-
PDF
- Split View
-
Views
-
Cite
Cite
C Rubín De Célix, E Ricart, M D Martín-Arranz, R de Francisco, J Barrio, F Mesonero, F Gomollón, L de Castro, L Ramos, S García-López, L Arias, M Mañosa, E Iglesias, X Calvet, I Pascual, M J Casanova, J L Pérez-Calle, A Giordano, M Sierra, I Vera, M Navarro-Llavat, R Lorente, M Piqueras, M Rivero, J Guardiola, M Esteve, A Fuentes Coronel, I Rodríguez-Lago, Á Ponferrada, Y Ber, C Tardillo, L Márquez, D Carpio, C Taxonera, F Bermejo, D Busquets, B Camps, E Domènech, M Chaparro, J P Gisbert, on behalf of the ENEIDA project of GETECCU *Co-senior authorship, P844 Frequency and effectiveness of dose de-escalation of biologic therapy in Inflammatory Bowel Disease: The RAINBOW-IBD study of ENEIDA, Journal of Crohn's and Colitis, Volume 18, Issue Supplement_1, January 2024, Pages i1557–i1559, https://doi.org/10.1093/ecco-jcc/jjad212.0974
Close - Share Icon Share
Abstract
Background
Biologic dose escalation is associated with increased costs and potential safety concerns; therefore, de-escalation could be considered in patients in remission after dose escalation. However, data on de-escalation outcomes is scarce. Primary aim: To describe the frequency and the evolution after de-escalation of infliximab (IFX), adalimumab (ADA), golimumab (GOL), vedolizumab (VED), and ustekinumab (UST). Secondary: To investigate the durability of dose de-escalation, the factors associated with relapse after de-escalation, and the effectiveness of a re-escalation.
Methods
Adult patients from ENEIDA registry who previously had their biologic dose escalated, were included. De-escalations (either decreasing the dose or lengthening the interval of administration) were specifically analysed. Survival curves assessing the impact of several variables on clinical relapse were compared using the log-rank test. Predictive factors associated with the risk of relapse after dose de-escalation were assessed by Cox-regression.
Results
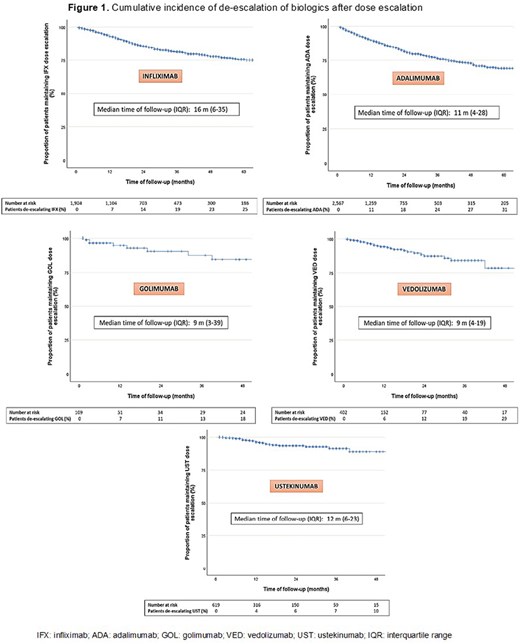
A total of 669 de-escalations from 5,096 previous dose escalations were performed (13%). The incidence rate of dose de-escalation per patient-year of follow-up was: 6% (95% confidence interval [CI]=5.8-6.2%), 9% (7.4-10.7%), 5% (1-9%), 6% (5.4-6.6%), and 3% (2.9-3.1%) in patients receiving IFX, ADA, GOL, VED and UST, respectively (Figure 1).
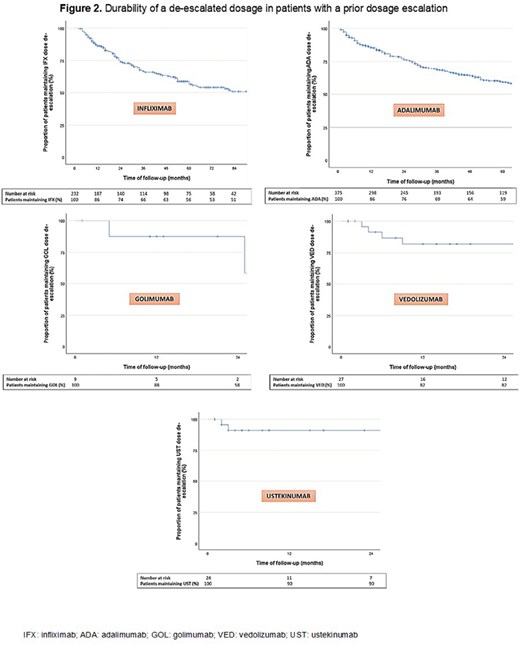
The favourable evolution after dose de-escalation (maintaining remission or response) was: 106/132 (80%) and 131/132 (99%) for IFX; 157/209 (75%) and 208/209 (99%) for ADA; 5/5 (100%) and 5/5 (100%) GOL; 14/16 (88%) and 16/16 (100%) for VED; and 9/12 (75%) and 11/12 (92%) for UST. The probability of maintaining the dose de-escalated at 12 months was: 86%, 86%, 88%, 82%, and 90% for IFX, ADA, GOL, VED and UST, respectively (Figure 2).
Predictive factors of relapse after de-escalation were as follows: 1) IFX: previous biologic exposure (Hazard ratio [HR]=2.7, 95%CI=1.1-6.9), and 2) ADA: age at dose de-escalation (HR=1.08, 95%CI=1.02-1.15). Variables associated with the risk of relapse with other biologics could not be identified. Response and remission were recaptured after re-escalation, respectively, in: 11/12 (92%) and 7/12 (58%) for IFX; 22/22 (100%) and 13/22 (59%) for ADA; 1/1 (100%) and 0/1 (0%) for GOL; 2/2 (100%) and 2/2 (100%) for VED; and 1/1 (100%) and 1/1 (100%) for UST.
Conclusion
In the largest cohort of patients with dose escalation of biologic treatment in real-life, approximately 10% of the patients have a dose de-escalation in the long-term. If carried out, the durability of the de-escalation seems to be high over time. In those who relapse after dose de-escalation, re-escalation of therapy is effective in more than half of the patients.