-
PDF
- Split View
-
Views
-
Cite
Cite
Diego Araiza Garaygordobil, Diana Laura Alfaro-Ponce, Massive coronary artery ectasia in a patient with myocardial infarction, European Heart Journal. Acute Cardiovascular Care, Volume 11, Issue 3, March 2022, Pages e1–e2, https://doi.org/10.1093/ehjacc/zuab105
Close - Share Icon Share
A 63-year-old man without a relevant medical history presented to the emergency department with sudden-onset chest pain accompanied by diaphoresis. A 12-lead electrocardiogram demonstrated ST-segment elevation in V1–V3 and subtle ST-segment elevation in inferior leads, suggestive of a proximal right coronary artery (RCA) occlusion, and the patient was referred for primary percutaneous intervention.
During coronary angiography, diffuse massive coronary artery ectasia was found (Figure 1). Initial flow was TIMI-0 in the RCA and TIMI-2 in the left anterior descending/left circumflex coronary artery. Thrombus aspiration, balloon angioplasty, and placement of a drug-eluting stent in the RCA were performed.
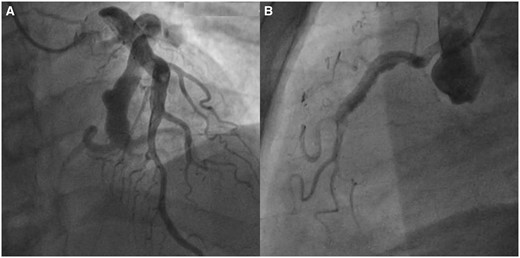
(A) Left coronary angiogram showing massive coronary artery ectasia of the LAD and Cx. (B) Right coronary angiogram showing coronary artery ectasia in the RCA and distal thrombus.
Coronary artery ectasia, defined as dilation greater than 1.5 times the diameter of the adjacent normal coronaries, can be either local or diffuse and is an uncommon finding in patients with acute coronary syndromes, with an estimated prevalence of 0.3–4.9%.1 In a recently published study, patients with coronary artery ectasia demonstrated a higher rate of major adverse cardiovascular events when compared with those without coronary ectasia (36.8% vs. 25.6%, P = 0.001) during a median follow-up of 4 years.2
In contrast to the classic atherosclerotic plaque, coronary artery ectasia is characterized by slow coronary flow prone to thrombus formation, coronary dilation, and positive arterial remodelling. In this case, which anti-thrombotic treatment would you recommend for the long-term prevention of recurrent ischaemic events?
Dual antiplatelet therapy.
No high-quality evidence exists for the selection of the optimal antithrombotic therapy in patients with coronary artery ectasia.
Triple antithrombotic therapy, including Vitamin K antagonists.
Triple antithrombotic therapy including direct oral anticoagulants.
Answer: 2
Coronary artery ectasia remains a treatment dilemma with respect to the optimal revascularization strategy and long-term anti-thrombotic treatment. Evidence arising from clinical cases suggests that oral anticoagulation may have a role in the prevention of recurrent ischaemic events.3 However, no evidence from randomized clinical trials exists and further research is needed.
Conflict of interest: none declared.




Comments