-
PDF
- Split View
-
Views
-
Cite
Cite
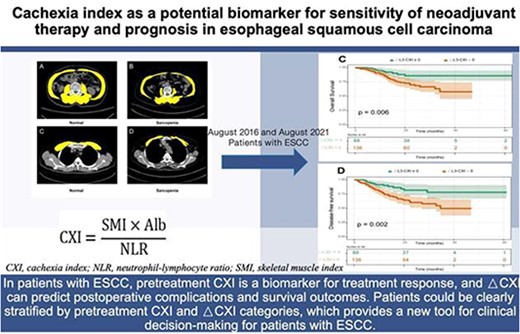
Pinhao Fang, Jianfeng Zhou, Yong Yuan, 240. CACHEXIA INDEX AS A POTENTIAL BIOMARKER FOR SENSITIVITY OF NEOADJUVANT THERAPY AND PROGNOSIS IN ESOPHAGEAL SQUAMOUS CELL CARCINOMA, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.025, https://doi.org/10.1093/dote/doae057.025
Close - Share Icon Share
Abstract
Cancer cachexia has a negative impact on the clinical outcome of patients with esophageal squamous cell carcinoma (ESCC). The cachexia index (CXI) is a potential biomarker for cancer cachexia, whereas its implications for ESCC prognosis and treatment outcomes have not been investigated.
In our study, 454 ESCC patients who had neoadjuvant therapy followed by surgery were included. Based on the exclusion criteria, a total of 224 patients were finally enrolled in this study. The CXI was determined as the serum albumin/neutrophil-lymphocyte ratio × the skeletal muscle index (based on CT image), which was classified as L3-CXI or pectoralis muscles-CXI depending upon the type of muscle involved. The patients were divided into high- and low-CXI groups using sex-specific medians as cutoff values for CXI.
Tumor regression grade = 0,1 (sensitive to treatment) to neoadjuvant therapy was obtained in 61.6% and 46.4% of patients in the high-pretreatment L3-CXI and low-pretreatment L3-CXI groups, respectively (P = 0.023). ESCC patients with △L3-CXI <0 (L3-CXI decreased during treatment) had significantly shorter overall survival (P = 0.006) and disease-free survival (P = 0.002) than those with △L3-CXI ≥0. Multivariable analysis showed that △L3-CXI <0 was an independent negative prognostic factor for overall survival and disease-free survival.
In patients with ESCC, pretreatment CXI is a biomarker for treatment response, and △CXI can predict postoperative complications and survival outcomes. Patients could be clearly stratified by pretreatment CXI and △CXI categories, which provides a new nutritional assessment tool for clinical decision-making for patients with ESCC.