-
PDF
- Split View
-
Views
-
Cite
Cite
Francesco Meucci, Miroslava Stolcova, Alessio Mattesini, Fabio Mori, Giovanni Orlandi, Francesca Ristalli, Cristina Sarti, Carlo Di Mario, A simple step-by-step approach for proficient utilization of the EchoNavigator technology for left atrial appendage occlusion, European Heart Journal - Cardiovascular Imaging, Volume 22, Issue 7, July 2021, Pages 725–727, https://doi.org/10.1093/ehjci/jeaa165
Close - Share Icon Share
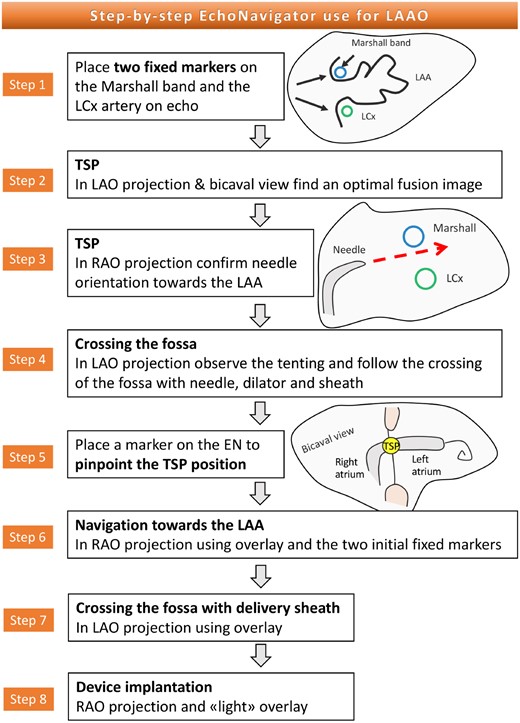
The EchoNavigator® (EN; PhilipsHealthcare, Amsterdam, Netherlands), a novel fusion imaging system that integrates real-time transoesophageal echocardiography (TOE) and fluoroscopy imaging is a promising interventional tool. We propose a simple eight-step sequence (Figure 1, panels 1–8) of utilization of the EchoNavigator for left atrial appendage occlusion (LAAO).

(1) Placement of the Marshall band and left circumflex artery markers on EN. (2) Overlay during trans-septal puncture: tenting phase (left). Note the needle at 4 o’clock in lower right panel. (3) Trans-septal needle in RAO projection: the white (Marshall) and green (CX) markers indicate the LAA orifice. (4) TSP in the LAO projection. Note blood aspirated in a syringe connected to TSP needle (point of arrow) confirming the position in LA. (5) Marking the exact point of trans-septal puncture (septum, purple marker). Note that in the LAO view the two markers defining the base of the LAA are superimposed (right panel). (6) Mullin’s sheath with a pig-tail in RAO projection and overlay of LAA. Navigating inside the LAA becomes intuitive. (7) Amplatzer 12-Fr sheath crossing a floppy septum. TOE imaging clearly shows the tenting but not the position of the sheath with respect to the left atrial opposite border, well delineated with fusion imaging (right panel). (8) Overlay of the appendage during the release of an Amulet device. The two dotted lines clearly show the main axis of the delivery sheath (red) and of the appendage (green). With a counterclockwise movement, the sheath is easily aligned with the main axis of the appendage. Ao, aorta; CX, left circumflex artery; LA, left atrium; LAA, left atrial appendage; RA, right atrium; SP, septum primum; SS, septum secundum; SVC, superior vena cava; TOE, transoesophageal echocardiography; TSP, trans-septal puncture; white or black arrows, inter-atrial septum at fossa ovalis.
First step
Defining the left atrial appendage ostium landmarks: Marshall band and left circumflex artery
This first step is performed in a 0° or 45° mid-oesophageal TOE view where the cross-section of the circumflex artery and the proximal tip of the Marshall band are visualized. These two structures are marked in order to establish the ‘posts of our football goal’ for the subsequent procedural guidance.
Second step
Trans-septal puncture: from beginning to tenting
An easy trans-septal puncture (TSP) is obtained using the overlay of the echographic bicaval view and the fluoroscopic image. In standard anatomies, an adequate visualization of the fossa ovalis is obtained in a shallow left anterior oblique (LAO) projection (approximately 30°). It is possible to fine-tune the angulation simply by turning fluoroscopy with the echographic overlay to optimally open and straighten the fossa.
With a stable bicaval view and LAO projection with an optimal echocardiographic overlay, the operator starts the usual TSP descent manoeuvre. Aided by a good quality imaging the steps of TSP are easily followed (Video 1). Once a good tenting is achieved, the TOE operator switches to a short-axis view to adjust the needle orientation in the postero-anterior direction. Once a satisfactory position according to the echo criteria (aiming at posterior and inferior aspect of the fossa) has been achieved we move to the following step.
Third step
Orientation of the tenting towards the main axis of the left atrial appendage
With the needle held in position, the orientation of the tenting is checked also in the right anterior oblique (RAO) projection (approximately at 30°), where the markers of the left atrial appendage (LAA) ostium are not superimposed and the correct trajectory towards them can be appreciated. A partial misalignment of the puncture can be corrected in height or posteriority with small clock or counterclockwise movements of the needle.
Fourth step
Monitoring of the TSP and crossing of the fossa with the Mullins sheath
With the echo-overlay described in Step 2 (LAO), the TSP is performed directly or assisted by diathermia or a SafeSept wire (PressureProducts, San Pedro, CA, USA) if resistance is felt. While pushing the dilator and/or Mullins sheath to the left, observing the fused image helps to understand the extent of tenting and avoid the risk of damaging the left atrial wall in case a very elastic floppy septum is present.
Fifth step
Marking the position of the trans-septal puncture
Once the fossa ovalis has been crossed and the tension has been released, we can alternate bicaval and short-axis TOE views to identify the exact point of the TSP with a third marker, minimizing the risk of losing position during backward movements of the hardware.
Sixth step
Entering the left atrial appendage with a pigtail catheter and/or with the delivery sheath
After crossing of the fossa with Mullins sheath, we switch to a RAO projection and use fusion imaging to visualize the two markers that allow us to navigate easily into the left upper pulmonary vein or directly in the LAA with the pigtail catheter or the delivery sheath with no need of multiple contrast checks (Video 2).
Seventh step
Monitoring the passage of the device delivery sheath through the fossa using overlay in LAO
The fusion imaging, used again as during the Step 4, allows us to control advancement of the sheath towards the left. When excessive resistance is encountered the echocardiographic overlay is very helpful in precise balloon-dilatation of a rigid fossa.
Eighth step
Following navigation inside the appendage with the sheath and release of the device
The final steps of LAAO are easily followed with 2D/3D TOE imaging. The use of a ‘light’ 2D/3D overlay might be useful, delineating the LAA without covering position and movement of sheaths and devices. The possibility of seeing together the orientation of the sheath and the orientation of the major axis of the appendage could be of great help also to non-experienced operators to understand the degree of rotation (mostly counterclockwise) needed on the sheath to align with the appendage and the position where to start unsheathing the device to reach the desired implant depth (Video 3).
Conclusion
The eight-point flow chart described above (Figure 2) summarizes the main steps to be followed to improve safety and optimize results of LAAO with EchoNavigation.
Conflict of interest: C.D.M. received institutional funding from Edwards, Medtronic, Astra-Zeneca, Daiichi Sankyo, and Shockwave medical. The other authors have nothing do disclose.



