-
PDF
- Split View
-
Views
-
Cite
Cite
Ariadne Lisa Van Der Velden, Sam SI Bartz, Thomas A Vermeer, Kick JEM Bluijssen, Charlène J van der Zijden, Lotte Blonk, Evert-Jan G Boerma, Jan HMB Stoot, Suzanne S Gisbertz, Eric HJ Belgers, Bas PL Wijnhoven, Mathie PG Leers, Meindert N Sosef, Guy HEJ Vijgen, 407. MICRONUTRIENT INSUFFICIENCY AFTER SURGERY FOR OESOPHAGOGASTRIC NEOPLASMS: A PROSPECTIVE INTERVENTION STUDY CALLED THE VITAMIN STUDY, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.162, https://doi.org/10.1093/dote/doae057.162
Close - Share Icon Share
Abstract
Oesophageal and gastric cancer have major impact on nutritional status and quality of life (QoL). Preoperative malnutrition is reported in 42–80%. However, studies investigating postoperative nutritional status are scarce and postoperative identification and treatment of micronutritional deficiencies are currently lacking in (inter-)national guidelines. The aim of this study is to identify micronutrient deficiencies after surgery for oesophagogastric neoplasms and target them by supplementation.
This is a recently closed multicenter trial in the Netherlands. Patients receive a tailormade multivitamin supplement which differs per group and a calcium supplement. Baseline measurements consist of blood withdrawal, faecal elastase-1 (FE-1) analysis, QoL questionnaires and dietary behaviour. After 6 (T=1), 12 (T=2) and 24 (T=3) months from baseline, measurements are repeated, and a supplement questionnaire is added. The primary objective is micronutrient deficiency (yes/no). Secondary objectives include occurrence and symptoms of exocrine pancreas insufficiency (EPI) and QoL.
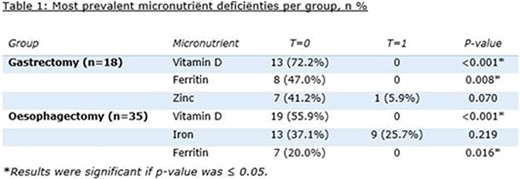
Inclusion spanned from December 2021 to December 2023. Preliminary results from 95 patients are available, whereby 68 patients underwent oesophagectomy and 27 gastrectomy. Of these, 55 patients received 6 months of supplementation (T=1). At T=0, 77.0% had at least one micronutrient deficiency. Identified deficiencies are shown in table 1. Deficiencies were more common in patients undergoing gastrectomy compared to those undergoing oesophagectomy (88.0% vs. 72.1%). Reduced FE-1 (<200 mg/kg) was found in 22.2% at baseline and 26.7% at T=1. 16.7% experienced EPI symptoms at baseline, which resolved at follow-up.
The most common micronutrient deficiencies decreased substantially after 6 months of supplementation. The follow-up extends until November 2024. Routine monitoring and supplementation could potentially be implemented in standard postoperative care for gastric and oesophageal cancer.