularization with CO2 laser, European Journal of Cardio-Thoracic Surgery, Volume 18, Issue 4, October 2000, Pages 498–499, https://doi.org/10.1016/S1010-7940(00)00546-7
Close - Share Icon Share
Transmyocardial laser revascularization is a controversial surgery for the treatment of advanced coronary disease aimed at improving myocardial perfusion and palliating the level of angina, with promising clinical results and low risks [1–3]. It is not an alternative to direct procedures, as the definitive mode of action has not been established yet [1,4]. In-hospital mitral regurgitation (MR) has been described [2], but a delayed clinical presentation has never been reported. We found a post-discharge MR possibly linked to this procedure. The objective of this letter is to draw attention to this rare circumstance.
A 59-year-old woman was diagnosed of coronary artery disease and treated with percutaneous angioplasty to the LCx artery. Three years later the angina recurred. The treadmill exercise-tolerance testing was positive and the thallium-201 scintigraphy revealed reversible defects in the anterior, septal and lateral walls. The cardiac catheterization showed an occluded LAD artery, a vessel smaller than 1 mm diameter, with poor distal bed only visible through collateral flow. The LCx was not restenotic, while the RCA looked ectasic without stenosis. The ventricular function was normal, and the mitral valve, competent. Symptoms were attributed to the evidenced ischemic areas. CABG to the LAD was rejected due to the disfavourable anatomy, and transmyocardial laser revascularization with CO2 was performed using transesophageal echocardiographic monitoring, drilling 29 effective channels in the anterior and lateral walls. The patient was discharged on the seventh postoperative day. She needed readmission 1 month later because of sudden pulmonary edema without angina. A systolic murmur was then detected and the echocardiography made a severe MR evident due to a broken chordae, together with normal ventricular motion, non-dilated mitral annulus and non-enlarged left atrium. As the clinical course was acute and very badly tolerated, an emergency intervention became necessary. A ruptured mitral chordae was detected intraoperatively whereas the papillary muscle was intact (Fig. 1) . Mitral replacement was performed in an attempt to correct the problem efficiently and to reduce the myocardial ischemic time. A Carbomedics 25-mm mechanical prosthesis (Carbomedics Inc, Austin, TX) was implanted keeping the native valve in place. From that moment onwards, the patient was asymptomatic after 10 months of follow-up.
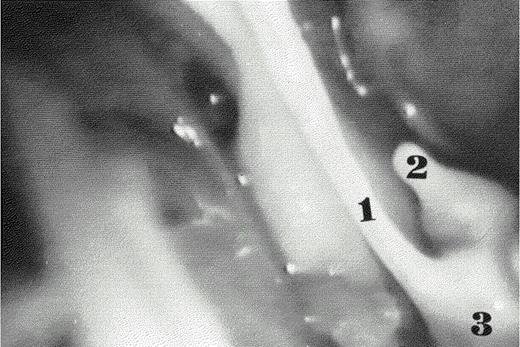
A ruptured primary mitral chordae was detected during the operation by means of a 10-mm Storz endoscope (Karl Storz, Tuttlinger, Germany). (1) Chordae tendina ad integrum. (2) Ruptured mitral chordae tendina. (3) Posterior papillary muscle.
Few data have been reported about potential risks or predictor factors of cardiac events after transmyocardial laser revascularization [3]. Accidental laserhit on valvular structures is remote because laser lacks enough power to drill a channel to such distal targets or it is very small, about 1 mm, to be relevant [5]. In our case, differing from other cases reported, MR appeared after discharge. Nevertheless, it is possibly linked to the intervention. One explanation is that during the operation, the laser pulse effect on the anterior wall, could have partially damaged the mitral chordae which got completely ruptured later on, determining an acute severe MR. Echocardiographic findings appeared later, simultaneously with symptoms, and they suggested a traumatic cause. Indeed, this surgery theoretically does not infarct the treated regions [1] and there were no data suggesting a perioperative infarction to explain an ischemic MR.




