-
PDF
- Split View
-
Views
-
Cite
Cite
Luigi P Badano, Gianfranco Parati, Denisa Muraru, Use of the three-dimensional technique to remove the looking glass through which the echocardiographers have imagined the pathophysiology of atrioventricular valve regurgitation, European Heart Journal - Cardiovascular Imaging, Volume 22, Issue 10, October 2021, Pages 1117–1118, https://doi.org/10.1093/ehjci/jeab155
Close - Share Icon Share
This editorial refers to ‘Differences in mitral valve geometry between atrial and ventricular functional mitral regurgitation in patients with atrial fibrillation: a three-dimensional transesoèhageal echocardiography study’ by G. Uno et al., pp. 1106--16.
Historically, echocardiography has always represented the mainstay of assessing the pathophysiology of atrioventricular valve diseases, their severity, and the extent of their impact on the up- and down-stream cardiac chambers.1 However, both the need of geometric assumptions and the limited visualization of the actual anatomy of the various components of the valve structures inherent to the 2D technique have hampered our ability to understand the various mechanisms leading to functional regurgitation of the atrioventricular valves. These limitations have brought to the oversimplification of these mechanisms, and the functional regurgitation of the atrioventricular valves has grossly been attributed to the dilatation of the annuli secondary to both the remodelling and dysfunction of the ventricles.2 The advent of three-dimensional echocardiography (3DE) has dramatically changed our way of assessing the atrioventricular valves.3,4 Using 3DE, we are able to measure the actual size of valve annuli and leaflets, and the volumes and the function of the cardiac chambers without any geometric assumption and with increased accuracy. Accordingly, we understood that the atria are not a passive bystander in both the tricuspid5,6 and the mitral7 functional regurgitation, and the complex interaction between the annulus enlargement and dysfunction, and the remodelling of valve leaflets as a powerful determinants of the severity of atrioventricular valve regurgitation.8,9 In the end, we realized that atrial fibrillation is not always a consequence of the volume overload of the atria due to the regurgitation of atrioventricular valves, but it can be the cause of the regurgitation of atrioventricular valves.10,11 However, it remains to be clarified whether the dilation of the annulus as a consequence of the enlargement of the atrium is the only mechanism that causes the regurgitation of the atrioventricular valves.
The study by Uno et al.12 provides new insights into the mechanism of atrial functional mitral regurgitation (FMR) by using quantitative 3DE to compare the geometry of mitral annulus and leaflets between the atrial and the ventricular forms of FMR in patients with atrial fibrillation. This sophisticated 3DE study included 135 patients with moderate or more severe atrial (defined as left ventricular—LV—ejection fraction >50% and normal wall motion) or ventricular (defined as LV global dysfunction or regional wall motion) forms of FMR. MR was quantified by vena contracta, and effective regurgitant orifice area and regurgitant volume calculated using the proximal isovelocity surface area method. The authors measured mitral valve complex geometry, LV size and function, and left atrial volumes. The 3DE parameters of the mitral annulus geometry and leaflet area were obtained using a dedicated software package in both mid-systole and end-diastole. Moreover, they measured the total leaflet area in diastole (with both leaflets open) and the closed leaflet area in mid-systole to obtain the coapted leaflet area as the difference between the two. As expected, LV end-diastolic and end-systolic volumes were significantly larger, and LV ejection fraction was significantly reduced in patients with the ventricular form of FMR. Conversely, the left atrial volumes were comparable between patients with the atrial and the ventricular form of FMR. Although the severity of FMR was similar between the atrial and the ventricular forms, the underlying mechanisms were quite different. The size of the annulus was similar between the two forms of FMR. However, both the total leaflet area and the ratio between total leaflet area and annulus area were significantly smaller in the atrial than in the ventricular form of FMR, indicating that the degree of leaflet remodelling was significantly larger in the patients with the ventricular FMR. Since leaflet tethering was also larger (larger tenting volume and coaptation height) in the ventricular form of FMR, it may explain why the severity of the regurgitation was similar. The results of this study suggest a lesser degree of valve adaptation in patients with the atrial form of FMR as the main mechanism to determine the severity of the regurgitation.
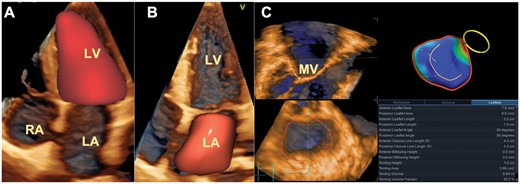
Use of 3D echocardiography to assess the pathophysiology of functional mitral regurgitation. (A) Surface rendering of the left ventricle to obtain volumes, shape, ejection fraction, and total stroke volume. (B) Surface rendering to obtain phasic volumes and function of the left atrium. (C) Surface rendering of the mitral valve to obtain quantitative assessment of the mitral annulus geometry and leaflet size. LA, left atrium; LV, left ventricle; MV, mitral valve; RA, right atrium.
In addition to the insufficient leaflet remodelling, another important determinant of the onset and severity of FMR in patients with atrial fibrillation is the impaired mitral annulus dynamics, with blunted presystolic narrowing, determined by the arrhythmia.13 Therefore, both anatomical and functional determinants intervene to determine the onset and the severity of FMR in patients with atrial fibrillation.
The results of the study by Uno et al.12 are important since they confirm that mitral and tricuspid leaflets are not static structures, but they can adapt in response to either annular dilation or to the leaflet tethering caused by the displacement and reorientation of the papillary muscles. The identification of the molecular mechanisms governing atrioventricular valve leaflet remodelling in functional regurgitation of the atrioventricular valves may help to develop specific treatments to reduce both the incidence and the severity of this condition that negatively affects the morbidity and the mortality of both atrial14 and ventricular15 FMR.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of EHJCI, the European Heart Rhythm Association or the European Society of Cardiology.



