-
PDF
- Split View
-
Views
-
Cite
Cite
G Tavazzi, C N J C Costanza, C F Corradi, C A Alviar, PEEP trial and effect on hemodynamic in cardiogenic shock, European Heart Journal. Acute Cardiovascular Care, Volume 13, Issue Supplement_1, April 2024, zuae036.149, https://doi.org/10.1093/ehjacc/zuae036.149
Close - Share Icon Share
Abstract
None.
Congestion is a paramount pathophysiological driver in patients with cardiogenic shock. Almost half of patients admitted due to cardiogenic shock undertake mechanical ventilation although ventilatory parameter, and their potential hemodynamic effect on the hemodynamic and congestion profile are often neglected.
We sought to evaluate the hemodynamic effect of positive end-expiratory pressure (PEEP) titration on patients admitted to intensive care unit for CS.
We perform PEEP titration trial on patients undertaking mechanical ventilation for respiratory failure related to CS. The trial consisted in 3 steps of PEEP increase from 5 to 15 cmH2O. For each step arterial saturation, right atrial -RAP- and systemic blood pressure along with heart rate and respiratory mechanics (tidal volume-TV-, dynamic lung compliance- CLdyn, driving- Δ- and plateau pressure- Ppl) were measured. All the measures were taken at end-expiration; RAP trace was analyzed and systolic, mean and diastolic component collected. The final PEEP was decided based on the best matching between saturation, CLdyn and TV. Descriptive and repeated measures with Bonferroni correction were applied as statistical analysis (IBM SPSS 29).
Twelve patients were included (10 male, 66 ± 7 years old; 8 acute myocardial infarction and 4 acute heart failure). At baseline the mean RAP was 8.44 (± 2.32) ; SBP 106 (IQR 92-112), HR 94 (IQR 88 - 102) Δ and Ppl pressures respectively 7.42 (± 0.79) and 12.08 (± 0.79, ),VT 427(± 65.42) and CLdyn 58.3 (± 7.1).
The right atrial pressure (RAP) differed between AMI and AHDF (8.25 ± 2.25 vs 20.25 ± 1.5; p < 0.001), so HR did (113 ± 3.4 versus 96 ± 3.2 betas per minutes; p 0.015).
RAP varied consistently during the PEEP trial (either sRAP, dRAP and mRAP- Table and Figure 1). The TV changed signficnatly between the 1st and 3rd step (p 0.004) and the CLdyn varied consistently throughout the 3 steps of the PEEP trial (p <0.001). A significant difference were observed according to aetiology in RAP (AMI Vs ADHF, eman difference 2.4 versus 4.3 mmHg) and in CLdyn (AMI Vs ADHF mean difference 12.31 vs 8 .65, p < 0.01) but not in the other parameters evaluated (p > 0.05).

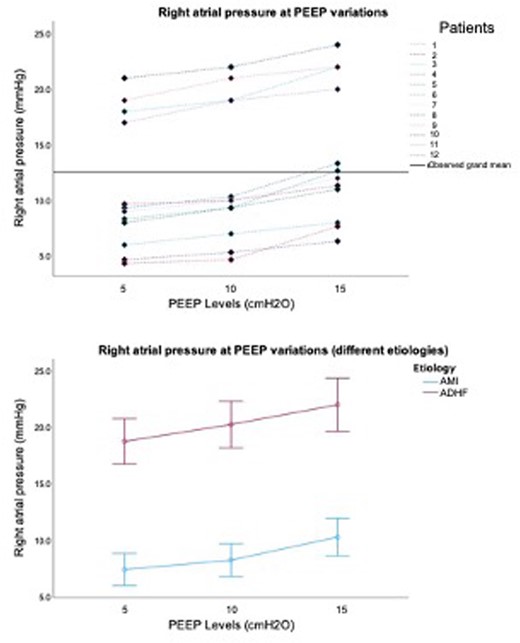
Graph PEEP vs RAP
- heart failure, acute
- myocardial infarction, acute
- phenotype
- hemodynamics
- hemodynamic measurements
- heart rate
- lung
- atrium
- cardiogenic shock
- right atrial pressure
- diastole
- intensive care unit
- positive end-expiratory pressure
- respiratory insufficiency
- respiratory mechanics
- systole
- arterial pressure
- pressure-physical agent
- graphical displays
- mechanical ventilation
- end-expiration
- acute decompensated heart failure
- causality
- titration method
- doppler hemodynamics
- mean right atrial pressure




Comments