-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Jones, Andrew Seely, Peter Grimminger, John Reynolds, Riccardo Rosati, George Hanna, Magnus Nilsson, Sheraz Markar, Richard van Hillegersberg, Mark van Berge Henegouwen, Suzanne Gisbertz, 561. COMMONALITY AND VARIATION IN PERIOPERATIVE ESOPHAGEAL CANCER MANAGEMENT IN HIGH VOLUME EUROPEAN CENTERS, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.286, https://doi.org/10.1093/dote/doae057.286
Close - Share Icon Share
Abstract
Esophageal cancer is a leading cause of cancer related death worldwide. For patients with locally advanced, non-metastatic, esophageal cancer (EC), surgical resection remains an essential pillar. The multitude of surgical options have driven innovation, however, lack standardization and at times high-quality data-driven practices. A surgeon-level in-depth interview and questionnaire was created to understand the perioperative care pathways and intraoperative techniques used by high-volume European EC centres to gain insight into commonality and variation of current practice.
Eight (8) expert upper gastrointestinal surgeons were invited to participate in an in-depth interview and questionnaire. The focus included preoperative care pathways for esophageal adenocarcinoma of the distal esophagus/GE junction, technical aspects of esophageal resection (Ivor-Lewis) and postoperative pathways. The involvement of allied health, dedicated research programs, multidisciplinary cancer conference (MCC), follow up protocols and management of T4b EC was also assessed.
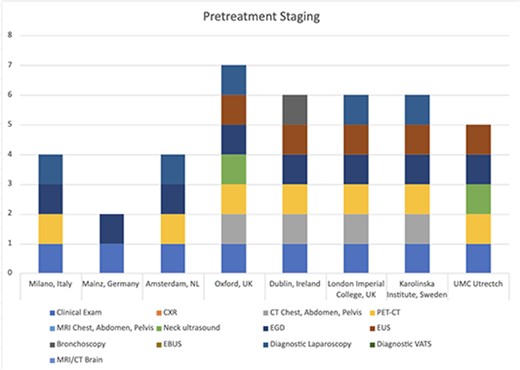
The response rate was 100% (8/8). Majority of respondents indicated a country-level regionalization of EC care. The number of centres performing esophageal resection varied from 4 – >100. Average number of esophagectomies/year ranged from 60-150. All centres presented EC patients at MCC, had dedicated research programs, and participated in National and International EC databases. Chemoradiotherapy was the predominate neoadjuvant treatment for GEJ cancers. Pretreatment clinical staging varied, with all centres having different, but pre-defined, preoperative and postoperative pathways. Intraoperative techniques including conduit preparation, feeding tube use, pyloric intervention, thoracic duct ligation and anastomotic technique varied substantially. There was no consensus regarding follow up or management of T4b EC.
The perioperative pathways and technical aspects of esophageal resection shared some commonalities however also differed substantially across high-volume EC centres in Europe. Multicenter, pragmatic randomized controlled trials (RCTs) are needed to better delineate which techniques should be included as standard of care, and which should be abandoned.