-
PDF
- Split View
-
Views
-
Cite
Cite
Zaal Meher-Homji, Daniel North, James D Stewart, Diana Moir, Anna Kalff, Shaun Fleming, Michelle R Ananda-Rajah, Andrew Fuller, C Orla Morrissey, A 40-Year-Old Man With Persistent Febrile Neutropenia and Subsequent Rash, Clinical Infectious Diseases, Volume 71, Issue 12, 15 December 2020, Pages 3260–3262, https://doi.org/10.1093/cid/ciaa562
Close - Share Icon Share
A 40-year-old previously well male was admitted for treatment of hairy cell leukemia, with a 5-day course of cladribine. Dietary history revealed the frequent consumption of uncooked pizza dough and the use of a probiotic. He developed fevers and hepatic derangement shortly afterward, resulting in a diagnosis of secondary hemophagocytic lymphohistiocytosis, requiring treatment with etoposide, dexamethasone, and tocilizumab, and resulting in a prolonged period of neutropenia. The patient developed persistent neutropenic fevers despite broad-spectrum antimicrobial agents and liposomal amphotericin B prophylaxis. On day 20 of neutropenia, an aerobic blood culture bottle flagged positive after 3 days of incubation. Gram stain demonstrated budding yeast cells, and subculture demonstrated growth of 0.5- to 1-mm cream-colored glabrous colonies on Sabouraud dextrose agar after 24 hours of incubation at 35°C (Figure 1). Blood cultures remained positive for 7 consecutive days with the same organism, but resolved after the removal of the intravenous catheter. The patient was neutropenic (< 0.5 × 109/L) for a total of 30 days, and after neutrophil count recovery, a satellite papular and nodular rash over both forearms was noted (Figure 2). On skin biopsy, Grocott methenamine silver staining revealed numerous budding yeast cells in the subcutaneous tissue with associated necrotic debris mixed with neutrophils (Figure 3). The skin biopsy tissue cultured the same organism as was isolated from the blood cultures.

Sabouraud dextrose agar subculture from a positive aerobic blood culture demonstrating numerous 0.5- to 1-mm cream-colored glabrous colonies after 24 hours of incubation at 35°C.

Erythematous papules and nodules on the left forearm of a 40-year-old man after 30 days of neutropenia.
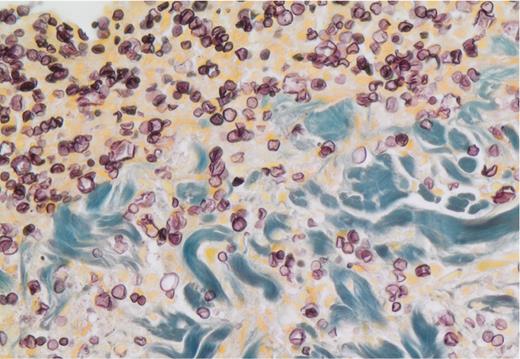
Grocott methenamine silver stain from a single nodule (×40 magnification). Budding yeast cells are visible in the subcutaneous tissue with associated necrotic debris mixed with neutrophils.
What is the diagnosis?
Diagnosis: Saccharomyces cerevisiae (baker’s yeast) fungemia and associated satellite skin lesions.
Saccharomyces cerevisiae is an ascomycetous yeast used in alcohol fermentation and in baking as a leavening agent, whereas the phenotypically indistinguishable S. cerevisiae var boulardii is a commercially available probiotic product. Saccharomyces cerevisiae is a likely transient dietary commensal in the gastrointestinal tract, which can be found in relative abundance in the feces of normal hosts eating a Western diet [1, 2]. Saccharomyces cerevisiae has been implicated in invasive disease among immunocompromised hosts, patients with intravenous catheter use, and patients with digestive tract disease [3]. While the majority of invasive disease is characterized by fungemia, organ involvement including pulmonary, intra-abdominal, urinary tract disease, and endocarditis has been described [3].
The patient had multiple risk factors for invasive fungal disease, including prolonged neutropenia and intravenous catheter placement. The main differential diagnosis we considered was invasive candidiasis; however, the frequent consumption of uncooked pizza dough increased the likelihood of S. cerevisiae invasive disease. Unusually, on myeloid reconstitution, he developed satellite skin lesions (Figure 2), characteristic of invasive candidiasis [4]. The skin biopsy revealed numerous yeast cells in the subcutaneous tissue (Figure 3), and S. cerevisiae was also cultured from the skin biopsy despite 10 days of appropriate antifungal therapy. Culturing the organism from the skin biopsy was important, as the histological features of S. cerevisiae are relatively indistinguishable from other budding yeasts.
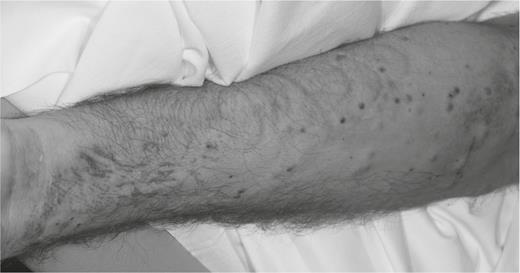
Erythematous papules and nodules on the left forearm of a 40-year-old man after 30 days of neutropenia.
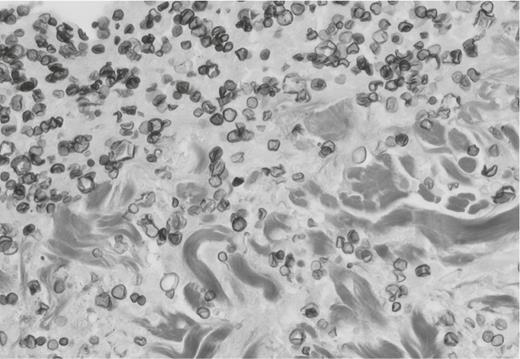
Grocott methenamine silver stain from a single nodule (×40 magnification). Budding yeast cells are visible in the subcutaneous tissue with associated necrotic debris mixed with neutrophils.
The patient completed a 3-week course of anidulafungin followed by an additional 3 weeks of voriconazole with resolution of the rash and clinical recovery. Serial transthoracic echocardiography revealed no cardiac valvular disease. Although the majority of historical cases have been treated with amphotericin B [3], the minimum inhibitory concentrations for echinocandins and azole derivatives other than fluconazole are generally low, and have been used even in the absence of clinically identified breakpoints for this organism. Immunocompromised patients should be educated to refrain from consuming probiotic products and uncooked foods that contain living yeast.
Note
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References




