-
PDF
- Split View
-
Views
-
Cite
Cite
Lena Karlsson, Carolina M Hansen, Christina Vourakis, Christopher LF Sun, Shahzleen Rajan, Kathrine B Søndergaard, Linn Andelius, Freddy Lippert, Gunnar H Gislason, Timothy CY Chan, Christian Torp-Pedersen, Fredrik Folke, Improving bystander defibrillation in out-of-hospital cardiac arrests at home, European Heart Journal. Acute Cardiovascular Care, Volume 9, Issue 4_suppl, 1 November 2020, Pages S74–S81, https://doi.org/10.1177/2048872619891675
Close - Share Icon Share
Most out-of-hospital cardiac arrests occur at home with dismal bystander defibrillation rates. We investigated automated external defibrillator coverage of home arrests, and the proportion potentially reachable with an automated external defibrillator before emergency medical service arrival according to different bystander activation strategies.
Cardiac arrests in homes (private/nursing/senior homes) in Copenhagen, Denmark (2008–2016) and registered automated external defibrillators (2007–2016), were identified. Automated external defibrillator coverage (distance from arrest to automated external defibrillator) and accessibility at the time of arrest were examined according to route distance to nearest automated external defibrillator and emergency medical service response time. The proportion of arrests reachable with an automated external defibrillator by bystander was calculated using two-way (from patient to automated external defibrillator and back) and one-way (from automated external defibrillator to patient) potential activation strategies. Of 1879 home arrests, automated external defibrillator coverage ≤100 m was low (6.3%) and a two-way bystander could potentially only retrieve an accessible automated external defibrillator before emergency medical service in 31.1% (n=37) of cases. If a bystander only needed to travel one-way to bring an automated external defibrillator (≤100 m, ≤250 m and ≤500 m), 45.4% (n=54/119), 37.1% (n=196/529) and 29.8% (n=350/1174) could potentially be reached before the emergency medical service based on current automated external defibrillator accessibility.
Few home arrests were reachable with an automated external defibrillator before emergency medical service if bystanders needed to travel from patient to automated external defibrillator and back. However, nearly one-third of arrests ≤500 m of an automated external defibrillator could be reached before emergency medical service arrival if the bystander only needed to travel one-way from the automated external defibrillator to the patient.
Introduction
Early defibrillation by an automated external defibrillator (AED) is associated with survival rates >50% for out-of-hospital cardiac arrests (OHCAs) in public.1,2 Consequently, public access defibrillation (PAD) programmes are recommended in international resuscitation guidelines,3,4 and have been implemented in several countries.5,,–8 Though rates of bystander defibrillation have improved in public locations,5,9,10 they have remained stagnant at around 1% in home arrests where ≈75% of cardiac arrests occur.5,11,,–14 A strategy of placing AEDs into private homes of individuals with a high-risk of cardiac arrest has not been shown to improve either early defibrillation rates or outcomes.15 Therefore, new strategies to improve bystander defibrillation in home arrests are warranted, since the absolute number of patients who collapse from shockable heart rhythm in home settings still outnumbers the corresponding number in public despite the lower rate of shockable heart rhythm.12,16
Prior to the introduction of smartphone applications (apps) that allow locating and activating citizen first-responders,8,17,–19 the only possibility for the emergency medical service (EMS) to guide bystanders to the nearest AED was for the dispatcher to identify a nearby accessible AED and guide bystanders on-site to retrieve the AED and run back (a ‘two-way travel strategy’). However, retrieval of an AED using this strategy rarely occurs in practice,20,–22 with reported referral rates to the nearest accessible AED in 1.2%20 and 2.8%21 of cases, respectively. With the introduction of new smartphone technology it is now possible to activate nearby citizen first-responders to fetch and bring a nearby AED to the location of arrest before EMS arrival (a ‘one-way travel strategy’).8,18,19,23 Implementing such a system has the potential to broaden the concept of PAD programmes since AEDs can then be reached by citizen first-responders coming from another location, thus expanding the potential radius between AED and cardiac arrest that still allows a citizen first-responder to reach home arrests with an AED prior to EMS arrival. Such citizen first-responder systems are rapidly evolving and have been implemented in several countries.8,17,–19,23 These could especially be of great value for home arrests where it is often the case that only one bystander is present, and this bystander needs to stay with the patient and provide cardiopulmonary resuscitation (CPR).
The aim of this study was to explore the potential to reach publicly available AEDs for home arrests by examining: (a) the current AED coverage and accessibility according to distance from home arrests to nearest AED, and (b) the degree to which citizen first-responder programmes could improve bystander defibrillation before EMS arrival by comparing the proportion of home arrests potentially reachable with an AED if bystanders needed to travel back and forth from arrest location to an AED (a ‘two-way strategy’) versus travelling only one-way from an AED location to the arrest location (a ‘one-way strategy’).
Methods
Study setting
The city of Copenhagen has a resident population of ≈600 000 and covers ≈97 km2. Copenhagen is serviced by a two-tiered EMS system with ambulances equipped with AEDs providing basic life support and a physician-staffed ambulance providing advanced life support. In the event of a cardiac arrest, both tiers are simultaneously activated from the emergency medical dispatch centre.24,–26 During the study period in the present study no first-responder programmes (for neither trained/untrained citizens, police/firefighters) were yet tested or implemented in Copenhagen.
The Danish AED Network
The Danish AED Network was established in 2007 with voluntary registration viewable through a public webpage and a smartphone app. Since 2011, all emergency medical dispatch centres have been able to identify the nearest accessible AED during cardiac arrest calls.5,24,–26 We included all AEDs available for PAD in the city of Copenhagen (2007–2016) with the following information per AED: date of registration, exact address and coordinates of AED placement, organization owning the AED, and exact days and hours of AED accessibility. AEDs placed in residential locations were defined as AEDs deployed in private/nursing homes, elderly housing/activity centres, housing associations, apartments and homes with housing support. AEDs placed in public locations included AEDs deployed in companies/offices, school/education facilities, sports facilities, shopping malls/shops/banks, unions/associations, attraction/recreational areas, health clinics, public buildings, churches/community centres, hotels/ conference venues, transportation facilities and other public spaces.26
Study design and population
This was a retrospective observational cohort study of cardiac arrests, and registered AEDs with the Danish AED Network. Cardiac arrest data in the Copenhagen area has been systematically collected following the Utstein criteria since 1994 and has previously been described in detail.12,25 We identified all non-EMS witnessed cardiac arrests of presumed cardiac cause in homes with known locations and addresses in the city of Copenhagen (2008–2016). We included the following cardiac arrest variables: date and time of arrest; location of arrest; initial cardiac rhythm (non-shockable rhythm or shockable rhythm); time from dispatch of vehicle to arrival at scene (EMS response time); and whether bystander performed CPR and/or defibrillated the patient before EMS arrival. Home arrest locations included private/senior/nursing homes, while public cardiac arrest locations encompassed all areas accessible to the general population, including all outdoor locations, public transportation sites, educational institutions, outpatient clinics, and commercial and civic establishments.12,25 Time of arrest was divided into three periods of time: daytime (08:00–15:59), evening (16:00–23:59), and night-time (00:00–07:59).25,27 Data on 30-day survival was obtained from the Danish Central Population Registry.
Calculated distances and AED coverage
AED coordinates were retrieved from the AED network, while coordinates for home arrests were defined by the address of occurrence. We calculated route distances from each home arrest to AEDs via the road/pedestrian streets, using the network analyst feature in ArcMap 10.5.26 An AED had to have been placed before the date of arrest to be included, and we assessed if the AED was accessible or not at the time of arrest. AED coverage of home arrests was investigated within different distance intervals (home arrests ≤100 m, ≤250 m, ≤500 m of an AED). The distance groups were not exclusive, thus, AEDs ≤100 m were also included in the group ≤250 m, and so on. Loss of AED coverage of home arrests due to AED inaccessibility was examined by determining the difference between AED coverage irrespective of AED accessibility and the time of day at which the cardiac arrest occurred.25 This was further stratified according to AED location type.
AEDs reachable prior to EMS arrival
The proportion of home arrests that could potentially be reached with an AED before EMS arrival was investigated for home arrests covered by an accessible AED (≤100 m, ≤250 m, and ≤500 m) at the time of arrest. Within each distance category the following response times were assessed: (a) EMS response time, (b) response time of a bystander if the bystander had to travel two-ways to retrieve an AED and bring it back to the patient (a ‘two-way bystander’), and (c) response time of a bystander if the bystander only needed to travel one-way to bring an AED (a ‘one-way bystander’). The EMS response time (time from dispatch of vehicle to arrival at the scene of home arrest) was derived from the time from vehicle dispatch (automated, electronically registered by the dispatch system) and the time of vehicle arrival at the scene (registered by the Copenhagen mobile emergency care unit physician for every case where a cardiac arrest is suspected). To assess the response time for a potential ‘two-way’ and ‘one-way’ bystander we calculated the real route distances from each home arrest to the nearest AED (thus, not straight-line distance) and then used a walking speed of 2 m/s (7.2 km/h) to calculate walking time. A similar ‘brisk walking speed’ has been documented among recreational walking adults,28 and similar29,30 and faster18 walking speeds have been used in earlier published articles regarding citizen responder speed in out-of-hospital cardiac arrest. To the best of our knowledge, there are no published data on the time it takes a dispatcher to guide a bystander present at an arrest location to find a nearby AED, remove the AED and bring it back. In addition, a possible ‘one-way’ bystander will most likely not be present exactly at the AED location when activated. To account for this, and make our findings comparable with the existing literature, we included similar time estimates to our retrieval times estimates as recently published in another study addressing this aspect (the study defined removal of an AED from the cabinet as one minute, and the time it would take to pass the AED location details to a bystander by the dispatcher as two minutes).30 We added two minutes to a potential ‘one-way’ bystander (added time to reach an AED location from the location where a citizen first-responder would receive the alarm) as activation of a ‘one-way’ bystander theoretically would be executed faster (simultaneously as activation of the EMS from the dispatch centre) compared to the potential time it would take for the dispatcher to guide a potential ‘two-way’ bystander at the scene of a home arrest to a nearby AED location and then back to the patient (therefore an additional three minutes for a potential ‘two-way’ bystander). During the conduction of the present study, a study from Switzerland (investigating the distance covered by lay first-responders activated for cardiac arrest) reported that the lay first-responders in their study would have reached the nearest AED after an average time of 58 s (interquartile range (IQR) 30–105 s).17 The vast majority of the citizen first-responders (comparable to a ‘one-way’ bystander in our study) in the study from Switzerland used a vehicle to reach the cardiac arrest site instead of running/walking at a brisk speed. Accordingly, the total retrieval time for a potential ‘two-way’ bystander in our study was: two-way walking time (from home arrest to the nearest AED and back), plus three minutes for the dispatcher to guide the bystander to the AED location and back, and one minute for the bystander to remove the AED; and the total retrieval time for a potential ‘one-way’ bystander was: one-way walking time (from AED to the home arrest location), plus two minutes for the bystander to reach the AED location (from the location where the citizen responder received the alarm and to the nearest AED), and one minute for the bystander to remove the AED. Cases with missing information on EMS response time were excluded from the analyses (1.1% of the total study population).
Statistics
For analyses on the proportion of home arrests potentially reachable before EMS by bystander activation strategy we assumed that the incidence of arrests followed the Poisson distribution, and confidence intervals (CIs) were calculated accordingly. Logistic regression was performed to examine the association between bystander defibrillation and 30-day survival with crude and adjusted results presented as odds ratios (ORs) with 95% CIs. All analyses were performed using SAS (statistical version 9.4, SAS institute Inc., North Carolina, USA).
Ethics
The Danish Data Protection Agency (Ref. no. 2007-58-0015, local ref. no. GEH-2014-107, I-Suite no. 02735) approved this study. In Denmark, no ethical approval is required for retrospective registry studies.
Results
We identified 1879 non-EMS witnessed arrests of presumed cardiac cause which occurred in homes (2008–2016) (Figure 1), and 1830 publicly available registered AEDs in the city of Copenhagen (2007–2016).
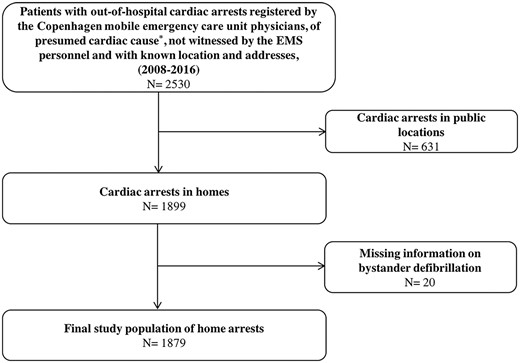
Patient selection.
EMS: emergency medical service.
*Cardiac arrest of presumed non-cardiac cause (arrests due to trauma, suicide, poisoning, drowning and exsanguination, or if the patient was judged to be terminally ill by the physician at the scene) were not included.
Characteristics of home arrests, bystander defibrillation and 30-day survival
More than 50% of home arrests occurred during the evening and night-time (n=1040), and 2.1% (n=40) received bystander defibrillation before EMS arrival. Bystander-defibrillated home arrests were more likely to be witnessed by bystander (82.5% vs 52.5%), receive bystander CPR (61.5% vs 41.2%), and achieve 30-day survival (27.5% vs 8.6%), compared to home arrests not defibrillated by bystander (Table 1). Among those not bystander-defibrillated, 15.7% had a shockable heart rhythm at EMS arrival. Bystander defibrillation was positively associated with achieving 30-day survival (OR: 2.62 (95% CI 1.18–5.81) adjusted for age, sex, bystander-witnessed status and whether bystander CPR was initiated) (Supplemental Material eFigure 1). Age, sex and median EMS response time were stable within each distance interval to the nearest AED, as were the proportion of patients whose arrest was witnessed by a bystander, who received bystander CPR, and who had a shockable heart rhythm (Supplemental Material eTable 1).
| . | Cardiac arrest, total, n (%) . | Bystander defibrillation, n (%) . | No bystander defibrillation, n (HA) . |
|---|---|---|---|
| 1879 (100.0) | 40 (2.1) | 1839 (97.9) | |
| Median age, years (IQR) | 72 (61–82) | 71 (55–77) | 72 (61–83) |
| Male, years (IQR) | 69 (59–79) | 68 (53–74) | 69 (59–79) |
| Female, years (IQR) | 75 (64–86) | 76 (68–79) | 75 (64–86) |
| Male, n (%) | 1085 (58.0) | 26 (65.0) | 1059 (57.9) |
| Median EMS response time,a min | 5 (4–7) | 6 (4–7) | 5 (4–7) |
| (IQR) | |||
| Shockable heart rhythm, n (%) | 328 (17.5) | 40 (100.0) | 288 (15.7) |
| Bystander witnessed arrest, n (%) | 993 (53.1) | 33 (82.5) | 960 (52.5) |
| Bystander CPR, n (%) | 775 (41.7) | 24 (61.5) | 751 (41.2) |
| 30-Day survival,bn (%) | 167 (9.0) | 11 (27.5) | 156 (8.6) |
| . | Cardiac arrest, total, n (%) . | Bystander defibrillation, n (%) . | No bystander defibrillation, n (HA) . |
|---|---|---|---|
| 1879 (100.0) | 40 (2.1) | 1839 (97.9) | |
| Median age, years (IQR) | 72 (61–82) | 71 (55–77) | 72 (61–83) |
| Male, years (IQR) | 69 (59–79) | 68 (53–74) | 69 (59–79) |
| Female, years (IQR) | 75 (64–86) | 76 (68–79) | 75 (64–86) |
| Male, n (%) | 1085 (58.0) | 26 (65.0) | 1059 (57.9) |
| Median EMS response time,a min | 5 (4–7) | 6 (4–7) | 5 (4–7) |
| (IQR) | |||
| Shockable heart rhythm, n (%) | 328 (17.5) | 40 (100.0) | 288 (15.7) |
| Bystander witnessed arrest, n (%) | 993 (53.1) | 33 (82.5) | 960 (52.5) |
| Bystander CPR, n (%) | 775 (41.7) | 24 (61.5) | 751 (41.2) |
| 30-Day survival,bn (%) | 167 (9.0) | 11 (27.5) | 156 (8.6) |
AED: automated external defibrillator; CPR: cardiopulmonary resuscitation; EMS: emergency medical service; IQR: interquartile range.
Number of missing: age (n=16), sex (n=9), response time (n=21), bystander witnessed status (n=10), bystander CPR (n=19).
Time from dispatch of vehicle to arrival at scene.
29 Arrests excluded due to missing information on 30-day survival.
| . | Cardiac arrest, total, n (%) . | Bystander defibrillation, n (%) . | No bystander defibrillation, n (HA) . |
|---|---|---|---|
| 1879 (100.0) | 40 (2.1) | 1839 (97.9) | |
| Median age, years (IQR) | 72 (61–82) | 71 (55–77) | 72 (61–83) |
| Male, years (IQR) | 69 (59–79) | 68 (53–74) | 69 (59–79) |
| Female, years (IQR) | 75 (64–86) | 76 (68–79) | 75 (64–86) |
| Male, n (%) | 1085 (58.0) | 26 (65.0) | 1059 (57.9) |
| Median EMS response time,a min | 5 (4–7) | 6 (4–7) | 5 (4–7) |
| (IQR) | |||
| Shockable heart rhythm, n (%) | 328 (17.5) | 40 (100.0) | 288 (15.7) |
| Bystander witnessed arrest, n (%) | 993 (53.1) | 33 (82.5) | 960 (52.5) |
| Bystander CPR, n (%) | 775 (41.7) | 24 (61.5) | 751 (41.2) |
| 30-Day survival,bn (%) | 167 (9.0) | 11 (27.5) | 156 (8.6) |
| . | Cardiac arrest, total, n (%) . | Bystander defibrillation, n (%) . | No bystander defibrillation, n (HA) . |
|---|---|---|---|
| 1879 (100.0) | 40 (2.1) | 1839 (97.9) | |
| Median age, years (IQR) | 72 (61–82) | 71 (55–77) | 72 (61–83) |
| Male, years (IQR) | 69 (59–79) | 68 (53–74) | 69 (59–79) |
| Female, years (IQR) | 75 (64–86) | 76 (68–79) | 75 (64–86) |
| Male, n (%) | 1085 (58.0) | 26 (65.0) | 1059 (57.9) |
| Median EMS response time,a min | 5 (4–7) | 6 (4–7) | 5 (4–7) |
| (IQR) | |||
| Shockable heart rhythm, n (%) | 328 (17.5) | 40 (100.0) | 288 (15.7) |
| Bystander witnessed arrest, n (%) | 993 (53.1) | 33 (82.5) | 960 (52.5) |
| Bystander CPR, n (%) | 775 (41.7) | 24 (61.5) | 751 (41.2) |
| 30-Day survival,bn (%) | 167 (9.0) | 11 (27.5) | 156 (8.6) |
AED: automated external defibrillator; CPR: cardiopulmonary resuscitation; EMS: emergency medical service; IQR: interquartile range.
Number of missing: age (n=16), sex (n=9), response time (n=21), bystander witnessed status (n=10), bystander CPR (n=19).
Time from dispatch of vehicle to arrival at scene.
29 Arrests excluded due to missing information on 30-day survival.
AED coverage and accessibility
AED coverage according to distance to the nearest AED (≤100 m, ≤250 m and ≤500 m) was 6.3% (n=119), 28.4% (n=533) and 63.1% (n=1185), respectively. AED coverage nearly halved within each distance interval due to AED inaccessibility at the time of arrest (3.6% (n=67) ≤100 m, 14.3% (n=269) ≤250 m, 39.6% (n=745) ≤500 m) (Supplemental Material eTable 1). AED coverage loss due to AED inaccessibility was markedly greater during the evening and night-time compared to daytime (Supplemental Material eFigure 2).
Among home arrests ≤100 m of an AED, most were covered by AEDs deployed at companies/offices (21.9%) followed by residential locations (17.7%), schools/education facilities (15.1%), sports facilities (12.6%) and health clinics (9.2%). Accounting for AED accessibility, AEDs in residential locations had the lowest coverage loss (4.8%) while schools/education facilities and sports facilities had the highest coverage loss (≈60%), followed by health clinics (54.5%) and companies/offices (34.6%). Within 250 m and 500 m of an AED, most AEDs covering home arrests were deployed in public locations and these AED location types experienced a coverage loss ranging from 24.7–75.0% due to AED inaccessibility (Supplemental Material eTable 2).
Proportion of arrests reachable with an AED prior to EMS arrival
The median distance from home arrests to nearest accessible AED (≤100 m, ≤250 m and ≤500 m) was 61 m (IQR: 38–84 m), 162 m (IQR: 100–209 m) and 310 m (IQR: 202–410 m), respectively. The median response time for EMS was five minutes (IQR: 4–7 min) within each distance category. The median response time for a one-way and two-way bystander strategy compared to EMS response time (≤100 m, ≤250 m and ≤500 m to nearest accessible AED) is shown in Figure 2.
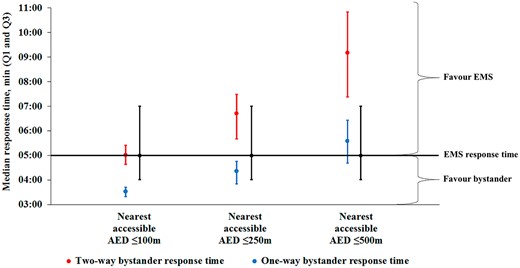
Median response time for a two-way or one-way bystander strategy compared to emergency medical service (EMS) response time.
The median response time for EMS, a two- and one-way bystander according to the nearest accessible automated external defibrillator (AED) ≤100 m, ≤250 m, and ≤500 m. Median time in minutes with 25th percentile (Quartile 1 (Q1)) and 75th percentile (Quartile 3 (Q3)).
Of all home arrests with an accessible AED ≤100 m, only 31.1% (n=37/119) of these AEDs could potentially be retrieved before EMS arrival by a bystander that needed to travel from the home arrest location and then back to the patient. However, a bystander that only needed to travel one-way could potentially reach the patient with an accessible AED before EMS arrival in 45.4% (n=54/119), 37.1% (n=196/529) and 29.8% (n=350/1174) of cases for distances of ≤100 m, ≤250 m and ≤500 m, respectively (Figure 3).
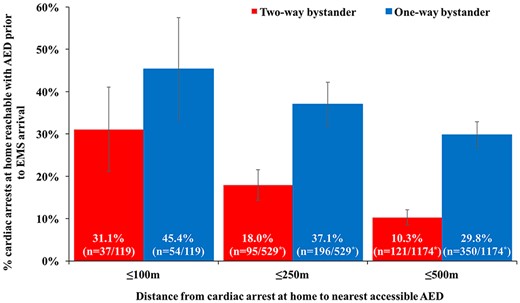
Proportion of home arrests potentially reachable with an automated external defibrillator (AED) prior to emergency medical service (EMS) arrival according to bystander activation strategy.
Error bars represents 95% confidence intervals based on the assumption that the incidence of home arrests followed the Poisson distribution.
*Due to missing values on EMS response time for home arrests covered by an AED ≤250 m and ≤500 m, four cases that had an AED ≤250 m and 11 cases that had an AED ≤500 m were excluded from analysis.
Discussion
This study examined the potential benefit of PAD for home arrests according to AED coverage and different bystander activation strategies. The study had three main findings. First, current AED coverage of home arrests was very low ≤100 m (6.3%), which may partly explain why only 2.1% of all cases are currently bystander-defibrillated before EMS arrival. Second, a two-way bystander could potentially only retrieve an accessible AED ≤100 m before EMS in 31.1% (n=37) of cases. Third, if bystanders only needed to travel one-way to bring an accessible AED to the arrest location (a ‘one-way travel strategy’ as when implementing citizen first-responder programmes), a markedly higher proportion of cases could potentially be reached before EMS arrival, namely 45.4%, 37.1% and 29.8% of cases within ≤100 m, ≤250 m and ≤500 m of an accessible AED, respectively. These findings indicate that implementing citizen first-responder programs utilising ‘one-way travel strategies’ may markedly increase the proportion of cardiac arrest patients at home that can be defibrillated prior to EMS arrival.
Our study presents novel and important findings to understand the currently low rates of bystander defibrillation in home arrests. We found only 6.3% of all home arrests were ≤100 m of an AED at the time of arrest. Taking AED accessibility and EMS response time into account, only 31.1% could be reached by an accessible AED ≤100 m at the time of arrest prior to EMS if bystanders needed to travel to the AED location and back to the patient. Contrary to cardiac arrests in public, patients at home often have only one bystander at their side and this bystander needs to stay with the patient and provide CPR. Even in the case of multiple bystanders, referral to a nearby AED by the medical dispatcher is reported to occur in only 1–4% of cardiac arrests.20,21 Another strategy of placing AEDs into private homes of individuals with a high-risk of sudden cardiac arrest was examined in the large Home Access Defibrillation Trial,15 which failed to improve early defibrillation and survival rates for cardiac arrests in private homes. This was to some extent explained by a very low rate of arrest events in the trial and a high proportion of arrests being unwitnessed or outside the patient’s home. An alternative and possibly more promising strategy could be to place AEDs accessible to all citizens within a residential area, whereby these AEDs could cover multiple cardiac arrests within the given area instead of only covering those individuals in a defined household.12 In Holland, bystanders have been recruited using a text-message system,8 thereby decreasing time to defibrillation (on an average, text-message responders defibrillated cardiac arrest cases two minutes and 39 s earlier than the EMS). In Sweden, a similar text-message system has been shown to increase the proportion of patients receiving bystander CPR.31 The same Swedish group has implemented a smart phone app system using the same app as the one now implemented in Denmark.23 In this context, our results are particularly promising. With citizen first-responder programmes, AEDs could potentially be fetched within longer distances instead of the traditional 100 m covering very few home arrests in our study. Even though a median EMS response time of only five minutes was observed in Copenhagen, nearly 30% of home arrests occurring ≤500 m of an accessible AED could potentially be reached with an AED before EMS arrival if a bystander only had to travel one-way. In home arrest areas with longer EMS response times, the proportion of cases potentially reachable before EMS may be even greater (Figure 2). A recent study from the UK analysed the total retrieval time from public and residential arrests to an AED (thus, one-way retrieval and not stratified by location of arrest) and reported that an AED could be retrieved before EMS arrival in 25.3% of all arrests.30 The higher proportions found in the present study can be explained by the much higher AED density in Copenhagen of 18.9 AEDs/km2 vs 0.23 AEDs/ km2 in the study from the UK. In the Netherlands, recent data on a citizen first-responder system has shown especially promising results in home arrests where 87.5% of all AEDs were used in these settings.8 The effect on bystander defibrillation and 30-day survival of using these systems has yet to be determined.8,19,32 However, we found that 27.5% of home arrests achieved 30-day survival if bystander-defibrillated which is in accordance with nationwide Danish data from 2012,5 and among home arrests that were not bystander-defibrillated 15.7% still had a shockable heart rhythm at EMS arrival. Furthermore, the maximum distance between citizen first-responders and cardiac arrest locations is currently unknown, but these distances are currently being investigated in clinical trials (the HeartRunner Trial (ClinicalTrials.gov Identifier: NCT03835403)).
Unfortunately, more than half of home arrests lost AED coverage due to limited AED accessibility at the time of arrest, which is a substantially higher coverage loss than that found amongst public arrests.25,27 Comparable with public arrests,25,27 coverage loss was highest during the evening and night-time, stressing the need for 24/7 (24 h per day, seven days per week) AED accessibility. Within 100 m, many home arrests were covered by AEDs placed specifically in residential locations (with good AED accessibility),26 whereas within longer distances, most arrests were covered by AEDs in public locations with low accessibility. Our findings indicate efforts are needed to widen the common definition of PAD to not only include arrests in public locations but also include improvement strategies for home arrests.33,34 However, even though citizens first-responder programmes may be a valuable strategy for home arrests, this may not be straightforward in all communities due to local ethical aspects or legislation.35,36 Good Samaritan laws may help in overcoming some of these obstacles.36 Another option is activation of off-duty police/firefighters as shown to be possible in King County, USA.13
Limitations
We only had information on publicly available AEDs registered within the Danish AED Network whereas there may be additional unregistered AEDs which could have been used for bystander defibrillation. However, the overall rate of defibrillation in home arrests was very low, and unregistered AEDs have previously been found to be less likely to be used,7 hence unlikely to influence our results. We only had information on bystander defibrillation and not AED applied but no shock given. Thus, AED use in home arrests is potentially higher than the reported 2% in the present study since the majority of home arrest patients have a non-shockable heart rhythm.12,16 Furthermore, due to the very low number of cases who were bystander defibrillated ≤100 m, ≤250 m and ≤500 m, it was not possible to do meaningful analyses of home arrest survival according to distance (Supplemental Material eTable 1). Overall, the aim of the present study was not to investigate potential change in outcomes by using different bystander activation strategies as this probably would require a randomised trial. There are currently no studies that document the survival benefit of activating nearby citizen first-responders in communities.19,32 However, by activating voluntary citizens, one can potentially shorten the time to starting CPR and use of AEDs before ambulance arrival, which is associated with increased survival.37 Lastly, the study setting was the city of Copenhagen which is an urban area with better AED coverage than rural areas.30 Therefore, results on AED coverage and response times may not be applicable to all cities and communities, but we believe that the main findings in this study are valuable for all communities seeking to improve early defibrillation in home arrests.
Conclusions
Few home arrests with an accessible AED ≤100 m were reachable prior to EMS if bystanders needed to travel from the patient to the AED and back. However, implementation of citizen first-responder strategies where a bystander only needs to travel one-way (from AED location to the patient) holds the potential to significantly increase the AED coverage distance of home arrests and thereby bystander defibrillation before EMS arrival.
The authors wish to thank the Danish AED Network for sharing information regarding AEDs registered in the network, and the EMS personnel that collected and reported information to the OHCA database. They also want to acknowledge and thank Kirstine Wodschow, from the University of Southern Denmark, National Institute of Public Health, for help and advice in performing the geocoding of OHCAs and distance calculations.
The authors declare that there is no conflict of interest.
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by The Danish Foundation TrygFonden. TrygFonden had no part in the design of the study; collection, analysis, and evaluation of data; writing and review of the manuscript; and final decision of the manuscript to be submitted for publication.
Supplemental material for this article is available online.




Comments