-
PDF
- Split View
-
Views
-
Cite
Cite
Domenico Paparella, Stefano Schena, Luigi de Luca Tupputi Schinosa, Nicola Vitale, One step surgical repair of type II acute aortic dissection and aortic coarctation, European Journal of Cardio-Thoracic Surgery, Volume 16, Issue 5, November 1999, Pages 584–586, https://doi.org/10.1016/S1010-7940(99)00286-9
Close - Share Icon Share
Abstract
It is presented the case of acute type II aortic dissection in a patient with aneurysmal ascending aorta, hypoplastic arch and isthmic coarctation. One single step replacement of the ascending aorta, arch and the isthmus was performed by ensuring simultaneous optimal perfusion above and below the coarctation through the femoral and subclavian artery.
1 Introduction
Rupture of the aorta or a dissecting aneurysm is a life-threatening complication of aortic coarctation [1]. This combined disorder has been identified as one of most frequent vascular malformations associated with Turner's syndrome [2]. The aortic tissue adjacent to the coarctation presents histologic features of cystic medial necrosis similar to those of Marfan's syndrome [3].
This combined condition is usually treated by two-step surgery. The first step involves emergency repair of the aortic dissection. Subsequently, coarctation repair is undertaken at a later date [4,5]. When a combined procedure is undertaken, providing adequate blood flow on cardio-pulmonary bypass (CPB) to both upper and lower body can be difficult. This is because, when the gradient across the coarctation is high, femoral artery cannulation can deliver adequate blood flow only to the lower torso, and not to the upper torso proximal to the coarctation of the aorta. Similarly, establishing CPB with cannulation of the distal arch in patients with coarctation may result in inadequate blood flow to the lower torso.
We present a technique that permits one-step replacement of the ascending aorta, arch and the isthmic coarctation and addresses the problem of CPB management.
2 Case report
A 14-year-old boy was referred to our unit for dizziness and the sudden onset of retrosternal, constrictive pain while playing soccer. On clinical examination, carotid and radial pulses were present whereas femoral pulses were absent. A 3/6 systolic murmur was heard in the aortic area. Blood pressure in the right arm was 200/110 mmHg and 150/90 mmHg in the left arm. A chest radiograph showed rib notching and reverse three sign. A computerised tomogram of the chest revealed an aneurysm of the ascending aorta with an intimal flap, normal aortic arch, and a coarctation of the aortic isthmus (Fig. 1) . Transthoracic echocardiogram confirmed the presence of a dissected aneurysm of the ascending aorta, mild aortic valve incompetence, and pericardial effusion. The diameter of the ascending aorta was 7.5 cm. At aortography, the intimal tear was visualised 2 cm above the aortic valve. The intimal flap extended up to the origin of the innominate artery. The aortic arch appeared to be hypoplastic, and the coarctation of the isthmus was again demonstrated. A gradient of 60 mmHg was measured across the coarctation.
Spiral angio C.T. scan (multiplanar reconstruction). Note the aortic aneurysm, intimal flap, hypoplastic arch and isthmic coarctation.
The patient underwent emergency surgery. He was positioned on the table in supine position with moderate rotation of the left side of his chest. The left common femoral artery was isolated and median sternotomy was performed. Two arterial cannulae were placed, one in the left subclavian and the other one in the left common femoral artery. The pericardium was then opened and 900 ml of fresh blood drained. In order to improve the surgical exposure of the coarctation, a left thoracotomy was carried out at the fourth intercostal space that was then joined to the sternotomy. The right atrium was cannulated and CPB initiated by perfusing simultaneously the lower torso through the femoral cannula while the head and arms were perfused through the cannula in the left subclavian artery. The two arterial lines were joined by means of a y connection. Cross-clamps were then placed proximally and distally to the coarctation, and the patient was cooled slowly. The coarctation was resected, and a 22-mm collagen coated polyester vascular prosthesis (InterVascular, La Ciatat, France) was anastomosed distally to the descending aorta. Once the temperature had reached 18°C, the ascending aorta was clamped below the innominate artery, opened and blood cardioplegia was infused in the coronary ostia. Cardiopulmonary by-pass was then interrupted and cerebral retrograde perfusion was started at the usual flow of 250–300 ml/min through a superior vena cava cannula, maintaining a central venous pressure of 14 mmHg. The aortic arch was inspected. Although it did not appear dissected, it was found to be hypoplastic, so its replacement was thought necessary. The neck vessels were not dissected. A cuff of aortic wall around the origin of the head vessels was trimmed and then anastomosed to the conduit with a continuous 5/0 prolene suture. The graft was then clamped proximally to the innominate artery and deaired. At this stage CPB was restarted only through the femoral cannula. The other arterial cannula was removed from the left subclavian artery. During rewarming, after the aortic valve had been repaired by resuspending the cusps with a 5/0 prolene suture, the conduit was anastomosed to the aorta 1 cm above the valve with a 4/0 prolene suture (Fig. 2) .
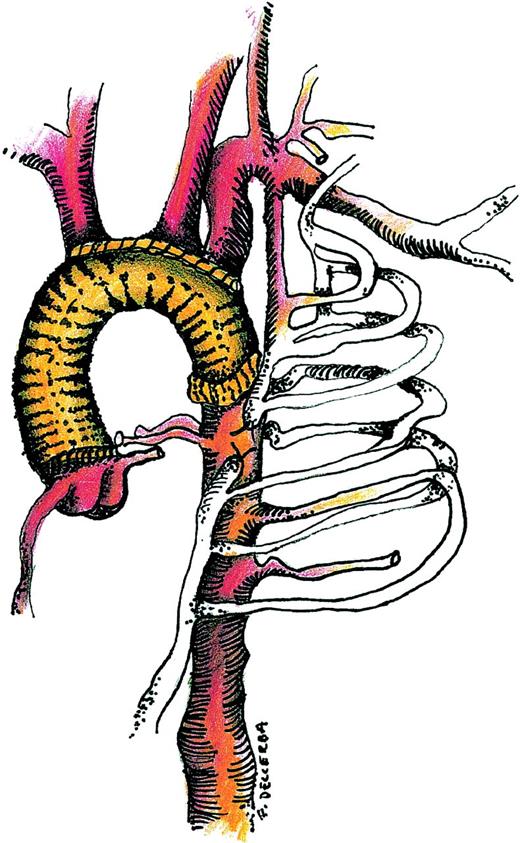
Combined replacement of the ascending aorta, arch and isthmic coarctation.
At the end of the procedure the patient was easily weaned off CPB; CPB, myocardial ischaemic and circulatory arrest times were 200, 110 and 25 min, respectively.
The patient was extubated the next morning. Intensive care unit stay was 4 days. No cerebral, respiratory or renal complications occurred. The remaining postoperative stay was also uneventful. The patient was discharged home on the 15th postoperative day on anti-hypertensive medications.
At 12 months follow-up, he was free of complications and in NYHA functional class I. Trans-esophageal echocardiogram revealed trivial aortic regurgitation, good function of the aortic graft, and no distal dissection.
3 Comment
A combined approach to the replacement of an ascending aortic aneurysm, arch and coarctation in the presence of acute aortic dissection has been previously reported by Svensson [7]. He excluded the coarctation using two conduits in a single stage procedure [7]. Co-existing aortic dissection and coarctation have been addressed in various ways by other authors [4–6]. None of these reports contained cases involving a hypoplastic arch. Staged procedures using proximal or distal perfusion alone with subsequent coarctation repair at 2 months have been described [4–6]. None of these reports contained cases involving a hypoplastic arch [4–6].
Our technique facilitates single-stage repair by maintaining adequate perfusion above and below the coarctation. Access to the entire aorta from the aortic root to the upper part of the descending aorta, arterial and venous access, conduct of CPB, and retrograde cerebral perfusion are the major considerations in planning this procedure. Each of these components have been addressed in the context of other aortic conditions.
The use of extended median sternotomy, antero-lateral thoracotomy and groin incision was found to be satisfactory in this case. Otherwise extended thoracotomy with a transverse sternotomy incision could have been employed.
Because of a 60 mmHg gradient across the coarctation, the management of CPB involved placing two arterial lines. This allowed for the maintenance of adequate flow to both areas of the body.
Repair of acute aortic dissection takes precedence over coarctation repair. A two-stage procedure may be suboptimal because following dissection repair, left ventricular afterload remains elevated and persistent hypertension increases the risk of aortic complications relating to the repair and the remaining coarctation. Furthermore, in our patient the graft distal anastomosis had to be performed beyond the coarctation due to hypoplasia of the arch.
In conclusion, we believe an adequate surgical exposure and this combined approach of using a simultaneous perfusion of lower and upper body appear to be a safe and useful technique for patients presenting with aortic dissection and coarctation.




