-
Views
-
Cite
Cite
Eugenio Picano, Eliseo Vano, Robert P Gale, Patrick Serruys, Cardiac radiation exposure and incident cancer: challenges and opportunities, European Heart Journal - Cardiovascular Imaging, Volume 25, Issue 12, December 2024, Pages 1620–1626, https://doi.org/10.1093/ehjci/jeae257
Close - Share Icon Share
Abstract
The use of radiological procedures has enormously advanced cardiology. People with heart disease are exposed to ionizing radiation. Exposure to ionizing radiation increases lifetime cancer risk with a dose-proportional hazard according to the linear no-threshold model adopted for radioprotection purposes. In the USA, the average citizen accumulates a median annual medical radiation exposure of 2.29 millisievert per year per capita as of the radiologic year 2016, corresponding to the dose exposure of 115 chest X-rays. Cardiology studies often involve high exposures per procedure accounting for ∼30–50% of cumulative medical radiation exposures. Malignancy is more incident in the most radiosensitive organs receiving the largest organ dose from cardiac interventions and cardiovascular imaging testing, such as the lung, bone marrow, and female breast. The latency period between radiation exposure and cancer is thought to be at least 2 years for leukaemia and 5 years for all solid cancers, and differences are more likely to emerge in cardiology studies with longer follow-up and inclusion of non-cardiovascular endpoints such as cancer incidence. In cardiological studies, excess cancers are observed 3–12 years following exposure, with longer follow-up times showing greater differences in cancer incidence. The presumed associated excess cancer risk needs greater study. These exposures provide a unique opportunity to expand our knowledge of the relationship between exposure to ionizing radiation and cancer risk. Future trials comparing interventional fluoroscopy vs. optimal medical therapy or open surgery should include a cancer incidence endpoint.
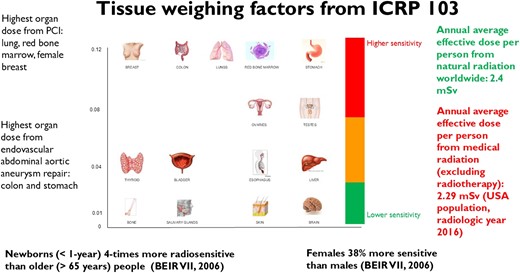
Different radiosensitivity of different organs is expressed by a tissue weighting factor, with higher values indicating higher cancer risk. Original data from ICRP 2021. The total annual global per capita effective dose due to natural radiation sources is 2.4 mSv from cosmic rays, terrestrial gamma rays, inhalation, and ingestion. The total annual medical per capita effective dose is referred to as the radiological year 2016 in the USA and includes diagnostic radiology, interventional radiology, and nuclear medicine, and excludes radiotherapy.





