-
PDF
- Split View
-
Views
-
Cite
Cite
Tuo Ji, Hai-Lian Chen, Jing Xu, Ling-Ning Wu, Jie-Jia Li, Kai Chen, Gang Qin, Lockdown Contained the Spread of 2019 Novel Coronavirus Disease in Huangshi City, China: Early Epidemiological Findings, Clinical Infectious Diseases, Volume 71, Issue 6, 15 September 2020, Pages 1454–1460, https://doi.org/10.1093/cid/ciaa390
Close - Share Icon Share
Abstract
To control the spread of 2019 novel coronavirus disease (COVID-19), China sealed Wuhan on 23 January 2020 and soon expanded lockdown to 12 other cities in Hubei province. We aimed to describe the epidemiological characteristics in one of the cities and highlight the effect of current implemented lockdown and nonpharmaceutical interventions.
We retrieved data of reported cases in Huangshi and Wuhan from publicly available disease databases. Local epidemiological data on suspected or confirmed cases in Huangshi were collected through field investigation. Epidemic curves were constructed with data on reported and observed cases.
The accumulated confirmed COVID-19 cases and fatality in Huangshi were reported to be 1015 and 3.74%, respectively, compared with 50006 and 5.08% in Wuhan until 27 March 2020. Right after 24 January, the epidemic curve based on observed cases in Huangshi became flattened. And 1 February 2020 was identified as the “turning point” as the epidemic in Huangshi faded soon afterward. COVID-19 epidemic was characterized by mild cases in Huangshi, accounting for 82.66% of total cases. Moreover, 50 asymptomatic infections were identified in adults and children. In addition, we found confirmed cases in 19 familial clusters and 21 healthcare workers, supporting interhuman transmission.
Our study reported the temporal dynamics and characteristics of the COVID-19 epidemic in Huangshi city, China, across the unprecedented intervention. Such new epidemiological inference might provide further guidance on current lockdown measures in high-risk cities and, subsequently, help improve public health intervention strategies against the pandemic on the country and global levels.
In December 2019, several cases of pneumonia of unknown etiology occurred in Wuhan city, Hubei province, China [1]. On 7 January 2020, a novel coronavirus was identified by the Chinese Center for Disease Control and Prevention (CDC) from the throat swab sample of a patient. It was named 2019 novel coronavirus (2019-nCoV) by the World Health Organization (WHO) [2] and subsequently severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses [3]. Preliminary studies have suggested that SARS-CoV-2 is more infectious but less deadly than the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) [4–8]. The 2019 novel coronavirus disease (COVID-19) has rapidly spread from Wuhan to other areas in China and an additional 190 countries in the world [9]. Many countries are facing the challenges in controlling its spread.
Wuhan is the capital of Hubei province with >11 million residents and is connected to other cities via high-speed railways and frequent domestic and international airline flights. In the early days of this outbreak, a total of 389 confirmed cases reported in Wuhan on 22 January 2020, there was much uncertainty about the epidemic scale. However, it was estimated that there would be over 3 billion passenger journeys within as well as in and out of China between 10 January and 18 February, around the Spring Festival (CGTN, 2020) [10]. As of 23 January 2020, Chinese government initiated an unprecedented public health intervention to confine the epidemic by shutting down all transportation in and out of Wuhan (ie, a modern form of quarantine) [11]. It was estimated that the number of newly confirmed cases would reach its peak at 8 (6–10) days after the lockdown initiation and that the quarantining might last for 2 weeks [12]. However, the real-world evidence for the impact of such interventions has not been thoroughly examined. The outbound travel restriction still remains effective in Wuhan when this article was written (28 March 2020).
Huangshi city, with a population of 2.7 million, is located in the southeast of Hubei Province, bordering Wuhan. Given their geographical and economical connection, Wuhan and Huangshi are officially recognized as “sister cities.” Lockdown of Huangshi meant to curb the import of COVID-19 cases from Wuhan, as well as the export of cases to other cities. The lockdown intervention, same as that in Wuhan, has lasted for 2 months (between 24 January and 23 March 2020) in Huangshi. At present, little is known regarding the COVID-19 epidemic in other cities near Wuhan. We conducted this study to describe epidemiological features of the novel coronavirus spread in Huangshi and to highlight the effect of the lockdown intervention.
METHODS
Data Source
We retrieved and merged data of reported cases in Huangshi and Wuhan from publicly available disease databases of Hubei Provincial Health Committee (http://wjw.hubei.gov.cn/). Local epidemiological data on suspected and confirmed cases in Huangshi were collected through field investigation by epidemiologists from local CDC together with trained health care workers from the hospitals. Standardized forms were designed to interview with the patients, their relatives, and close contacts. Data used in the present analyses include age, sex, geographic location, dates of symptom onset, contact history with suspicious persons or environment, and clinical syndromes.
Data collection and analysis of these cases were determined by the municipal Health Commission to be part of an outbreak investigation. The study was thus deemed exempt from institutional review board approval.
Infection Control Measures
As of 10:00 AM Beijing time, 23 January 2020, Wuhan shut down all public transportation, including the airport, railway station, and bus and subway services. Closure of travel to and from the Huangshi was implemented starting 10:00 AM, 24 January 2020. In addition, Huangshi on 25 January 2020 addressed a wide range of nonpharmaceutical interventions (NPI) regarding surveillance, detection, and containment measures (http://www.hbdaye.gov.cn/xwzx/dyyw/202001/t20200128_597815.html). First, real-time syndromic surveillance was used for individuals seeking care at clinics or hospitals to detect the onset of the illness. Second, health screening and quarantine were applied for incoming travelers. Third, voluntary personal social isolation (such as staying at home) and compulsory facial masks outdoors were indicated for all residents, followed by monitoring and reporting. Finally, factories, businesses, schools, and other institutions were closed during the outbreak. The community workers, together with volunteers, dedicated to ensure the effective NPI implementation. As the epidemic situation got stable, Huangshi on 13 March 2020 announced resuming work and production in an orderly manner.
Case Definitions
These diagnostic criteria were based on the WHO interim guidance [2] and the recommendation by the Chinese National Health Commission (http://www.gov.cn/zhuanti/2020-02/05/content_5474791.htm).
A confirmed case was defined as both (1) fulfilled 2 clinical criteria plus 1 epidemiological clue, or all 3 clinical criteria, and (2) had the throat-swab specimens tested positive for SARS-CoV-2 using real-time reverse transcription polymerase chain reaction (RT-PCR) assay. Clinical criteria of manifestations were: (1) fever and/or acute respiratory illness, (2) radiographic evidence of pneumonia, and (3) low or normal white-cell count or low lymphocyte count. Epidemiological clues were: (1) history of travel to or residence in Wuhan city within 14 days prior to symptom onset; (2) close contact with a confirmed or probable case of COVID-19 within 14 days prior to symptom onset; (3) close contact with persons who had fever or acute respiratory illness and were from Wuhan city or local community with case-reported, within 14 days prior to symptom onset; (4) a cluster of persons with similar symptoms was identified. The laboratory protocol for SARS-CoV-2 real-time RT-PCR assay was described previously [4]. The tests were screened by local CDC and confirmed by Hubei provincial CDC.
Confirmed cases were classified into 4 clinical syndromes: (1) uncomplicated illness, for example, cold-like upper respiratory illness; (2) mild pneumonia, that is, mild radiographic evidence of pneumonia; (3) severe pneumonia, plus 1 of severe respiratory distress, respiratory rate >30 breaths/minute, or SpO2 <90% on room air; (4) critical illness, complicated with septic shock or acute respiratory distress syndrome (ARDS) needing mechanical ventilation.
From 12 February 2020, the clinically diagnosed patients in Hubei province (not applicable for other provinces in China) who fulfilled 1 epidemiological clue and had radiographic evidence of pneumonia were classified as confirmed cases, regardless of the PCR results.
Statistical Analysis
All continuous variables were analyzed with student t tests and categorical variables with χ2 or Fisher exact tests. A P-value of <.05 was considered as the level of significance. The epidemic curves were constructed on reported or observed cases. Stata software (version 14.0, StataCorp, USA) was used for statistical analysis. The maps were performed using ArcGIS software (version 10.6, Esri, USA).
RESULTS
The accumulated number of confirmed cases with COVID-19 in Huangshi and Wuhan were reported to be 1015 and 50006, respectively, until 27 March 2020 (Figure 1A). In Huangshi, 57% (575/1015) of the total cases were in the main city, following by its 2 satellite cities Daye (24%) and Yangxin (16%). Patients in Huangshi showed slightly lower case fatality of 3.74% (38/1015), compared with 5.08% (2538/50006) in Wuhan (P = .055).
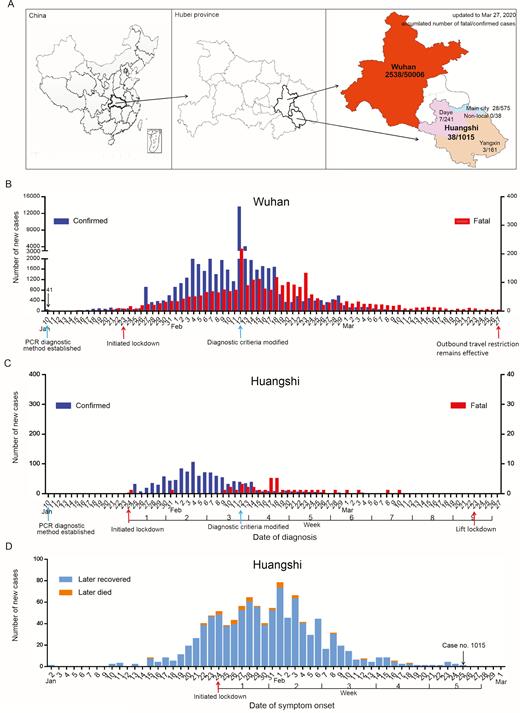
Epidemic curves of reported and observed cases with COVID-19 in Wuhan and Huangshi. A, Accumulated number of confirmed and fatal cases with COVID-19 in Wuhan and Huangshi until 27 March 2020. B, New confirmed and fatal cases in Wuhan between 10 January and 27 March 2020. C, New confirmed and fatal cases with COVID-19 in Huangshi between 10 January and 27 March 2020. D, New observed cases with COVID-19 in Huangshi between 2 January and 1 March 2020. Abbreviation: COVID-19, 2019 novel coronavirus disease, PCR, polymerase chain reaction.
Based on the reported data by the official government, we constructed the epidemic curves of confirmed and fatal cases with COVID-19 in Wuhan and Huangshi from 10 January to 27 March 2020 (Figure 1B, C). The exponential increase in the number of reported cases was observed in Wuhan. The abrupt increase on 12 February was attributed to the diagnosis criteria modification (Figure 1B). In contrast, the threat of a sustained epidemic in Huangshi is less likely (Figure 1C).
Given that there was delay for the laboratory test and diagnosis procedure, we also constructed the epidemic curve for Huangshi based on symptoms onset. The first case of COVID-19 in Huangshi was observed on 2 January. The onset day of epidemic was 10 January, defined as the first day of ascending phase leading to the peak. Right after 24 January (day 1 of lockdown), the epidemic curve became flattened, suggesting that the lockdown intervention slowed the progression of the epidemic. The first of February 2020 (day 9 of lockdown) was identified as the “turning point” as the epidemic in Huangshi faded soon afterward. There have been no new cases observed since 26 February 2020 (Figure 1D).
Demographic and clinical characteristics of the 1015 confirmed COVID-19 cases, 93.62% (997) of whom were SARS-CoV-2 RNA positive, are shown in Table 1. They were consisted of 509 males and 504 females, aged from 1 month through 92 years (mean 49.01, median 49). The novel coronavirus infection predominated in the young and mature adult age groups (18–44 group, 37.04%; 45–64 group, 42.07%). There were 8 cases in infants (0–3 years) and 6 cases in pregnant women. The proportion of healthcare worker (HCW) cases was 2.07% (21/1015). Those patients who had a history of visit to or residence in Wuhan city within 14 days prior to symptom onset were defined as probably imported cases. The percentages of imported cases in patients with symptom onset before 24 January 2020 and patients onset afterward were 63.07% and 31.94%, respectively (P < .001). COVID-19 epidemic was characterized by mild cases (uncomplicated illness or mild pneumonia) in Huangshi, accounting for 82.66% of total cases. The percentage of uncomplicated illness in cases with symptoms onset on/after 24 January 2020 were significantly higher than that in cases with earlier onset (46.48% vs 23.30%, P < .001). There was no significant difference between cases with onset before 24 January 2020 and those afterward in terms of age, sex, and fatality rate.
Demographic and Clinical Characteristics of Confirmed COVID-19 Cases in Huangshi
| . | Symptom Onset . | . | |
|---|---|---|---|
| Characteristics . | Before 24 Jan (n = 176) . | On/after 24 Jan (n = 839) . | Total (n = 1015) . |
| Age (years)a | 48 (21–85) | 50 (0–92) | 49 (0–92) |
| ≤17 | 0 | 19 (2.26%) | 19 (1.87%) |
| 18–44 | 75 (42.61%) | 301 (35.88%) | 376 (37.04%) |
| 45–64 | 79 (44.89%) | 348 (41.48%) | 427 (42.07%) |
| ≥65 | 22 (12.50%) | 171 (20.38%) | 193 (19.01%) |
| Male | 87 (49.43%) | 422 (50.30%) | 509 (50.15%) |
| Imported caseb | 111 (63.07%) | 268 (31.94%) | 379 (37.34%) |
| Pregnant women | 0 | 6 (0.68%) | 6 (0.59%) |
| Clinical syndrome | |||
| Uncomplicated illnessc | 41 (23.30%) | 390 (46.48%) | 431 (42.46%) |
| Mild pneumonia | 104 (59.09%) | 304 (36.23%) | 408 (40.20%) |
| Severe pneumonia | 23 (13.07%) | 84 (10.01%) | 107 (10.54%) |
| Critical illness | 8 (4.55%) | 61 (7.27%) | 69 (6.80%) |
| Fatality | 4 (2.27%) | 34 (4.05%) | 38 (3.74%) |
| Healthcare worker | 4 (2.27%) | 17 (2.03%) | 21 (2.07%) |
| . | Symptom Onset . | . | |
|---|---|---|---|
| Characteristics . | Before 24 Jan (n = 176) . | On/after 24 Jan (n = 839) . | Total (n = 1015) . |
| Age (years)a | 48 (21–85) | 50 (0–92) | 49 (0–92) |
| ≤17 | 0 | 19 (2.26%) | 19 (1.87%) |
| 18–44 | 75 (42.61%) | 301 (35.88%) | 376 (37.04%) |
| 45–64 | 79 (44.89%) | 348 (41.48%) | 427 (42.07%) |
| ≥65 | 22 (12.50%) | 171 (20.38%) | 193 (19.01%) |
| Male | 87 (49.43%) | 422 (50.30%) | 509 (50.15%) |
| Imported caseb | 111 (63.07%) | 268 (31.94%) | 379 (37.34%) |
| Pregnant women | 0 | 6 (0.68%) | 6 (0.59%) |
| Clinical syndrome | |||
| Uncomplicated illnessc | 41 (23.30%) | 390 (46.48%) | 431 (42.46%) |
| Mild pneumonia | 104 (59.09%) | 304 (36.23%) | 408 (40.20%) |
| Severe pneumonia | 23 (13.07%) | 84 (10.01%) | 107 (10.54%) |
| Critical illness | 8 (4.55%) | 61 (7.27%) | 69 (6.80%) |
| Fatality | 4 (2.27%) | 34 (4.05%) | 38 (3.74%) |
| Healthcare worker | 4 (2.27%) | 17 (2.03%) | 21 (2.07%) |
Abbreviation: COVID-19, 2019 novel coronavirus disease.
aMedian (range).
bImported cases were defined as those who had a history of visit to or residence in Wuhan city within 14 days prior to symptom onset. χ2 test P < .001.
cPercentage of uncomplicated illness. χ2 test P < .001.
Demographic and Clinical Characteristics of Confirmed COVID-19 Cases in Huangshi
| . | Symptom Onset . | . | |
|---|---|---|---|
| Characteristics . | Before 24 Jan (n = 176) . | On/after 24 Jan (n = 839) . | Total (n = 1015) . |
| Age (years)a | 48 (21–85) | 50 (0–92) | 49 (0–92) |
| ≤17 | 0 | 19 (2.26%) | 19 (1.87%) |
| 18–44 | 75 (42.61%) | 301 (35.88%) | 376 (37.04%) |
| 45–64 | 79 (44.89%) | 348 (41.48%) | 427 (42.07%) |
| ≥65 | 22 (12.50%) | 171 (20.38%) | 193 (19.01%) |
| Male | 87 (49.43%) | 422 (50.30%) | 509 (50.15%) |
| Imported caseb | 111 (63.07%) | 268 (31.94%) | 379 (37.34%) |
| Pregnant women | 0 | 6 (0.68%) | 6 (0.59%) |
| Clinical syndrome | |||
| Uncomplicated illnessc | 41 (23.30%) | 390 (46.48%) | 431 (42.46%) |
| Mild pneumonia | 104 (59.09%) | 304 (36.23%) | 408 (40.20%) |
| Severe pneumonia | 23 (13.07%) | 84 (10.01%) | 107 (10.54%) |
| Critical illness | 8 (4.55%) | 61 (7.27%) | 69 (6.80%) |
| Fatality | 4 (2.27%) | 34 (4.05%) | 38 (3.74%) |
| Healthcare worker | 4 (2.27%) | 17 (2.03%) | 21 (2.07%) |
| . | Symptom Onset . | . | |
|---|---|---|---|
| Characteristics . | Before 24 Jan (n = 176) . | On/after 24 Jan (n = 839) . | Total (n = 1015) . |
| Age (years)a | 48 (21–85) | 50 (0–92) | 49 (0–92) |
| ≤17 | 0 | 19 (2.26%) | 19 (1.87%) |
| 18–44 | 75 (42.61%) | 301 (35.88%) | 376 (37.04%) |
| 45–64 | 79 (44.89%) | 348 (41.48%) | 427 (42.07%) |
| ≥65 | 22 (12.50%) | 171 (20.38%) | 193 (19.01%) |
| Male | 87 (49.43%) | 422 (50.30%) | 509 (50.15%) |
| Imported caseb | 111 (63.07%) | 268 (31.94%) | 379 (37.34%) |
| Pregnant women | 0 | 6 (0.68%) | 6 (0.59%) |
| Clinical syndrome | |||
| Uncomplicated illnessc | 41 (23.30%) | 390 (46.48%) | 431 (42.46%) |
| Mild pneumonia | 104 (59.09%) | 304 (36.23%) | 408 (40.20%) |
| Severe pneumonia | 23 (13.07%) | 84 (10.01%) | 107 (10.54%) |
| Critical illness | 8 (4.55%) | 61 (7.27%) | 69 (6.80%) |
| Fatality | 4 (2.27%) | 34 (4.05%) | 38 (3.74%) |
| Healthcare worker | 4 (2.27%) | 17 (2.03%) | 21 (2.07%) |
Abbreviation: COVID-19, 2019 novel coronavirus disease.
aMedian (range).
bImported cases were defined as those who had a history of visit to or residence in Wuhan city within 14 days prior to symptom onset. χ2 test P < .001.
cPercentage of uncomplicated illness. χ2 test P < .001.
Nineteen familial clusters of confirmed cases have been found and are shown in Figure 2. Four clusters were composed of imported cases and local cases. The other 15 clusters were all local cases, suggesting secondary or tertiary transmission. Based on the dates of illness onset of cases in these clusters, we estimated that the serial interval distribution was 6.5 ± 6.3 days (mean ± standard deviation [SD]).
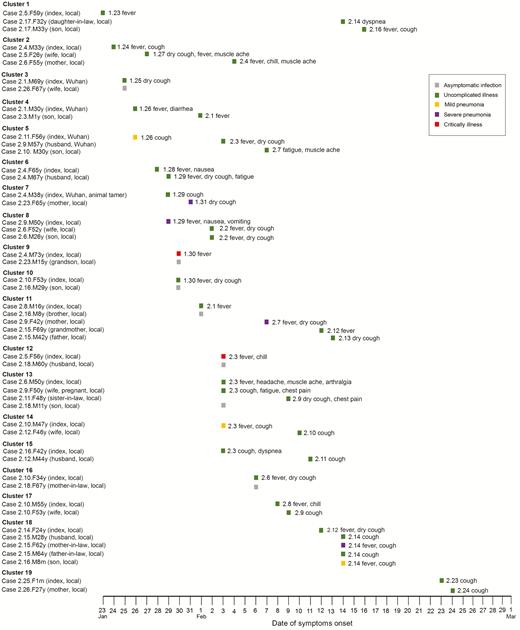
Timeline of 19 familial clusters of COVID-19 in Huangshi. Date of diagnosis (eg, 2.4, February 4, 2020), sex (M or F, male or female), age (y or m, years or months), relationship to the index case (eg, son or mother), imported case or not (Wuhan or local) were used to denote main characteristics of the patient. Abbreviation: COVID-19, 2019 novel coronavirus disease.
Moreover, asymptomatic infections have been identified not only in 41 adults but also in 9 children. They had epidemiological clues for COVID-19 contact, and the throat-swab tested positive for SARS-CoV-2 RNA. After quarantined for at least 14 days, all the persons had no signs of illness.
DISCUSSION
As observed during this pandemic, the novel coronavirus virus could spread globally before the epidemic peaks locally [9]. One week before WHO’s declaration of the global public health emergency of international concern, Chinese government launched the remarkable lockdown intervention in high-risk cities, the first such quarantine in its history. To the best of our knowledge, this report for the first time described the epidemiological features of the COVID-19 outbreak in a city in China, other than Wuhan, across the implemented lockdown intervention. The relationship detected in our analysis strongly suggests that the aggressive public health intervention resulted in flattened epidemic curves and a trend toward better overall outcomes.
Why were Huangshi and 11 other cities closed down besides Wuhan? There had been concerns that the synchrony level of COVID-19 epidemics in Hubei’s 13 cities might be high enough to view Hubei province as “single epidemiological unit” [13]. However, our study revealed considerable differences in the timing and magnitude of COVID-19 epidemics between Huangshi and Wuhan cities. The basic reproduction number (R0) of COVID-19 was estimated to be as high as 3.11–6.49 [12, 14]. It turned out that the rapidity of the growth of cases in Wuhan was much greater than that observed in outbreaks of either SARS or MERS-CoV [15, 16]. The lockdown intervention resulted in the limited outbreak in Huangshi, as well as containment of the export of cases. Some mathematical models suggested that the lockdown strategy applied early may significantly reduce disease transmission by up to 70% [12].
Most researchers believe that Wuhan is the epicenter of COVID-19 outbreak, with patient zero suspected to have originated there. Yet how this novel coronavirus arrived in Wuhan remains unclear. The primary reservoirs for SARS-CoV and MERS-CoV were bats, whereas the intermediary sources were civet cats and camels, respectively [17]. The genomic sequencing results showed that 2019-nCoV was closely related (with 88% identity) to 2 bat-derived SARS-like coronaviruses but more distant from SARS-CoV (79%) and MERS-CoV (50%) [18]. In addition, the epidemiological association between 66% (27/41) of the initial infected patients with the Huanan wet market [4] suggests that the novel coronavirus may be related to sale of wild animal as game food. Consistent with previous reports, we found laboratory-confirmed cases in 19 familial clusters and 21 healthcare workers, supporting human-to-human transmission.
It is worth noting that COVID-19 was characterized by mild cases (uncomplicated illness plus mild pneumonia) in Huangshi, accounting for 82.66% of total confirmed cases, higher than previous reports on cases in Wuhan [6]. In addition, 50 asymptomatic infections were identified through screening. This might be explained by both a decreased virulence throughout the successive transmission, like SARS-CoV [19], and underreporting bias in early cases in Wuhan. Undetected asymptomatic or mild cases may also be a factor in the apparent decrease in the case fatality rate over time. If asymptomatic or mildly symptomatic but infectious cases constituted an important fraction of the total infection, R0 might be higher than estimated because detecting and isolating these cases would be “extremely challenging” [20, 21].
A practical issue requiring further study is when such lockdown intervention could be relaxed. Without an effective vaccine, these cities remain vulnerable against imported cases with infection. In the event of a severe pandemic, such as 1918 influenza, cities will likely need to maintain lockdown for longer than 2–8 weeks [22]. Actually, Huangshi city reported no new cases since it lift lockdown on 23 March 2020.
Admittedly, this study has several limitations. First, only 1 city with COVID-19 was included. It would be better to include as many cities as possible in Hubei, and in other provinces in China, to get a more comprehensive insight of COVID-19 epidemic. Second, more detailed information, such as genomic sequencing outcomes and the overall people’s response to NPI measures, was unavailable at the time of analysis. However, the data in this study permit an early assessment of the epidemiological characteristics of COVID-19 in Huangshi, China. Finally, underreporting bias is also a natural limitation of this study, as some asymptomatic or mild cases might be missed.
In conclusion, our study reported the temporal dynamics and characteristics of the COVID-19 epidemic in Huangshi city, China, across the implemented lockdown intervention. Such new findings might provide further guidance on current lockdown intervention in high-risk cities and, subsequently, improve public health strategies against the pandemic on the country and global levels.
Notes
Acknowledgments. The authors thank all the patients and their families, as well as the epidemiologists and medical staff who carried out this study in Huangshi city.
Financial support. This study was funded in part by grants from Jiangsu Provincial Health Committee (QNRC2016402 and LGY2017039) and from Nantong Municipal Bureau of Science and Technology (HS2016002).
Potential conflicts of interest. T. J., H.-L. C., J. X., L.-N. W., J.-J. L., and K. C. declared that there were no conflicts of interests. G. Q. is the recipient of grants from Jiangsu Provincial Health Committee and Nantong Municipal Bureau of Science and Technology. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Author notes
T. J. and H-L. C. contributed equally to this work.




