-
PDF
- Split View
-
Views
-
Cite
Cite
Thitiporn Chobarporn, Stephanie Wood, 369. IMPACT OF THE COVID-19 PANDEMIC ON ESOPHAGEAL CANCER PATIENTS UNDERGOING ESOPHAGECTOMY: AN ACS-NSQIP DATABASE ANALYSIS, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.128, https://doi.org/10.1093/dote/doae057.128
Close - Share Icon Share
Abstract
To cope with the increasing number of infected patients, medical access was restricted, and public facilities were closed throughout the COVID-19 pandemic. Early detection and treatment of esophageal cancer is critical for improved prognosis. However, the impact of pandemic-related medical access restrictions has not be evaluated to date for esophageal cancer. Therefore, the purpose of this research is to determine how the lockdown policy affected the surgical outcome of patients with esophageal cancer.
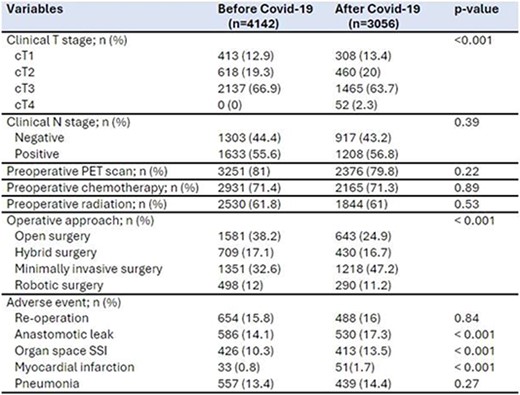
We analyzed patients who underwent esophagectomy for esophageal cancer between 2016-2022 using data obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), including the procedure targeted esophagectomy database. The patients were stratified into two groups based on their operation date relative to pandemic (BEFORE COVID group: 2016-2019 vs AFTER COVID group: 2020-2022). Demographic data and perioperative outcomes were compared between the two groups. Statistical analysis included Chi-square tests for categorical variables and independent student T-tests for continuous data, with a significance threshold set at p < 0.05.
Between 2016-2022, 7,198 esophageal cancer patients underwent esophagectomy. Clinical T4 increased significantly, but clinical N and pathologic T and N stages showed no impact. PET scan imaging, neoadjuvant chemotherapy and radiotherapy remained unchanged. The utilization of a minimally invasive approach rose substantially from 32.6% to 47.2% (p < 0.001). Positive margin rates increased from 7.5% to 9% (p = 0.03), and anastomotic leak rates increased from 14.1% to 17.2% (p < 0.001). Operative time, blood loss, and conversion rate showed no significant differences. Perioperative complications, including organ space surgical site infections and myocardial infarctions, significantly increased after COVID-19.
The COVID-19 pandemic altered the clinical staging of esophageal cancer patients undergoing esophagectomy, but it did not disrupt access to essential investigations and treatment. A notable increase in the implementation of minimally invasive techniques was observed after the pandemic. However, significant impacts were noticed on operative outcomes, including positive margin and leak rates.