-
PDF
- Split View
-
Views
-
Cite
Cite
G Joy, JD Crane, JB Augusto, C Lau, A Seraphim, A Bhuva, JC Moon, H Xue, P Kellman, JK Cruickshank, BM Mcgowan, C Manisty, Microvascular and mechanical improvements following bariatric surgery in the obese; mechanistic insights from advanced & automated quantitative perfusion cardiac MRI, European Heart Journal - Cardiovascular Imaging, Volume 22, Issue Supplement_1, January 2021, jeaa356.298, https://doi.org/10.1093/ehjci/jeaa356.298
Close - Share Icon Share
Abstract
Type of funding sources: Public Institution(s). Main funding source(s): Guy"s and St Thomas" Charity University College London Hospital Biomedical Research Centre
In people with obesity, bariatric surgery reduces mortality, heart failure and coronary disease, improving metabolic (blood sugar, lipid profile, inflammation) and cardiovascular (diastolic/systolic function, filling pressure, cardiac remodelling) parameters. Myocardial microvascular function is a candidate causal link of metabolic to structural cardiac abnormalities.
We hypothesised that bariatric surgery could improve myocardial microvascular and mechanical function in both those with and without diabetes.
Methods Before and six months after bariatric surgery, 24 subjects with obesity were assessed with haematology, biochemistry and advanced CMR (cines, vasodilator adenosine stress and rest fully-automated quantitative perfusion mapping, tissue-tracking (CVI42, post processing).
Results. Mean age was 49± 12 years, 35%(8) were male, 63%(15), had hypertension, 17 (71%) had diabetes. Surgery resulted in decreases in BMI (44 ± 7 to 34 ± 6 kg/m2 p = 0.0001) and HbA1c (57 ± 16 to 42 ± 9mmol/mol p = 0.0001). EF% and absolute LV end-diastolic volumes remained unchanged, but mass regressed and myocardial contraction fraction (ratio of stroke volume and LV volume) increased (see Table). There were also strain improvements (radial 35 ± 8.8 to 37.3 ± 8.7 %p = 0.029) (circumferential -19.8 ± 2.3 vs -20.7 ± 3% p = 0.017), although longitudinal did not improve (-16.3 ± 3.2 to -15.9 ± 3% p = 0.25).
Myocardial perfusion significantly improved (stress myocardial blood flow, MBF 2.35 ± 0.71 to 2.80 ± 0.98 ml/g/min p = 0.008; myocardial perfusion reserve MPR 2.47 ± 0.78 to 2.97 ± 0.95 p = 0.005). Improvement in stress MBF and MPR from pre-operative to post-operative was higher in the non-diabetics (n = 7 (29%)) than the diabetics (n = 17 (71%)) (stress MBF: 1.15 ± 1.00 vs 0.16 ± 0.39ml/g/min p = 0.002) MPR: (1.09 ± 0.73 vs 0.25 ± 0.66 p = 0.011).
At 6 months, bariatric surgery results in beneficial myocardial remodelling and substantial improvements in myocardial microvascular function. These improvements occur most in those without diabetes suggesting that there may be reversible and irreversible components to microvascular dysfunction.
Perfusion and strain variables
| Variable . | Pre-op (n = 24) . | Post-op (n = 24) . | p-value . |
|---|---|---|---|
| LVEDV (ml) | 163 ± 28 | 161 ± 29 | 0.64 |
| EF (%) | 70 ± 8 | 70 ± 7 | 0.78 |
| Stroke volume (ml) | 113 ± 19 | 111 ± 21 | 0.6 |
| LV Mass (g) | 117 ± 25 | 103 ± 21 | 0.001 |
| Myocardial contraction fraction | 94 ± 14 | 105 ± 14 | 0.001 |
| Variable . | Pre-op (n = 24) . | Post-op (n = 24) . | p-value . |
|---|---|---|---|
| LVEDV (ml) | 163 ± 28 | 161 ± 29 | 0.64 |
| EF (%) | 70 ± 8 | 70 ± 7 | 0.78 |
| Stroke volume (ml) | 113 ± 19 | 111 ± 21 | 0.6 |
| LV Mass (g) | 117 ± 25 | 103 ± 21 | 0.001 |
| Myocardial contraction fraction | 94 ± 14 | 105 ± 14 | 0.001 |
LVEDV - left ventricular end-diastolic volume, EF - ejection fraction
Perfusion and strain variables
| Variable . | Pre-op (n = 24) . | Post-op (n = 24) . | p-value . |
|---|---|---|---|
| LVEDV (ml) | 163 ± 28 | 161 ± 29 | 0.64 |
| EF (%) | 70 ± 8 | 70 ± 7 | 0.78 |
| Stroke volume (ml) | 113 ± 19 | 111 ± 21 | 0.6 |
| LV Mass (g) | 117 ± 25 | 103 ± 21 | 0.001 |
| Myocardial contraction fraction | 94 ± 14 | 105 ± 14 | 0.001 |
| Variable . | Pre-op (n = 24) . | Post-op (n = 24) . | p-value . |
|---|---|---|---|
| LVEDV (ml) | 163 ± 28 | 161 ± 29 | 0.64 |
| EF (%) | 70 ± 8 | 70 ± 7 | 0.78 |
| Stroke volume (ml) | 113 ± 19 | 111 ± 21 | 0.6 |
| LV Mass (g) | 117 ± 25 | 103 ± 21 | 0.001 |
| Myocardial contraction fraction | 94 ± 14 | 105 ± 14 | 0.001 |
LVEDV - left ventricular end-diastolic volume, EF - ejection fraction
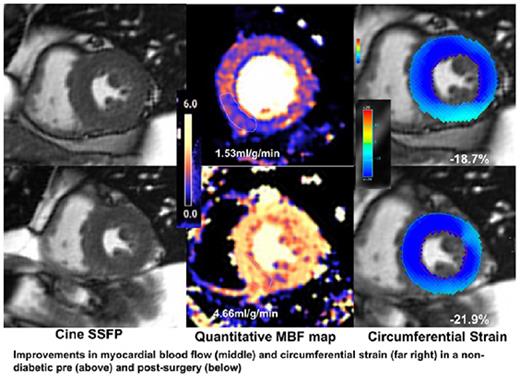
Abstract Figure.
- adenosine
- myocardium
- obesity
- hypertension
- myocardial perfusion
- body mass index procedure
- diabetes mellitus
- inflammation
- myocardial contraction
- congenital heart defects
- heart failure
- vasodilators
- biochemistry
- cardiovascular system
- charities
- diastole
- hemoglobin a, glycosylated
- perfusion
- stroke volume
- surgical procedures, operative
- systole
- blood glucose
- heart
- hematology
- mortality
- stress
- surgery specialty
- coronary heart disease
- ejection fraction
- cardiac mri
- fasting lipid profile
- biomedical research
- bariatric surgery
- left ventricular end diastolic volume
- fractional flow reserve, myocardial



