-
PDF
- Split View
-
Views
-
Cite
Cite
Gian Luca Martinelli, Mauro Cassese, Giovanni Speziali, Alessandro Testa, Marco Lirici, Mario Bobbio, Maurizio Braccio, Marco Diena, Myocardial revascularization through a mini-thoracotomy with thoracoscopic assistance, European Journal of Cardio-Thoracic Surgery, Volume 14, Issue Supplement_1, October 1998, Pages S68–S70, https://doi.org/10.1016/S1010-7940(98)00108-0
Close - Share Icon Share
Abstract
Objective: Left internal mammary artery harvesting through a mini-thoracotomy makes gaining the proximal portion of this vessel very difficult and exposes the patient to the risk of chest wall trauma due to excessive spreading of the ribs. The adoption of video thoracoscopic assistance can give several advantages to the procedure. Methods: With the patient in a 30° left-side-up thoracotomy position, a 8–12 cm anterior thoracotomy is performed in the left fourth or fifth intercostal space. Two thoracoscopic ports are inserted in the third and fourth left intercostal spaces in the midaxillary line. Complete mobilization of the left internal mammary artery is performed with a mixed surgical and thoracoscopic technique. Results: Since July 1996, 12 patients underwent myocardial revascularization with the left internal mammary artery through a mini-thoracotomy, with the aid of video assisted thoracoscopy. There were no deaths or perioperative infarctions. Mean hospital stay was 4 days (3–6). In nine patients a postoperative angiographic study was performed: in all cases the length of the mammary artery pedicle was adequate; one patient underwent a successful angioplasty on a narrowed anastomosis on the left anterior descending artery. In another patient the left internal mammary artery had been grafted to a diagonal branch. In all other cases angiography showed good results. Conclusions: Thoracoscopic assistance helps achieving complete mobilization of the left internal mammary artery, maximizing its useful length, without an extended thoracotomy.
1 Material and methods
Since July 1996, 658 patients underwent coronary artery surgery at our institution. Of these, 45 patients with proximal, isolated left anterior descending coronary artery (LAD) lesions received a single bypass graft (left internal mammary artery (LIMA) to (LAD)). Twenty-three patients were operated on through a median sternotomy with cardiopulmonary bypass while 22 patients had beating-heart surgery. Ten of these last 22 patients had a median sternotomy, while twelve patients, ten males and two females (age 48–74 years, mean 57.8 years) underwent myocardial revascularization with the LIMA through a mini-thoracotomy with the help of video-assisted thoracoscopy. Four patients had a previous percutaneous transluminal coronary angioplasty to the LAD. Although this type of procedure has gained tremendous popularity in the last few years [1–3], we limit our current indications to a selected population of patients showing:
presence of a proximal, isolated LAD lesion not suitable for PTCA;
adequate characteristics of the proposed target vessel on preoperative angiogram;
adequate body habitus (no obese patients);
presence of contraindication(s) to cardiopulmonary bypass;
particular cosmetic needs.
2 Technique
After orotracheal intubation with a double-lumen tube, the patient is positioned in a 30° left-side-up anterior thoracotomy position. A left anterior thoracotomy is performed in the fourth or fifth intercostal space and harvesting of the mammary artery is initiated from the distal end under direct vision. The left lung is excluded from ventilation and allowed to collapse. A retractor/stabilizer (CTS, CardioThoracic Systems, Cupertino, CA) is utilized to improve exposure. Two thoracoscopic ports are created in the third and fourth intercostal space on the anterior axillary line. One of these ports allows introduction of a rigid camera instrument (Karl Storz Endoskope, Tuttlingen, Germany), while the other is used for introduction of an electric cautery or endoscopic forceps. Dissection and mobilization of the LIMA to its origin is then continued using a mixed technique: the distal third of the mammary artery is harvested under direct vision through the thoracotomic incision, while the proximal two-thirds are mobilized with a fully thoracoscopic technique [4, 5]. We have harvested the mammary artery both as a pedicled and as a skeletonized vessel.
The pericardium is opened and its edges suspended to the chest wall. The LAD is exposed and the intended anastomotic site is identified.. After systemic heparinization (1.5 mg/kg), the mammary artery is transected and the blood flow is checked.
The anastomosis is performed under both direct and thoracoscopic visualization using a continuous 7-0 Prolene suture. The stabilizing arm of the CTS retractor is used to provide field stability with the help of a looping suture around the LAD proximal to the anastomotic site (Fig. 1) [6].
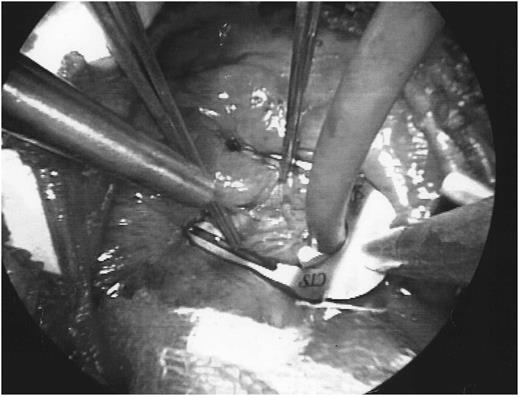
The stabilizing arm of the retractor (CardioThoracic Systems) is used to provide field stability with the help of a looping suture around the LAD proximal to the anastomotic site.
Heart rate control with farmacologic agents is not routinely used. A 14-gauge angiocath, connected to an oxygen supply (3–5 l/min) is used as a blower to keep the field dry. After hemostasis has been checked through the fiber optic camera, one or two left pleural chest tubes are inserted through the thoracoscopy incisions; The lung is re-expanded, a catheter for intrapleural analgesia is positioned and the chest is closed in the usual manner.
3 Results
We had no mortality or perioperative infarction. Mean coronary occlusion time was 11 min (range 7–18 min). No patient developed any sign or symptom of neurological injury (either transient or permanent). One patient underwent re-exploration for bleeding from a side branch of the LIMA, while another patient had to be switched to a median sternotomy with cardiopulmonary bypass for hemodynamic instability. Mean hospital stay was 4 days (range 3–6 days). Nine patients had a 1-month postoperative angiographic study. One patient underwent successful angioplasty of a narrowed LIMA–LAD anastomosis, in another case the LIMA had been sewn to a diagonal branch of the LAD. This patient was asymptomatic, and he was discharged after a negative exercise test. In all other cases angiography showed a good result with adequate length of the mammary artery pedicle (Fig. 2). Two more patients are awaiting for the postoperative study to be performed.
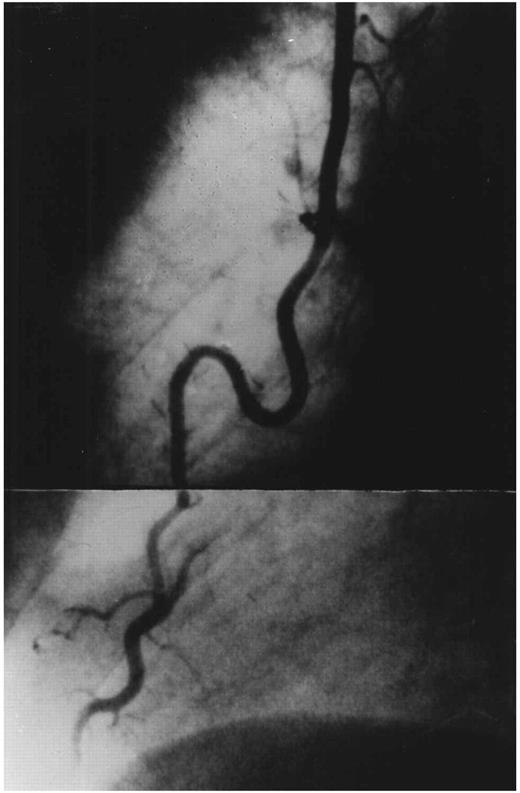
Routine postoperative coronary angiogram showing a patent left internal mammary artery to left anterior descending coronary artery anastomosis and adequate length of the mammary artery pedicle.
4 Discussion
We believe that thoracoscopic assistance during thoracotomic procedures carries several advantages. It provides the means to obtain complete mobilization of the LIMA, avoiding excessive spreading of the ribs, reducing chest wall trauma and preventing rib fracture and chondrocostal disjunction. It also makes it possible to accurately check hemostasis throughout the mammary artery bed.
Since the experience reported in the present article, our team has performed 11 other minimally invasive bypass graft cases; in four of these, the LIMA was completely harvested under thoracoscopic vision with the closed chest technique described by Nataf and colleagues [4].
Currently we first introduce the thoracoscope in the patient's chest; if LIMA visualization is satisfactory, harvesting is performed thoracoscopically, otherwise we use the combined technique described above.
As far as the indications for this type of surgical procedure, we think that only in a small number of cases it is the best procedure for the patient. The learning curve effect with the related morbidity must be overcome to render minimally invasive coronary revascularization competitive with the standard alternative on a larger number of candidates.
References
- angiogram
- coronary revascularization
- internal thoracic artery
- anterior descending branch of left coronary artery
- anastomosis, surgical
- angioplasty
- infarction
- mammary arteries
- ribs
- surgical procedures, operative
- thoracoscopy
- thoracotomy
- minithoracotomy
- chest wall injuries
- pedicle
- anterior thoracotomy
- intercostal space
- video assisted thoracoscopy




