-
PDF
- Split View
-
Views
-
Cite
Cite
Fabiana Duarte, Catarina Relvas Novo, Miguel Guerra, Answer: Multiple free-floating cardiac masses in a young woman with pulmonary embolism, European Heart Journal. Acute Cardiovascular Care, Volume 13, Issue 6, June 2024, Pages 519–520, https://doi.org/10.1093/ehjacc/zuae033
Close - Share Icon Share
This Spot the Diagnosis article refers to ‘Question: Multiple free-floating cardiac masses in a young woman with pulmonary embolism’, by F. Duarte et al., https://doi.org/10.1093/ehjacc/zuae032.
A 20-year-old female patient presented for a medical consultation due to chest pain and reduced exercise tolerance with 1-week duration. The patient denied alcohol consumption, tobacco, or illicit drug use and had no previous medical conditions. She was not taking any medications, including oral contraceptives. The physical examination was unremarkable. Biochemical evaluation revealed leucocytosis and elevated C-reactive protein, while the chest X-ray showed opacity in the lower right lung field. An initial diagnosis of community-acquired pneumonia was made, and empirical antibiotic therapy was initiated.
Upon medical re-evaluation, the patient continued to experience chest pain and reported a productive cough with haemoptysis. The patient’s vital signs remained stable. The electrocardiogram showed sinus tachycardia (Figure 1A). At that time, a computed tomography angiography was performed, revealing a subacute subsegmental pulmonary embolism (PE; Figure 1B and C). It was classified as a low-risk PE, and the patient was discharged under direct oral anticoagulation.
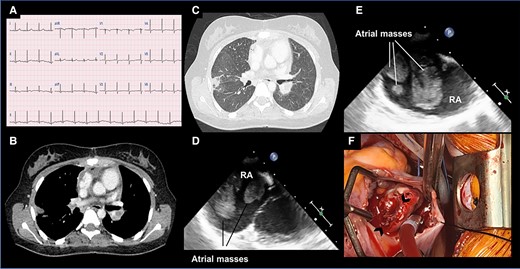
(A) 12-lead electrocardiogram demonstrates sinus tachycardia. (B, C) Axial chest computed tomography images reveal a subsegmental pulmonary embolism. (D, E) Transesophageal echocardiogram (0º and 90º, respectively) display multiple free-floating masses in the right atrium. (F) An intraoperative image depicts an open right atrium containing several pedunculated and sessile masses (indicated by arrowheads).
One day later, a transthoracic echocardiogram (TTE) revealed multiple echogenic masses with a round surface in the right atrium (RA). A transoesophageal echocardiogram confirmed the presence of multiform and free-floating masses in the RA, attached to the inferior region of interatrial septum (Figure 1D and E; see Supplementary material online, Videos S1 and S2). Due to the uncertainty of its nature and the concern for additional embolic events, urgent cardiac surgery was performed. Several pedunculated and sessile masses in the RA were removed through an atrial approach (Figure 1F; see Supplementary material online, Video S3).
In light of such clinical presentation, what is the next most important step in the diagnostic process?
Obtain sets of blood cultures before initiating antibiotic therapy.
Perform additional tests, including coagulation tests and histopathological examination.
Perform a thoracic–abdominal–pelvic computed tomography and, if necessary, a positron emission tomography (PET) scan.
Await histopathological examination of the mass before changing the treatment.
Answer: 2
Additional aetiological investigation revealed elevated coagulation tests, including activated partial thromboplastin time, lupus anticoagulant positivity, and moderate titres of IgG/IgM anti-B2-glycoprotein I and IgG/IgM anticardiolipin antibodies. Protein C/S and fibrinogen were within normal limits, and other rheumatological markers were negative.
Histological evaluation was consistent with a recent and partially organized thrombus. No malignant tissue was evident, and calretinin immunohistochemistry was negative. The hypothesis of cardiac myxoma was excluded.
The diagnosis of antiphospholipid syndrome (APS) was established, leading to a modification of the initial anticoagulant therapy from direct oral anticoagulation to a vitamin K antagonist. No additional vascular, cardiac, or haematologic complications were observed.
Despite an elevation in inflammatory markers, the patient remained afebrile, had no risk factors for endocarditis, and vegetations are typically irregular and attached to valvular structures, which was not the case here. Considering the patient’s age and sudden clinical presentation, the probability of a malignant condition was reduced, and cardiac metastases are also uncommon.
This case represents a particular scenario involving the abrupt onset of APS in a previously healthy young woman. While vascular complications have been documented, the coexistence of PE and intracardiac thrombus is uncommon, as is the need for urgent surgical intervention. However, surgery was deemed essential to prevent further life-threatening complications.
Supplementary material
Supplementary material is available at European Heart Journal: Acute Cardiovascular Care online.
Author contribution
F.D. and C.R.N. wrote the initial version of the manuscript. C.R.N. and F.D. conceived and developed the idea. M.G. reviewed the manuscript.
Funding
None declared.
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Author notes
Fabiana Duarte and Catarina Relvas Novo shared first authorship.
Conflict of interest: none declared.




Comments