-
PDF
- Split View
-
Views
-
Cite
Cite
K Kito, M Okamoto, K Shirakura, H Kobayashi, I Chikuda, J Nishikawa, Y Iseki, T Katayama, T Sajima, H Kawashima, H Yamamoto, Y Watanabe, N Yokoyama, K Kozuma, A Kataoka, Efficacy of the party balloon inflation maneuver comparing with the valsalva maneuver for diagnosis of PFO and HOCM in transthoracic echocardiography, European Heart Journal - Cardiovascular Imaging, Volume 26, Issue Supplement_1, January 2025, jeae333.329, https://doi.org/10.1093/ehjci/jeae333.329
Close - Share Icon Share
Abstract
Previously, we reported clinical cases where the party balloon inflation manoeuvre (PBIM) proved more effective than the conventional Valsalva manoeuvre (VM) in diagnosing patent foramen ovale (PFO) and hypertrophic obstructive cardiomyopathy (HOCM). Additionally, increased venous return with PBIM was observed using hepatic vein flow assessed by transthoracic echocardiography (TTE). PBIM may offer enhanced visualisation of provocation, especially in cases where VM is insufficient. However, the haemodynamic evidence for the efficacy of PBIM with the optimal protocol compared to VM for PFO and HOCM has not been established.
This study aimed to demonstrate the superiority of PBIM over the conventional VM and establish the optimal PBIM protocol for diagnosing PFO and HOCM through two experiments.
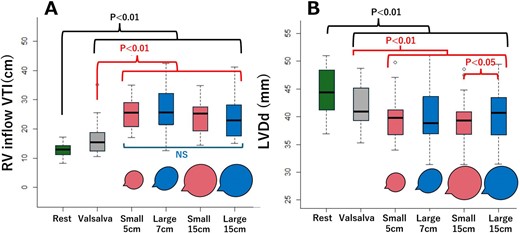
(Experiment 1) To understand the characteristics of party balloons, we measured the diameters and corresponding pressures of two commercially available balloons of different sizes (23 and 30 cm, referred to as a smaller balloon (SB) and a larger balloon (LB), respectively). (Experiment 2) We studied 23 healthy adult volunteers (physicians or sonographers, mean age 36 ± 10 years, 78% male), to investigate the haemodynamic effects of PBIM using protocols derived from the results of Experiment 1. Haemodynamic parameters, such as right ventricular inflow-velocity time integral (RV inflow-VTI) representing PFO haemodynamics and left ventricular end-diastolic diameter (LVDd) representing HOCM haemodynamics, were assessed by TTE during (for HOCM) and after (for PFO) the manoeuvre. These parameters were compared among PBIM, rest, and VM.
Experiment 1: Figure 1 shows that both the SB and LB reached their peak pressures at diameters of 5 cm and 7 cm, respectively, and the pressures stabilised around a diameter of 15 cm. Experiment 2: Based on Experiment 1, four different PBIM protocols were used, SB inflated to 5 cm and 15 cm, and LB inflated to 7 cm and 15 cm. RV inflow-VTI increased in all PBIM protocols compared to VM (p <0.01). However, no significant differences were observed among all PBIM protocols (Figure 2A). LVDd decreased in all PBIM protocols compared to VM (p <0.01). Specifically, LVDd was significantly smaller when the SB was inflated to a diameter of 15 cm compared to the LB inflated to a diameter of 15 cm (p <0.05) (Figure 2B).
PBIM can effectively provoke the haemodynamic changes associated with PFO and HOCM compared to VM, potentially leading to a more accurate diagnosis. Notably, using a smaller balloon may be more advantageous for diagnosing HOCM.

Author notes
Funding Acknowledgements: None.



