-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Tovar, Jesús Peinado, Santiago Palomino, Fernando Llanos, Claudio Ramírez, Gisella Valderrama, Roger I Calderón, Roger B Williams, Gustavo E Velásquez, Carole D Mitnick, Molly F Franke, Leonid Lecca, Prevalence of Severe Acute Respiratory Syndrome Coronavirus 2 Antibodies Among Market and City Bus Depot Workers in Lima, Peru, Clinical Infectious Diseases, Volume 74, Issue 2, 15 January 2022, Pages 343–346, https://doi.org/10.1093/cid/ciab323
Close - Share Icon Share
Abstract
We report severe acute respiratory syndrome coronavirus 2 antibody positivity among market and city bus depot workers in Lima, Peru. Among 1285 vendors from 8 markets, prevalence ranged from 27% to 73%. Among 488 workers from 3 city bus depots, prevalence ranged from 11% to 47%. Self-reported symptoms were infrequent.
Essential service workers perform functions that are critical to maintaining infrastructure. They include first responders and individuals working in healthcare, education, food and agriculture, and public transit. In the context of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, particular attention has been paid to healthcare workers who, by nature of their jobs, face an increased risk of exposure to the virus. While studies have documented frequent SARS-CoV-2 antibody positivity among healthcare workers globally [1–4], this risk can be reduced with appropriate personal protective equipment (PPE) and infection control practices [5].
Few studies have examined SARS-CoV-2 antibody prevalence among frontline essential service workers who are not healthcare workers or first responders. These workers may face an elevated risk of SARS-CoV-2 exposure through public-facing jobs that cannot be performed from home. These workers jobs may not be prioritized for, or have access to, PPE to the same extent as healthcare workers or first responders. Moreover, lower-wage frontline workers may face financial constraints in purchasing PPE and tend to rely on public transportation for commuting, further increasing risk. One US-based study found that frontline workers (most of whom were not healthcare workers) had 6 times the risk of SARS-CoV-2 antibody positivity of those who did not conduct frontline work [6]. Despite an elevated risk of occupational exposure, low-wage workers with essential frontline jobs may be unable to afford to stay home when ill, in the absence of paid sick leave.
As part of the regional response to SARS-CoV-2, the Peru Ministry of Health and the nongovernmental organization Socios En Salud conducted SARS-CoV-2 antibody testing among groups at high risk of workplace exposure. We report the frequency of antibody positivity among market and city bus depot workers, 2 sectors of understudied frontline essential service workers with potential for high exposure.
METHODS
Study Setting
Peru, a nation of 31 million inhabitants, is highly affected by SARS-CoV-2. As of 31 January 2021, >1.1 million cases and >40 000 deaths were reported, with metropolitan Lima disproportionately affected [7]. Nationwide, the case-fatality rate is 3.5% [7]. Through November 2020, SARS-CoV-2 rapid antibody testing was the predominant testing modality; rapid antigen and reverse-transcription polymerase chain reaction (RT-PCR) testing was rarely available. The present work took place in the northern Lima health jurisdiction, which includes urban and periurban areas and informal human settlements; it is characterized by high rates of poverty.
Study Procedures
Day-long SARS-CoV-2 testing campaigns were conducted at 8 markets and 3 bus depots from 5 June to 18 July 2020, during which time the reported number of cases in Peru rose from 191 758 to 349 500 [7]. Bus depots served metropolitan Lima and were operated by the primary bus company in the catchment area; markets constituted the zone’s main markets. During the study period, businesses and markets routinely implemented infection control protocols, including hand sanitizing, temperature checks, social distancing, and mandatory masks.
Before campaign implementation at each locale, Socios En Salud staff coordinated with site leadership, who provided a roster of workers and served as communication liaisons. On the day of testing, health personnel invited workers to participate in voluntary testing. Among those who agreed, the team conducted rapid SARS-CoV-2 antibody testing using the Standard Q COVID-19 IgG/IgM Duo (SD Biosensor). Workers completed a survey regarding symptoms within the past 2 weeks and relevant comorbid conditions [8]. Testing occurred in a well-ventilated area with tables and chairs spaced ≥2 m apart. After a finger prick, a drop of blood was deposited on the test device. Results were read after 15 minutes and communicated to the individual. If the result was indeterminate, a second and final test was conducted. Those with a reactive result (immunoglobulin [Ig] G, IgM, or both) were managed according to national guidelines, which included isolation, virtual clinical follow-up, tracing of contacts, and provision of social support as needed.
Statistical Analyses
We report the prevalence of antibody positivity (combined IgG/IgM) by site. Among bus depot workers, we stratify by role.
Research Ethics
Data were collected as part of public health response activities. Workers did not provide informed consent to participate in research. The Ethics Committee of the nongovernmental organization Asociación Benéfica PRISMA approved use of the data for research purposes.
RESULTS
Of listed market and bus depot workers, 94% and 90%, respectively, were tested for SARS-CoV-2 antibodies. Among them were 1285 vendors (55% female; median age [interquartile range], 40 [30–51] years) from 8 markets and 488 workers (15% female; median age, 39 [32–48] years) from 3 bus depots, including drivers (n = 329), administrative (n = 62), maintenance (n = 34) and security personnel (n = 25), cooks (n = 11), and cleaners (n = 16).
The frequency of antibody positivity ranged from 27% to 73% in market workers (Figure 1A) and was 11%, 32%, and 47% at the 3 bus depots. Prevalence tended to be lower in drivers relative to other jobs (Figure 1B). Overall, 44% of market workers and 29% of bus depot workers had a reactive result. Of those, 13% of market workers (76 of 563) and 21% of bus depot workers (29 of 141) reported coronavirus disease 2019 (COVID-19) symptoms within 2 weeks, including cough, sore throat, nasal congestion, difficulty breathing, fever, diarrhea/vomiting, headache, diarrhea, and malaise.
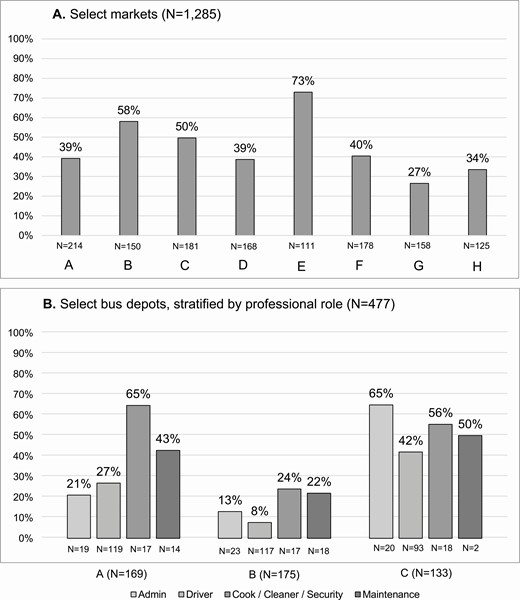
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody prevalence among essential frontline workers in northern Lima, Peru, June–July 2020. A, Vendors in select markets (n = 1285). B, Bus depot workers, excluding 11 whose professional role was not classifiable into one of the identified categories (n = 477).
The prevalence of self-reported comorbid conditions was 5.9% (76 of 1285) in market workers, with obesity (n = 33), diabetes (n = 14), and cardiovascular disease (n = 17) most common. Among bus depot workers, the prevalence of self-reported comorbidities was 7.2% (35 of 488), with obesity (n = 13), diabetes (n = 10), and cardiovascular disease (n = 5) most common.
DISCUSSION
We found frequent SARS-CoV-2 seropositivity among market and bus depot workers in urban Peru during the “first wave” of infections, highlighting the need for an urgent occupational and public health response to provide protections for these and other frontline essential workers who may be highly exposed. The risk of SARS-CoV-2 infection to frontline essential workers with direct contact with the public can be reduced with appropriate PPE and infection control, but in Peru, where the majority of employment is informal, this responsibility often falls to the individual worker. The workers included in this report were independent contractors, earning daily wages, without guaranteed salary or paid sick time. Thus, purchase of appropriate PPE and the decision to stay home when sick directly compete with earnings.
Given the frequency of asymptomatic and presymptomatic SARS-CoV-2 infection, strengthening infection control measures (eg, enabling hand-sanitization and social distancing, improving ventilation and airflow, reinforcing adherence to mask requirements for the public), and providing appropriate PPE for frontline public-facing workers are critical measures for protecting workers and curtailing transmission of SARS-CoV-2. Elevating the priority level of these frontline workers for COVID-19 vaccination would align with the National Vaccination Plan [9], which seeks to ensure the continuity of basic services, and could have important public health implications given the constrained ability of these workers to exercise other measures that would protect their contacts. Studies have shown high secondary infection rates in household contacts of frontline essential workers [10]. In Peru, independent day labor is a marker of socioeconomic precariousness; the introduction of SARS-CoV-2 to a vulnerable household may fuel a vicious cycle of household and community transmission in which overcrowding, poor ventilation, and/or inability to effectively isolate result in ongoing transmission to other household members who, likewise, must leave the home for income generation.
Early on in the pandemic, antibody testing was used for clinical management and contact tracing because tests that directly detect the virus (ie, rapid antigen and RT-PCR) were not in sufficient supply to meet testing demands in this setting. This approach is not recommended, because it fails to detect infectious cases and causes socioeconomic harm through unnecessary isolation of individuals who are no longer infectious. On the other hand, these data demonstrate that rapid antibody testing can be useful for identifying populations at high risk of infection and in whom more intensive rapid antigen or RT-PCR testing and additional protections are warranted.
The high participation rate was likely driven by a high demand for testing among workers, which was intensified by a lack of broadscale access. While high testing coverage minimizes potential selection bias; the antibody prevalences reported here may still be underestimates. First, although assay specificity is high, nearing 99%, sensitivity is about 90% after 2 weeks [11]. Second, sampling from the workplace can introduce healthy worker bias—if sick workers commonly stayed home or had died of COVID-19, the observed antibody prevalence estimates would underestimate the proportion of workers with past (or current) SARS-CoV-2 infection. Similarly, if workers commonly had early-stage infection, the positive antibody prevalence would underestimate this quantity. While the SARS-CoV-2 antibody prevalences are specific to each locale and somewhat variable, the overall message that these public-facing frontline essential service workers outside the healthcare industry are at high risk of SARS-CoV-2 infection is broadly generalizable to settings with a high incidence of SARS-CoV-2 and where there is a lack of formalized protections for independent or informal workers.
In conclusion, we found a high prevalence of SARS-CoV-2 infection in independent frontline essential workers who lack social and material protections. Policies that implement and reinforce social safety nets and prioritize vaccination for these workers may prove to be critical for control of SARS-CoV-2, particularly during the current devastating “second wave” of infections in Peru.
Notes
Acknowledgments. We are grateful to the COVID-19 Rapid Response Teams of DIRIS Lima Norte and Socios En Salud and to the frontline essential workers in Peru.
Disclaimer. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the US National Institutes of Health. The funding source had no role in the study design; in the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
Financial support. Public health response activities were financed by Peruvian Ministry of Health, Partners In Health and the United States Agency for International Development. G.E.V. received support from the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (grant K08 AI141740), the Dr Lynne Reid/Drs Eleanor and Miles Shore Fellowship at Harvard Medical School, the Burke Global Health Fellowship at the Harvard Global Health Institute, and the Harvard Center for AIDS Research (grant P30 AI060354), all to G.E.V.’s institution.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Author notes
M. F. F. and L. L. contributed equally to this work.




