-
PDF
- Split View
-
Views
-
Cite
Cite
Shanhu Qiu, Xue Cai, Lijing Jia, Zilin Sun, Tongzhi Wu, Janine Wendt, Jürgen Michael Steinacker, Uwe Schumann, Does objectively measured light-intensity physical activity reduce the risk of cardiovascular mortality? A meta-analysis, European Heart Journal - Quality of Care and Clinical Outcomes, Volume 7, Issue 5, November 2021, Pages 496–504, https://doi.org/10.1093/ehjqcco/qcaa051
Close - Share Icon Share
Abstract
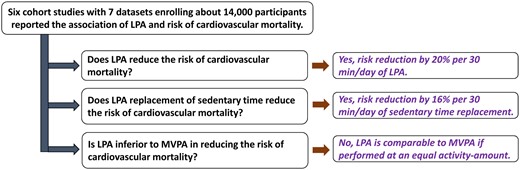
Current physical activity guidelines emphasize little on light-intensity physical activity (LPA) in terms of reducing the risk of cardiovascular mortality. This meta-analysis aimed to bridge this gap by assessing their association using objectively measured LPA data.
Databases of PubMed and Scopus were searched to April 2020 for prospective cohort studies that reported the association of LPA assessed by activity monitors with the risk of cardiovascular mortality in the general population. Multivariable-adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) were pooled using a random-effects model. Dose–response and subgroup analyses were also performed. Six cohort studies with seven datasets enrolling 13 960 participants were included. LPA was all measured by accelerometers. The HR of LPA per 30 min/day for cardiovascular mortality was pooled to be 0.80 (95% CI 0.67–0.96). This association was non-linearly shaped (Pnonlinearity < 0.01) and unaffected by sex difference. Moreover, substituting LPA for sedentary time of 30 min/day lowered the risk of cardiovascular mortality by 16% (95% CI 0.73–0.96). Results showed further that LPA was inferior to moderate-to-vigorous physical activity in reducing the risk of cardiovascular mortality when performed with an equal time-length set at 30 min/day (HR 0.83 vs. 0.54, Pcomparison = 0.046), but became comparable if at an equal activity-amount set at 150 metabolic equivalents-min/day (HR 0.67 vs. 0.54, Pcomparison = 0.41).
LPA shows potential in reducing the risk of cardiovascular mortality, and interventions targeting at LPA improvement are worth being encouraged.
Introduction
Physical inactivity is now considered the fourth leading cause of death, resulting in a substantial economic burden worldwide.1,2 Current guidelines have recommended undertaking ≥150 min/week of moderate-to-vigorous physical activity (MVPA) or ≥75 min/week of vigorous-intensity physical activity (VPA) to gain cardiovascular benefits, such as to reduce the risk of cardiovascular mortality.3,4 However, none of them has placed a particular emphasis or provided guidance on light-intensity physical activity (LPA), the intensity which is defined as 1.5–3.0 metabolic equivalents (METs)5; despite that LPA, like casual walking or housework, represents the predominant form of physical activity (PA) in one’s daily life, and that there is accumulating evidence linking increased LPA to cardiometabolic benefits.6–8 Notably, the adherence to current recommendations of MVPA or VPA has not been improved even after years of efforts and remains at a suboptimal level of about 63–65%.9 In contrast, LPA is attainable and consistent with most activities of daily living.
Recommendations of PA in present guidelines have largely relied on questionnaires, which, however, could not accurately capture the intensities of PA, in particular, for LPA. This may account for the previous inconsistent findings relating to the effects of LPA.10–12 Activity monitors (e.g. pedometers and accelerometers), which document LPA in an objective manner and can differentiate LPA from MVPA or VPA, may overcome such limitation. In recent years, these monitors have experienced a surge in popularity, and are frequently used to investigate the influence of objectively measured LPA on health outcomes like all-cause or cardiovascular mortality.13–18 Yet, the findings of these studies remain inconclusive, in particular, for the risk of cardiovascular mortality, with half of them suggesting that LPA cannot effectively prevent against cardiovascular mortality.13–15
Given these and to assist in informing clinical decision-makers to recommend LPA for health promotion, we conducted this meta-analysis with dose–response analysis of prospective cohort studies to systematically investigate the association of objectively measured LPA with the risk of cardiovascular mortality in the general population. Since sedentary time is associated with an increased risk of cardiovascular mortality,19 we also assessed whether its replacement with an equal time-length of LPA would produce any favourable result in reducing the risk of cardiovascular mortality. Furthermore, to facilitate the use of LPA in clinical practice, we compared its effectiveness in reducing the risk of cardiovascular mortality with that of MVPA, a PA form that is consistently recommended in current health guidelines.3,4
Methods
This meta-analysis was reported with reference to the Preferred Reporting Items for Systematic Review and Meta-Analysis guideline (Supplementary material online, Table S1), following an a priori designed protocol published on PROSPERO (CRD42019147767).
Characteristics of included studies on light-intensity physical activity and risk of cardiovascular mortality
| Author (year) . | Study . | Age (years) . | Men (%) . | BMI (kg/m2) . | Follow-up (years) . | Sample size . | Covariables controlled for . | Quality score . | |
|---|---|---|---|---|---|---|---|---|---|
| Total . | Death . | ||||||||
| LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.13 (2018) | ABCS | 66.7 | 44 | 25.6 | 14.2 | 851 | 24 | Education, smoking, health conditions at baseline, and achieving at least 150 min/week of MVPA | Nine stars |
| Ensrud et al.14 (2014) | MrOS | 79 | 100 | NA | 4.5 | 2918 | 138 | Age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of instrumental activity of daily living impairments, and percentage body fat | Nine stars |
| Evenson et al.15 (2016) | NHANES | 55.3 | 45.4 | 28.4 | 6.7 | 3809 | 107 | Age, sex, race/ethnicity, educational level, married, cigarette smoking, interaction between current employment and follow-up time, need special equipment to walk, arthritis, cancer, body mass index, interaction between body mass index categories and follow-up time, hypertension, diabetes, sedentary physical activity, and MPVA | Nine stars |
| LaMonte et al.16 (2018A)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race and ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| LaMonte et al.16 (2018)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race, ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| Replacing sedentary time with LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.17 (2018) | ABCS | 52.8 | 44.1 | 25.6 | 14.2 | 851 | 24 | LPA, MVPA, total accelerometer-wearing time, stratified by sex and age textiles, education, smoking, presence of hypertension, heart disease, cancer, and diabetes at baseline | Nine stars |
| Schmid et al.18 (2016) | NHANES | 65 | 53.3 | NA | 6.35 | 3702 | 196 | Age, sex, total accelerometer wear time, all activities except LPA, education, ethnicity, height, smoking, alcohol consumption, total dietary fat intake, total dietary fibre intake, mobility limitations, history of diabetes, history of coronary heart disease, history of congestive heart failure, history of stroke, history of cancer, and waist circumference | Nine stars |
| Author (year) . | Study . | Age (years) . | Men (%) . | BMI (kg/m2) . | Follow-up (years) . | Sample size . | Covariables controlled for . | Quality score . | |
|---|---|---|---|---|---|---|---|---|---|
| Total . | Death . | ||||||||
| LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.13 (2018) | ABCS | 66.7 | 44 | 25.6 | 14.2 | 851 | 24 | Education, smoking, health conditions at baseline, and achieving at least 150 min/week of MVPA | Nine stars |
| Ensrud et al.14 (2014) | MrOS | 79 | 100 | NA | 4.5 | 2918 | 138 | Age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of instrumental activity of daily living impairments, and percentage body fat | Nine stars |
| Evenson et al.15 (2016) | NHANES | 55.3 | 45.4 | 28.4 | 6.7 | 3809 | 107 | Age, sex, race/ethnicity, educational level, married, cigarette smoking, interaction between current employment and follow-up time, need special equipment to walk, arthritis, cancer, body mass index, interaction between body mass index categories and follow-up time, hypertension, diabetes, sedentary physical activity, and MPVA | Nine stars |
| LaMonte et al.16 (2018A)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race and ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| LaMonte et al.16 (2018)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race, ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| Replacing sedentary time with LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.17 (2018) | ABCS | 52.8 | 44.1 | 25.6 | 14.2 | 851 | 24 | LPA, MVPA, total accelerometer-wearing time, stratified by sex and age textiles, education, smoking, presence of hypertension, heart disease, cancer, and diabetes at baseline | Nine stars |
| Schmid et al.18 (2016) | NHANES | 65 | 53.3 | NA | 6.35 | 3702 | 196 | Age, sex, total accelerometer wear time, all activities except LPA, education, ethnicity, height, smoking, alcohol consumption, total dietary fat intake, total dietary fibre intake, mobility limitations, history of diabetes, history of coronary heart disease, history of congestive heart failure, history of stroke, history of cancer, and waist circumference | Nine stars |
ABCS, the Sweden Attitude Behaviour and Change study; BMI, body mass index; LPA, light-intensity physical activity; MrOS, the Osteoporotic Fractures in Men Study; MVPA, moderate-to-vigorous physical activity; NA, not applicable; NHANES, the National Health and Nutrition Examination Survey; OPACHS, the Objective Physical Activity and Cardiovascular Health Study.
This study stratified LPA as low- and high-LPA, with A as low-LPA and B as high-LPA.
Characteristics of included studies on light-intensity physical activity and risk of cardiovascular mortality
| Author (year) . | Study . | Age (years) . | Men (%) . | BMI (kg/m2) . | Follow-up (years) . | Sample size . | Covariables controlled for . | Quality score . | |
|---|---|---|---|---|---|---|---|---|---|
| Total . | Death . | ||||||||
| LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.13 (2018) | ABCS | 66.7 | 44 | 25.6 | 14.2 | 851 | 24 | Education, smoking, health conditions at baseline, and achieving at least 150 min/week of MVPA | Nine stars |
| Ensrud et al.14 (2014) | MrOS | 79 | 100 | NA | 4.5 | 2918 | 138 | Age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of instrumental activity of daily living impairments, and percentage body fat | Nine stars |
| Evenson et al.15 (2016) | NHANES | 55.3 | 45.4 | 28.4 | 6.7 | 3809 | 107 | Age, sex, race/ethnicity, educational level, married, cigarette smoking, interaction between current employment and follow-up time, need special equipment to walk, arthritis, cancer, body mass index, interaction between body mass index categories and follow-up time, hypertension, diabetes, sedentary physical activity, and MPVA | Nine stars |
| LaMonte et al.16 (2018A)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race and ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| LaMonte et al.16 (2018)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race, ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| Replacing sedentary time with LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.17 (2018) | ABCS | 52.8 | 44.1 | 25.6 | 14.2 | 851 | 24 | LPA, MVPA, total accelerometer-wearing time, stratified by sex and age textiles, education, smoking, presence of hypertension, heart disease, cancer, and diabetes at baseline | Nine stars |
| Schmid et al.18 (2016) | NHANES | 65 | 53.3 | NA | 6.35 | 3702 | 196 | Age, sex, total accelerometer wear time, all activities except LPA, education, ethnicity, height, smoking, alcohol consumption, total dietary fat intake, total dietary fibre intake, mobility limitations, history of diabetes, history of coronary heart disease, history of congestive heart failure, history of stroke, history of cancer, and waist circumference | Nine stars |
| Author (year) . | Study . | Age (years) . | Men (%) . | BMI (kg/m2) . | Follow-up (years) . | Sample size . | Covariables controlled for . | Quality score . | |
|---|---|---|---|---|---|---|---|---|---|
| Total . | Death . | ||||||||
| LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.13 (2018) | ABCS | 66.7 | 44 | 25.6 | 14.2 | 851 | 24 | Education, smoking, health conditions at baseline, and achieving at least 150 min/week of MVPA | Nine stars |
| Ensrud et al.14 (2014) | MrOS | 79 | 100 | NA | 4.5 | 2918 | 138 | Age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of instrumental activity of daily living impairments, and percentage body fat | Nine stars |
| Evenson et al.15 (2016) | NHANES | 55.3 | 45.4 | 28.4 | 6.7 | 3809 | 107 | Age, sex, race/ethnicity, educational level, married, cigarette smoking, interaction between current employment and follow-up time, need special equipment to walk, arthritis, cancer, body mass index, interaction between body mass index categories and follow-up time, hypertension, diabetes, sedentary physical activity, and MPVA | Nine stars |
| LaMonte et al.16 (2018A)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race and ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| LaMonte et al.16 (2018)a | OPACHS | 78.6 | 0 | 28.1 | 3.1 | 6382 | 154 | Awake accelerometer wear time, age, race, ethnicity, education, current smoking, alcohol intake in past 3 months, age at menopause, self-rated general health, and number of comorbid conditions | Nine stars |
| Replacing sedentary time with LPA and risk of cardiovascular mortality | |||||||||
| Dohrn et al.17 (2018) | ABCS | 52.8 | 44.1 | 25.6 | 14.2 | 851 | 24 | LPA, MVPA, total accelerometer-wearing time, stratified by sex and age textiles, education, smoking, presence of hypertension, heart disease, cancer, and diabetes at baseline | Nine stars |
| Schmid et al.18 (2016) | NHANES | 65 | 53.3 | NA | 6.35 | 3702 | 196 | Age, sex, total accelerometer wear time, all activities except LPA, education, ethnicity, height, smoking, alcohol consumption, total dietary fat intake, total dietary fibre intake, mobility limitations, history of diabetes, history of coronary heart disease, history of congestive heart failure, history of stroke, history of cancer, and waist circumference | Nine stars |
ABCS, the Sweden Attitude Behaviour and Change study; BMI, body mass index; LPA, light-intensity physical activity; MrOS, the Osteoporotic Fractures in Men Study; MVPA, moderate-to-vigorous physical activity; NA, not applicable; NHANES, the National Health and Nutrition Examination Survey; OPACHS, the Objective Physical Activity and Cardiovascular Health Study.
This study stratified LPA as low- and high-LPA, with A as low-LPA and B as high-LPA.
Data sources and search strategy
An electronic literature search of PubMed and Scopus from their inceptions to 5 April 2020 was conducted, using the terms or words related to ‘physical activity’, ‘cohort studies’, and ‘mortality’ with the language restriction to English. The detailed literature search strategy, which was made upon the discussion by two investigators (S.Q. and X.C.), was available in Supplementary material online, Table S2. Reference lists from identified articles were manually examined for any relevant studies.
Subgroup analysis on the association between light-intensity physical activity and risk of cardiovascular mortality
| Variables . | No. of studies . | HR (95% CI) . | I2 (%) . | Pinteraction . |
|---|---|---|---|---|
| Sex | ||||
| Men | 1 | 0.81 (0.64–1.02) | NA | 0.76a |
| Women | 2 | 0.71 (0.49–1.03) | 89 | |
| Combined | 2 | 0.92 (0.76–1.12) | 53 | |
| Wearing site | ||||
| Waist/hip | 4 | 0.80 (0.65–0.99) | 88 | 0.96 |
| Arm | 1 | 0.81 (0.64–1.02) | NA | |
| Controlling for | ||||
| Age | ||||
| Yes | 4 | 0.80 (0.66, 0.99) | 88 | 0.96 |
| No | 1 | 0.79 (0.59, 1.05) | NA | |
| BMI | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | NA | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Smoking | ||||
| Yes | 5 | 0.80 (0.67, 0.96) | 84 | NA |
| No | 0 | NA | NA | |
| Alcohol | ||||
| Yes | 2 | 0.71 (0.49, 1.03) | 89 | 0.33 |
| No | 3 | 0.89 (0.77, 1.04) | 53 | |
| MVPA | ||||
| Yes | 2 | 0.92 (0.76, 1.12) | 53 | 0.33 |
| No | 3 | 0.74 (0.59, 0.94) | 78 | |
| ST | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | <1 | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Variables . | No. of studies . | HR (95% CI) . | I2 (%) . | Pinteraction . |
|---|---|---|---|---|
| Sex | ||||
| Men | 1 | 0.81 (0.64–1.02) | NA | 0.76a |
| Women | 2 | 0.71 (0.49–1.03) | 89 | |
| Combined | 2 | 0.92 (0.76–1.12) | 53 | |
| Wearing site | ||||
| Waist/hip | 4 | 0.80 (0.65–0.99) | 88 | 0.96 |
| Arm | 1 | 0.81 (0.64–1.02) | NA | |
| Controlling for | ||||
| Age | ||||
| Yes | 4 | 0.80 (0.66, 0.99) | 88 | 0.96 |
| No | 1 | 0.79 (0.59, 1.05) | NA | |
| BMI | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | NA | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Smoking | ||||
| Yes | 5 | 0.80 (0.67, 0.96) | 84 | NA |
| No | 0 | NA | NA | |
| Alcohol | ||||
| Yes | 2 | 0.71 (0.49, 1.03) | 89 | 0.33 |
| No | 3 | 0.89 (0.77, 1.04) | 53 | |
| MVPA | ||||
| Yes | 2 | 0.92 (0.76, 1.12) | 53 | 0.33 |
| No | 3 | 0.74 (0.59, 0.94) | 78 | |
| ST | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | <1 | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
BMI, body mass index; CI, confidence interval; cpm, counts/min; HR, hazard ratio; LPA, light-intensity physical activity; MPVA, moderate-to-vigorous physical activity; NA, not applicable; ST, sedentary time.
It only compared between men and women.
Excluding the one within 50–1064 cpm.
Subgroup analysis on the association between light-intensity physical activity and risk of cardiovascular mortality
| Variables . | No. of studies . | HR (95% CI) . | I2 (%) . | Pinteraction . |
|---|---|---|---|---|
| Sex | ||||
| Men | 1 | 0.81 (0.64–1.02) | NA | 0.76a |
| Women | 2 | 0.71 (0.49–1.03) | 89 | |
| Combined | 2 | 0.92 (0.76–1.12) | 53 | |
| Wearing site | ||||
| Waist/hip | 4 | 0.80 (0.65–0.99) | 88 | 0.96 |
| Arm | 1 | 0.81 (0.64–1.02) | NA | |
| Controlling for | ||||
| Age | ||||
| Yes | 4 | 0.80 (0.66, 0.99) | 88 | 0.96 |
| No | 1 | 0.79 (0.59, 1.05) | NA | |
| BMI | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | NA | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Smoking | ||||
| Yes | 5 | 0.80 (0.67, 0.96) | 84 | NA |
| No | 0 | NA | NA | |
| Alcohol | ||||
| Yes | 2 | 0.71 (0.49, 1.03) | 89 | 0.33 |
| No | 3 | 0.89 (0.77, 1.04) | 53 | |
| MVPA | ||||
| Yes | 2 | 0.92 (0.76, 1.12) | 53 | 0.33 |
| No | 3 | 0.74 (0.59, 0.94) | 78 | |
| ST | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | <1 | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Variables . | No. of studies . | HR (95% CI) . | I2 (%) . | Pinteraction . |
|---|---|---|---|---|
| Sex | ||||
| Men | 1 | 0.81 (0.64–1.02) | NA | 0.76a |
| Women | 2 | 0.71 (0.49–1.03) | 89 | |
| Combined | 2 | 0.92 (0.76–1.12) | 53 | |
| Wearing site | ||||
| Waist/hip | 4 | 0.80 (0.65–0.99) | 88 | 0.96 |
| Arm | 1 | 0.81 (0.64–1.02) | NA | |
| Controlling for | ||||
| Age | ||||
| Yes | 4 | 0.80 (0.66, 0.99) | 88 | 0.96 |
| No | 1 | 0.79 (0.59, 1.05) | NA | |
| BMI | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | NA | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
| Smoking | ||||
| Yes | 5 | 0.80 (0.67, 0.96) | 84 | NA |
| No | 0 | NA | NA | |
| Alcohol | ||||
| Yes | 2 | 0.71 (0.49, 1.03) | 89 | 0.33 |
| No | 3 | 0.89 (0.77, 1.04) | 53 | |
| MVPA | ||||
| Yes | 2 | 0.92 (0.76, 1.12) | 53 | 0.33 |
| No | 3 | 0.74 (0.59, 0.94) | 78 | |
| ST | ||||
| Yes | 1 | 0.98 (0.92, 1.04) | <1 | 0.23 |
| No | 4 | 0.75 (0.63, 0.90) | 67 | |
BMI, body mass index; CI, confidence interval; cpm, counts/min; HR, hazard ratio; LPA, light-intensity physical activity; MPVA, moderate-to-vigorous physical activity; NA, not applicable; ST, sedentary time.
It only compared between men and women.
Excluding the one within 50–1064 cpm.
Study selection
Studies eligible for this meta-analysis should meet the following criteria: (i) enrolling individuals aged at least 18 years; (ii) being prospective cohort designed; (iii) employing activity monitors including pedometers and accelerometers to document LPA quantified in min/day; (iv) reporting the outcome on cardiovascular mortality; and (v) providing hazard ratios (HRs) and corresponding 95% confidence intervals (CIs).
Studies were excluded if they were cross-sectional or case–control studies, failed to document LPA objectively, or did not report outcomes of interest. Studies were also excluded if they had focused only on hospitalized or disease-specific populations.
Data extraction and quality assessment
Two independent investigators (S.Q. and X.C.) collected the data for each eligible study using a standardized excel form, which included: first author, publication year, number of participants and cases, geographic location, mean baseline age and body mass index (BMI), proportion of men, follow-up duration, methods used to define LPA, mortality incidence, effect measure (i.e. HR with 95% CIs), and the most completely adjusted covariates. Data from different exposure categories of LPA as well as the corresponding effect measures and the follow-up person-years were also recorded if available. In case of a cohort generating multiple publications, only the one with the most complete data was selected.20,21 Study quality was assessed by the Newcastle-Ottawa Scale, which has a score up to nine stars.22 Disagreement was solved by discussion with a third investigator (U.S.).
Data synthesis and analysis
The summary HR for cardiovascular mortality per 30 min/day of objectively measured LPA was calculated using a random-effects model22 for the primary analysis. If such an individual HR was not provided, it was imputed based on the approaches described previously.21,23 For this, the median or mean LPA for each category was assigned to the corresponding HR.22 If the median or mean was not reported, it was obtained using the mid-point of boundaries, or calculated by assuming the width of the open-ended highest LPA category was equal to that of its adjacent category.24,25 For the additional analysis that compares the effectiveness of LPA vs. equal activity-amount of MVPA in reducing the risk of mortality using a random-effects model, the activity-amount was defined as intensity × time, where the intensity of LPA was assigned as 2.3 METs and MVPA as 5 METs based on the 2011 Compendium of Physical Activities.5 Dose–response analysis was performed with reference to the method described by Greenland and Longnecker.26,27 The non-linear association was assessed using a restricted cubic spline, with the knot locating at the 10th, 50th, and 90th percentiles of the overall exposure distribution. The non-linearity was determined by testing the coefficient of the second spline, which was assumed to be equal to zero.
Heterogeneity was assessed by I2 statistic, with its value of ≥50% being considered significant.22 Subgroup or meta-regression analyses were performed to evaluate the influence on the summary HR from age, BMI, sex, geographic location, follow-up time, adjusted covariates (e.g. MVPA), LPA cut-off points, and activity monitor types (e.g. uniaxial vs. triaxial), if available. Publication bias was assessed using the Begg’s test.22 All statistical analyses were performed using STATA (Version 14.0, StataCorp LP, College Station, TX, USA), and a two-sided P-value <0.05 was considered statistically significant.
Results
Identification and characteristics of included studies
The literature search yielded 511 unique citations from PubMed and Scopus, of which six cohort studies were included.13–18 The reasons for other study exclusion are given in Figure 1. Of the included studies, the one by LaMonte et al.16 stratified LPA as low- and high-LPA, which was later treated as two separate datasets during the analyses.
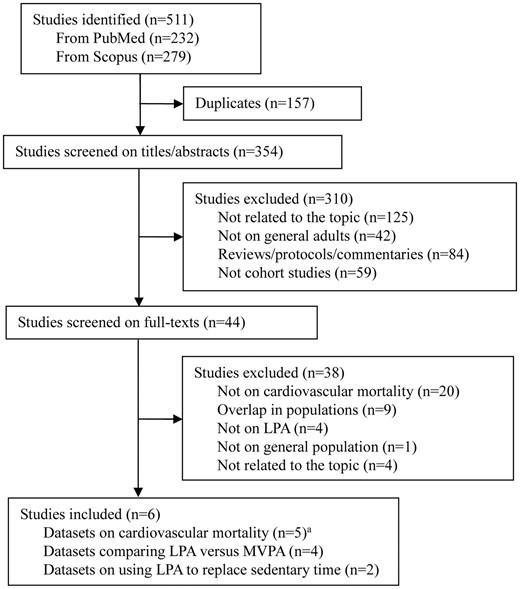
Search flowchart.
aThe study by LaMonte et al.16 had two datasets and were included separately. LPA, light-intensity physical activity; MVPA, moderate-to-vigorous physical activity.
The characteristics of included studies are shown in Table 1. The mean age of enrolled participants ranged from 52.8 to 79 years, and their BMI varied from 25.6 to 28.4 kg/m2. All studies were conducted in developed countries, with four in the USA14–16,18 and two in Sweden.13,17 All death events were ascertained by reviewing death certificates and/or administrative databases including Cause of Death Register and National Death Index. All studies were judged to be of good quality based on the Newcastle-Ottawa Scale (Table 1).
LPA was measured by accelerometers in all included studies. And data proceeded for LPA analysis from the accelerometers were required to be recorded for >10 h for >1 day among most of the included studies (Supplementary material online, Table S3). These accelerometers were generally worn on waist or hip, except one study reported to be on arm,14 for seven consecutive days. Three types of accelerometers were used, with the ActiGraph uniaxial and triaxial ones (ActiGraph, Pensacola, FL, USA) being most commonly employed.13,15–18 The definitions of LPA varied in general, and most of them were around 100–2019 counts/min,15–18 based on their accelerometer readings (Supplementary material online, Table S3).
LPA and the risk of cardiovascular mortality
Five datasets from four studies enrolling 13 960 participants with 423 cardiovascular deaths during a mean follow-up period of 7.1 years were included.13–16 Among them, only two datasets from the same study conducted in older adults presented a favourable effect of LPA against risk of cardiovascular mortality with statistical significance.16 The summary HR for cardiovascular mortality per 30 min/day of LPA was pooled to be 0.80 (95% CI 0.67–0.96), with evidence of significant heterogeneity (I2 = 84%) (Figure 2A). Yet the HR became non-significant in studies controlling for MVPA (HR 0.92, 95% CI 0.76–1.12) or sedentary time (HR 0.98, 95% CI 0.92–1.04). Meta-regression analysis noted that the HR was not affected by sex (Table 2) nor age (Supplementary material online, Table S4). No evidence of publication bias was detected (P > 0.99 for Begg’s test). Despite the dose–response analysis suggested a non-linear relationship between LPA and the risk of cardiovascular mortality (Pnon-linearity = 0.004), the curve indicated that the higher the LPA time, the larger the risk reduction in cardiovascular mortality, in general (Figure 2B).
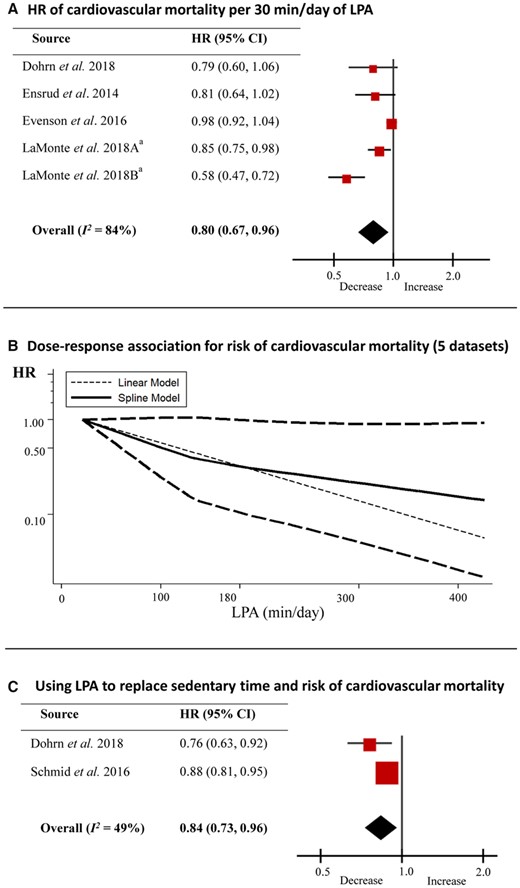
Light-intensity physical activity and risk of cardiovascular mortality. (A) Hazard ratio of cardiovascular mortality per 30 min/day of light-intensity physical activity; (B) dose–response analysis for risk of cardiovascular mortality in relation to light-intensity physical activity; (C) replacing sedentary time by light-intensity physical activity and risk of cardiovascular mortality. aData derived from the same study,16 with A representing data from low-light-intensity physical activity and B from high-light-intensity physical activity. CI, confidence interval; HR, hazard ratio; LPA, light-intensity physical activity.
Replacing sedentary time with LPA and the risk of cardiovascular mortality
Two datasets from two studies enrolling 4553 participants assessed the impact of using LPA to replace sedentary time in reducing the risk of cardiovascular mortality,17,18 in which the isotemporal substitution method was consistently employed.28 Results showed that the pooled HR for cardiovascular mortality was 0.84 (95% CI 0.73–0.96, I2 = 49%), when replacing 30 min/day of sedentary time with an equal time-length of LPA (Figure 2C). Moreover, there exists the trend that the longer the sedentary time being replaced by LPA, the larger the benefit in reducing the risk of cardiovascular mortality (HR 0.76 for replacing 30 min/day of sedentary time vs. HR 0.91 for replacing 10 min/day of sedentary time, Pcomparison = 0.06), as evidenced by the results from Dohrn et al.17
LPA vs. MVPA in reducing the risk of cardiovascular mortality
Of the individual studies that evaluated both LPA and MVPA with identical covariates adjustment, four provided outcomes on cardiovascular mortality.13–16
Comparison for an equal time-length
The scale set for the equal time-length of LPA or MVPA was 30 min/day, which is the recommended time-dose for MVPA by current guidelines.3,29 The summary HRs for cardiovascular mortality were 0.83 (95% CI 0.71–0.97) per 30 min/day of LPA, and 0.54 (95% CI 0.37–0.81) per 30 min/day of MVPA, with the difference being significant (Pcomparison = 0.046, Figure 3A).
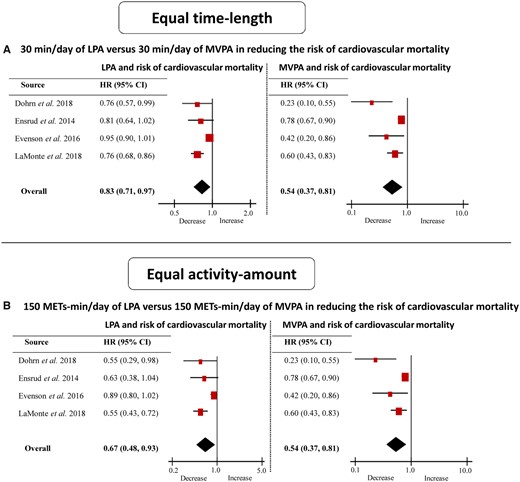
Light-intensity physical activity vs. moderate-to-vigorous physical activity in an equal time-length or at an equal activity-amount in reducing risk of cardiovascular mortality. (A) 30 min/day of light-intensity physical activity vs. 30 min/day of moderate-to-vigorous physical activity in reducing risk of cardiovascular mortality; (B) 150 metabolic equivalents-min/day of light-intensity physical activity vs. 150 metabolic equivalents-min/day of moderate-to-vigorous physical activity in reducing risk of cardiovascular mortality. CI, confidence interval; HR, hazard ratio; LPA, light-intensity physical activity; MVPA, moderate-to-vigorous physical activity.
Comparison for an equal activity-amount
The scale assigned for the equal activity-amount of LPA or MVPA was 150 METs-min/day, which equals to 65 min/day of LPA or 30 min/day of MVPA. The pooled HRs for cardiovascular mortality were comparable between LPA and MVPA (HR 0.67 per 150 METs-min/day of LPA vs. HR 0.54 per 150 METs-min/day of MVPA, Pcomparison = 0.41, Figure 3B).
Discussion
Summary of the main findings
This meta-analysis of prospective cohort studies conducted in the general population showed that: (i) LPA per every 30 min/day reduced the risk of cardiovascular mortality by 20%; (ii) substituting LPA for sedentary time with an equal time-length decreased the risk of cardiovascular mortality; and (iii) LPA was as effective as MVPA in lowering the risk of cardiovascular mortality, when performed at an equal activity-amount.
Interpretations and implications
Physical activity remains a cornerstone in the management of metabolic disorders.30,31 However, current guidelines and/or position statements have focused exclusively on MVPA or VPA, with little mention on LPA. The recent meta-analyses may have bridged this gap by showing that LPA, which is objectively measured by accelerometers, is able to lower the risk of all-cause mortality.6,32 As a supplementation to their work, our study provided further evidence that LPA decreased the risk of cardiovascular mortality, and that sex difference or age did not moderate the risk reduction in cardiovascular mortality. It is speculated that these outcomes might be modulated by a series of cardiometabolic improvements resulted from LPA, such as improved glycaemic control, lowered blood pressure, and enhanced vascular function,6,33 although the underlying mechanism remains to be elucidated.
Being independent of PA, sedentary time has been proven to be associated with an increased risk of cardiovascular and all-cause mortality.19 A recent meta-analysis has suggested that breaking up sedentary time with LPA could lower post-prandial glucose, decrease insulin secretion, and reduce inflammatory response.34 As an extension to these findings, our study showed that replacing sedentary time with LPA for 30 min/day lowered the risk of cardiovascular mortality by ∼16%, and that the longer the sedentary time being replaced by LPA, the larger the risk reduction in cardiovascular mortality. These undoubtfully highlight the effectiveness of LPA in combating the harm from the accumulation of sedentary behaviour, and may imply that substituting LPA for sedentary behaviour could be a practical and attractive disease prevention strategy for office workers or the elderly who may spend most of their time being sedentary during the day. Yet, it should be noted that the replacement effect of LPA in our meta-analysis was assessed by the isotemporal substitution method, which reflects only the theoretical effect of replacing sedentary time by LPA, rather than the effect from the actual changes in sedentary time. Thus, studies with randomized controlled designs that investigate the benefits of actual sedentary time changes replaced by LPA (e.g. 30–60 min/day) on cardiometabolic markers (e.g. glycaemic control or physical fitness) and the subsequent risk of cardiovascular mortality during a relatively long follow-up period (e.g. >2 years) are needed in future.
Current guidelines and position statements have also highlighted the superiority of PA performed at a higher intensity in promoting cardiometabolic health.3,29 Partly in agreement with this, we found that MVPA did introduce a larger risk reduction in cardiovascular mortality compared with an equal time-length of LPA. Yet, as evidenced by our direct comparison, this strength did not persist any more if their activity-amounts were comparable, indicating that such a particular emphasis on high-intensity to yield better benefits is not a must. This is in support of the latest notion that any PA, including LPA, is good for health.35 Moreover, this might be of major clinical relevance, since it may foster confidence in recommending LPA for individuals who are initially unable to perform MVPA or VPA (e.g. the elderly, patients with myocardial infarction) or for those who are unwilling to undertake MVPA or VPA because of uncomfortable feelings during PA.
Our study has also provided some insights as to what extent the time-dose of LPA can be recommended for possible health promotion. In contrast to previous studies that suggested a linear dose–response association between subjectively measured PA and risk of non-alcoholic fatty liver disease25 or heart failure,36 our dose–responses analyses found that objectively measured LPA was non-linearly and inversely related to the risk of cardiovascular mortality. From the curves derived, we observed that LPA exceeding 180 min/day yielded a significant effect in reducing cardiovascular mortality. Considering the results from Lee et al.37 that the major stepping form in a day was at a stepping rate of 1–39 steps/min (incidental steps) in the elderly, and given that LPA is the major form of PA, it seems then the optimal steps/day would be maximized to be about 7200, if our results should be transferred into clinical practice.
In addition to the time-dose of LPA for recommendation, our study showed that the risk reduction of LPA in cardiovascular mortality was independent of cardiovascular risk factors including age, BMI, smoking, or alcohol intake. However, this benefit of LPA disappeared when controlling for MVPA, while this result remains to be confirmed if it would be influenced by the small number of included studies and if it is necessary to control for MVPA when analysing the benefits of LPA on health outcomes in light of the potential risk of over-adjustment bias.
Strengths and limitations
Our study is the most comprehensive meta-analysis with a sample size over 13 000 that explored the association between objectively measured LPA and risk of cardiovascular mortality in the general population. Apart from this, our subgroup and meta-regression analyses, the dose–response curve, as well as the comparisons between LPA and MPVA would help to facilitate the interpretations of our results.
However, our study has several limitations. First, we cannot exclude the possibility that our results might be influenced by unmeasured confounding bias. For example, LPA was measured only once at baseline, while the change in LPA during the follow-up years might affect the observed relationships. Moreover, we are not able to ascertain whether LPA is a truly independent predictor of cardiovascular mortality, since it is plausible that the performance of LPA could be only a marker for physiological well-being that is closely related to numerous health outcomes. Therefore, future studies are required to employ a randomized controlled design to assess whether the increases in LPA resulted from the interventions that target at PA promotion would be responsible for the reduced risk of cardiovascular mortality.
Second, despite of the clear definitions of LPA in all included studies, their inconsistent criteria, which might be due to the differences in the accelerometer brands, location, or types (Supplementary material online, Table S3), may contribute to marked heterogeneity observed in this meta-analysis. However, our meta-regression analysis did not demonstrate that such an inconsistency may significantly affect the summary HRs (Supplementary material online, Table S4). This could be also supported by the individual study reporting consistent results based on different LPA definitions,15 as well as by the results from our analyses that the differences in the location (Table 2) or types (Supplementary material online, Table S4) of the accelerometers did not alert the summary HR for cardiovascular mortality significantly.
Third, the enrolled participants in our meta-analysis were rather older than young, and our main findings may therefore be more applicable to adult population at older age. On this regard, future research with a specific focus on young adults, or extensively, on diseased population stratified by age, would be helpful to enrich the understanding of the health benefits of LPA. Fourth, the number of included studies was rather small, and our outcome of interest was exclusively on cardiovascular mortality but not on a broad area such as major adverse cardiovascular events, albeit there is evidence that LPA is helpful to lower the risk of major adverse cardiovascular events.38 This may potentially limit the wide interpretation of our findings. Fifth, all included studies were from Western countries, while it remains unclear whether our conclusions could be generalized to individuals from Eastern countries like China or India. Finally, although publication bias was not detected by the Begg’s test, the failure to search for grey literature or unpublished studies may still be likely to incur this.
Conclusions
In conclusion, increased LPA shows potential in reducing the risk of cardiovascular mortality and may exhibit a comparative effect to MVPA if performed at an equal activity-amount. Furthermore, substituting sedentary behaviour with LPA may lower the risk of cardiovascular mortality. As a result, it is appropriate and clinically important to recommend LPA in daily life, in particular for those who cannot start MPVA or VPA at initial. Moreover, interventions designed to promote LPA, such as using step counters and mobile applications,39,40 should be encouraged in the general population.
Supplementary material
Supplementary material is available at European Heart Journal – Quality of Care andClinical Outcomes online.
Conflict of interest: None declared.



