-
PDF
- Split View
-
Views
-
Cite
Cite
T Thevathasan, A Freund, U Zeymer, J Poess, T Ouarrak, S Schneider, H Thiele, S Desch, ECLS-SHOCK, ECMO-related complications and mortality in patients with infarct-related cardiogenic shock, European Heart Journal. Acute Cardiovascular Care, Volume 14, Issue Supplement_1, April 2025, zuaf044.167, https://doi.org/10.1093/ehjacc/zuaf044.167
Close - Share Icon Share
Abstract
Recent randomised controlled trials, along with a meta-analysis of individual patient data, have demonstrated that the routine application of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) does not confer a survival benefit over standard medical therapy in patients experiencing acute myocardial infarction complicated by cardiogenic shock (AMI-CS).
This study sought to determine whether potential complications specifically associated with VA-ECMO might contribute to an elevated risk of mortality, possibly explaining the similar mortality outcomes observed between patients receiving VA-ECMO and those managed with conventional therapy in cases of AMI-CS.
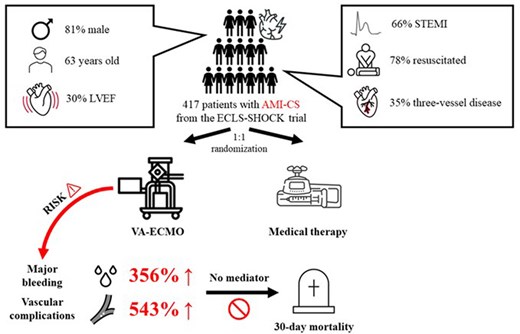
Data was sourced from the ECLS-SHOCK trial, a randomised study comparing routine VA-ECMO implementation to medical therapy alone in infarct-related cardiogenic shock. The study employed causal mediation analyses, using VA-ECMO-related complications as a mediator in primary analyses (Figure 1), alongside logistic regression and analyses of death causality as secondary analyses. These analyses examined the impact of VA-ECMO-related complications on 30-day mortality, with adjustments made for bleeding and vascular complication risk factors.
This analysis included a total of 417 patients (Figure 2). VA-ECMO-related complications were identified, particularly moderate to severe bleeding and peripheral vascular complications necessitating intervention. Out of the study population, 88 patients (21.1%) experienced complications likely attributable to VA-ECMO, predominantly within five days post-randomisation, with higher occurrences in the VA-ECMO group compared to the control group: bleeding in 49 (23.4%) vs. 20 (9.6%) patients, p<0.001, and peripheral vascular complications in 23 (11.0%) vs. 8 (3.8%) patients, p=0.01. However, causal mediation analyses indicated no significant mediating effect of VA-ECMO-related complications on 30-day mortality (p=n.s.; Figure 2). Logistic regression and mortality causality analyses similarly identified no significant correlation between the presence of VA-ECMO-related complications and mortality (p=n.s.).

Author notes
Funding Acknowledgements: None.




Comments