-
PDF
- Split View
-
Views
-
Cite
Cite
H Aleman Gonzalez, K Stamp, E Whitehead, A Pattinson, J Turnbull, S Myers, A Talbot, S Sebastian, P372 Accelerated dosing schedule with ustekinumab in anti-TNF refractory Crohn`s disease, Journal of Crohn's and Colitis, Volume 16, Issue Supplement_1, January 2022, Pages i374–i375, https://doi.org/10.1093/ecco-jcc/jjab232.499
Close - Share Icon Share
Abstract
The efficacy of ustekinumab in prior biologic exposed refractory patients with inflammatory bowel disease is significantly inferior to those who are bio naïve. The optimal therapeutic level and hence the optimal dosing strategy in this setting is uncertain. Whether early dose optimisation is beneficial in this group of patients has not been evaluated. We aimed to compare the effectiveness and safety of early dose optimisation for maintenance compared to conventional maintenance regime in a retrospective cohort of refractory IBD patients
All patients initiated on ustekinumab following failure of one or more anti-TNF agents were included. Patients who received conventional maintenance regime (Q8W) was compared to those who received accelerated maintenance regime (Q4H). The primary end point was steroid free remission at, 12 months or at last follow up. The secondary end points were ustekinumab persistence at, 6 months and, 12 months, need for surgery and drug related infectious or non-infectious complications
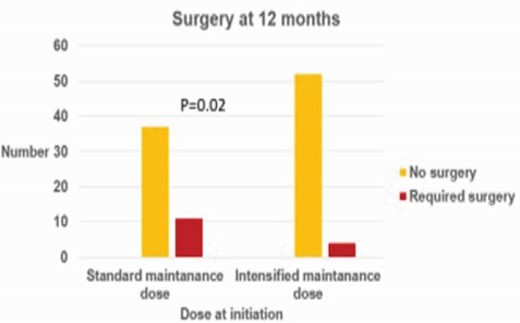
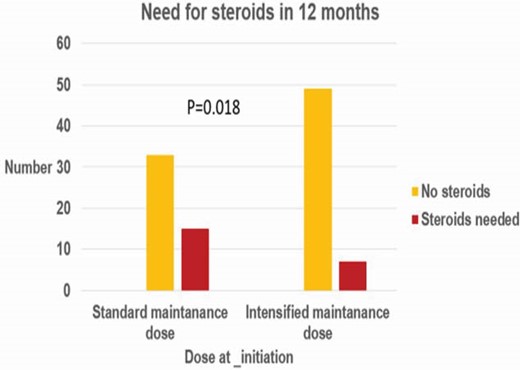
One hundred and four patients were included (male: female, 48:56). Median follow up was, 11 months (IQR, 5–14). Fifty-six patients received accelerated dosing regimen while, 48 patients received standard dosing regime. Dose escalation was required in, 18 patients (37.5%) of standard dosing regimen while four patients (7.1%) in the accelerated dosing regimen had dose de-escalation. Higher proportion patients in the accelerated dosing regimen were in steroid free remission, 87.5% vs, 68.8% (p=0.018). Proportion of patients requiring surgery was higher in the standard dosing regimen group (22.91, 5 vs, 7.14%, p = 0.02). Ustekinumab persistence in patient started on the accelerated regime and conventional dosing regime was not significantly different at, 6 months (94.1% and, 95.3%, p=0.58) and, 12 months (84.4% and, 95.3, p=0.1). No serious drug related complications observed in either group
Early dose optimisation of ustekinumab improves steroid free remission rates and reduces the need for surgery in patients with anti-TNF refractory patients with IBD



