-
PDF
- Split View
-
Views
-
Cite
Cite
Sarah E Smith, Robert Pratt, Lisa Trieu, Pennan M Barry, Dzung T Thai, Shama Desai Ahuja, Sarita Shah, Epidemiology of Pediatric Multidrug-Resistant Tuberculosis in the United States, 1993–2014, Clinical Infectious Diseases, Volume 65, Issue 9, 1 November 2017, Pages 1437–1443, https://doi.org/10.1093/cid/cix561
Close - Share Icon Share
Abstract
Multidrug-resistant tuberculosis (MDR-TB) is an important global public health threat, but accurate estimates of MDR-TB burden among children are lacking.
We analyzed demographic, clinical, and laboratory data for newly diagnosed pediatric (age <15 years) TB cases reported to the US National TB Surveillance System during 1993–2014. MDR-TB was defined as culture-confirmed TB disease with resistance to at least isoniazid and rifampicin. To ascertain potential underestimation of pediatric MDR-TB, we surveyed high-burden states for clinically diagnosed cases treated for MDR-TB.
Of 20789 pediatric TB cases, 5162 (24.8%) had bacteriologically confirmed TB. Among 4826 (93.5%) with drug susceptibility testing, 82 (1.7%) had MDR-TB. Most pediatric MDR-TB cases were female (n = 51 [62%]), median age was 5 years (interquartile range, 1–12 years), one-third were Hispanic (n = 28 [34%]), and two-thirds (n = 55 [67%]) were born in the United States. Most cases had additional resistance to ≥1 other first-line drug (n = 66 [81%]) and one-third had resistance to ≥1 second-line drug (24/73 tested). Of 77 who started treatment prior to 2013, 66 (86%) completed treatment and 4 (5%) died. Among the 4 high-TB-burden states/jurisdictions surveyed, there was 42%–55% underestimation of pediatric MDR-TB cases when using only culture-confirmed case definitions.
Only one-quarter of pediatric TB cases had culture-confirmed TB, likely resulting in underestimation of true pediatric MDR-TB burden in the United States using strictly bacteriologic criteria. Better estimates of pediatric MDR-TB burden in the United States are needed and should include clinical diagnoses based on epidemiologic criteria.
Multidrug-resistant tuberculosis (MDR-TB), defined as resistance to at least isoniazid and rifampicin, is an important clinical and public health threat worldwide with an estimated 480000 cases in 2015 [1]. Accurate estimates of MDR-TB burden among children are not available, in part due to the paucibacillary nature of TB in children and challenges with microbiologic confirmation of disease [2]. Globally, only 10%–30% of pediatric TB cases have laboratory-confirmed TB disease; most cases are diagnosed clinically based on symptoms and chest radiograph findings [3, 4]. Confirming MDR-TB requires microbiologic diagnosis, which makes detecting all cases of MDR-TB among children impossible with currently available diagnostics. Pediatric TB cases may be recommended for empiric MDR-TB treatment based on clinical or epidemiologic evidence of MDR-TB, such as known contact to a pulmonary MDR-TB case, first-line TB treatment failure, or loss to follow-up during previous TB treatment. Currently, in the United States, only laboratory-confirmed cases of MDR-TB are counted as MDR-TB in the national TB surveillance system.
Recent modeling studies estimate that 850000–1000000 children developed TB in 2010, of whom 25000–32000 had MDR-TB [5, 6]. The World Health Organization (WHO) estimated 490000 incident cases of TB among children in 2012, the first global TB estimate among children and about half of the modeling estimates [7]. This WHO estimate assumed that the ratio of notified to incident cases was the same for adults and children, essentially ignoring the difficulties of pediatric TB diagnosis. More recent estimates of pediatric TB by WHO have incorporated new modeling approaches that better estimate TB burden among children [1]. However, a major gap in diagnosis and treatment of pediatric TB and MDR-TB still exists. Identifying pediatric MDR-TB is important not only for initiating appropriate treatment in children, but also to identify where recent transmission may have occurred. Knowledge of the clinical management and outcomes of children with MDR-TB is limited worldwide, consisting mainly of case reports and small case series [8–14]. However, appropriate treatment of pediatric MDR-TB has favorable outcomes, even in resource-limited settings of high human immunodeficiency virus (HIV) prevalence [8, 15]. As funding for TB control activities decreases, better estimates of MDR-TB burden are needed to develop accurate spending estimates and to support development of pediatric formulations of second-line anti-TB drugs.
The United States has had declining TB incidence for 22 years, with 2015 representing the first year since 1993 that TB case counts increased, yet annual proportions of MDR-TB have remained essentially stable [16]. Children account for approximately 5% of the TB burden in the United States, with 440 cases of childhood TB reported in 2015 [16]. However, the epidemiology of MDR-TB among children in the United States has not previously been reported. In this study, we describe the epidemiology of pediatric MDR-TB in the United States over the past 2 decades.
METHODS
All 50 states and the District of Columbia report TB cases to the US National Tuberculosis Surveillance System (NTSS), using a standardized case report form on which demographic, clinical, laboratory, initial treatment regimen, and treatment outcome information are collected. Inclusion in the NTSS requires that the case meet 1 of the following verification criteria: (1) laboratory-confirmed cases have Mycobacterium tuberculosis isolated from a clinical specimen by culture or nucleic acid amplification test or, in the absence of these, demonstration of acid-fast bacilli in the specimen; (2) clinical cases meet the following criteria: (a) positive TB skin test or interferon-γ release assay, (b) other signs or symptoms compatible with TB (eg, abnormal chest radiograph, or clinical evidence of current disease), (c) treatment with ≥2 anti-TB medications, and (d) completed diagnostic evaluation; or (3) provider diagnosis case is diagnosed by a healthcare provider but does not fulfill all criteria necessary to meet laboratory or clinical case definitions.
In this analysis, we included all newly diagnosed pediatric TB cases (age <15 years) reported to the NTSS from 1993 through 2014 [17]. Laboratory-confirmed MDR-TB was defined as culture-confirmed TB disease caused by M. tuberculosis resistant to at least isoniazid and rifampicin during initial or final drug susceptibility testing (DST) (in contrast to standard annual reports of US national TB surveillance data that use only initial DST) [18]. US-born persons were defined as persons born in the United States, Puerto Rico, or US outlying area or born abroad to US parents; all other persons were defined as foreign-born. Children were grouped into age categories that are biologically relevant to diagnosis and disease progression [2]. HIV test results were available for each reported TB case, with the following exceptions: through 2004, California only reported positive HIV results based on TB and AIDS registry matching; all other California TB cases were classified as “unknown.” California did not report any HIV results from 2005 to 2010, and HIV data are missing from Vermont during 2007–2014.
Regional categorization of countries was based on the WHO Global Tuberculosis Report [1]. Anti-TB drug categories and resistance patterns are defined by WHO [19]. NTSS end-of-treatment outcomes have been previously defined [17]. In brief, a patient either (1) completed the prescribed course of therapy as recorded by the patient’s clinician, (2) could not be located before treatment completion, (3) refused to complete therapy, (4) permanently stopped therapy because of an adverse event due to anti-TB medications, (5) died before treatment completion, or (6) moved to a different local health department jurisdiction and the final treatment outcome was unknown. Sputum culture conversion was defined as an initial culture-positive sputum specimen, followed by at least 1 negative sputum culture without a subsequent positive culture.
To estimate potential underestimation of pediatric MDR-TB in NTSS, which is based only on phenotypic DST results, we contacted 6 states that contributed the highest number of laboratory-confirmed pediatric MDR-TB cases to NTSS during the study period. Each state was asked to report all cases of pediatric TB in patients who received MDR-TB treatment and, when available, the reason for this treatment decision. Empiric MDR-TB was defined as a patient who received MDR-TB treatment based on clinical or epidemiologic evidence of MDR-TB without laboratory confirmation of MDR-TB. State case identification and report year were used to match the cases in NTSS for complete epidemiologic data. The proportion of underestimation was calculated per reporting state as number of empiric MDR-TB cases divided by total number of cases treated for MDR-TB (laboratory-confirmed and empiric MDR-TB) during the same period.
Univariate analyses were used to assess trends and frequencies. Bivariate analyses were used to assess associations of demographic and clinical characteristics with age group and with empiric MDR-TB using Pearson’s χ2 or Fisher’s exact test, where appropriate. The Kruskal-Wallis test was used to test association of continuous variables. P value <.05 was considered statistically significant. Analyses were performed using SAS version 9.3 software (SAS Institute, Cary, North Carolina).
This study was approved by the NTSS Analytic Steering Committee and determined to be an evaluation of routine surveillance data by the Centers for Disease Control and Prevention.
RESULTS
Of 20789 children with TB disease reported during 1993–2014, 5162 (24.8%) had culture-confirmed TB, of whom 4826 (93.5%) had phenotypic DST results available to rifampicin and isoniazid (Figure 1). The annual proportion of culture-confirmed pediatric TB ranged between 23% and 34%. Eighty-two (1.7%) children had laboratory-confirmed MDR-TB, of whom 78 (95%) had no previous history of TB. Annually, 1–6 pediatric MDR-TB cases were reported (0.4%–2.6% of pediatric TB cases with DST results) (Supplementary Figure 1).
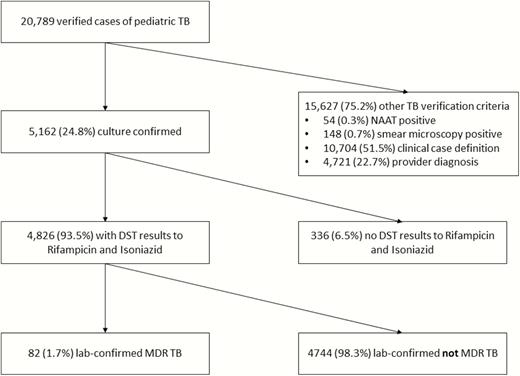
Flowchart of all verified pediatric tuberculosis cases reported from 1993 to 2014 and laboratory-confirmed multidrug-resistant tuberculosis cases. Abbreviations: DST, drug susceptibility test; MDR-TB, multidrug-resistant tuberculosis; NAAT, nucleic acid amplification test; TB, tuberculosis.
Most laboratory-confirmed pediatric MDR-TB cases were female (n = 51 [62%]) and one-third were of Hispanic ethnicity (n = 28 [34%]) (Supplementary Table 1). The median age was 5 years (interquartile range [IQR], 1–12 years). Two-thirds (n = 55 [67%]) were US-born persons. Twenty-two states reported ≥1 pediatric MDR-TB case, but >60% of cases occurred in 5 states. Most pediatric MDR-TB cases had pulmonary involvement only (n = 55 [67%]) (Supplementary Table 2).
Pediatric Multidrug-Resistant Tuberculosis by Age Group
Younger children aged <1 year and 1–4 years were more likely to be born in the United States (88% and 92%, respectively) than older children aged 5–9 years and 10–14 years (47% and 44%, respectively) (P = .0003; Table 1). Most children aged 10–14 years had positive sputum culture (82%) compared with younger children (<1 year: 13%; 1–4 years: 17%; 5–9 years: 20%; P < .0001). A large proportion of young children had positive cultures from gastric aspirates (<1 year: 56%; 1–4 years: 54%).
Sociodemographic and Clinical Characteristics of Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis in the United States by Age Group, 1993–2014 (n = 82)
| Characteristic . | Variable . | Age Group, y . | . | ||||
|---|---|---|---|---|---|---|---|
| <1 . | 1–4 . | 5–9 . | 10–14 . | P Value . | |||
| Sex | Male | 5 (31) | 9 (38) | 6 (40) | 11 (41) | ||
| Female | 11 (69) | 15 (62) | 9 (60) | 16 (59) | .9 | ||
| Race/ethnicity | Asian | 0 (0) | 8 (33) | 5 (33) | 11 (41) | ||
| Black | 5 (31) | 5 (21) | 5 (33) | 6 (22) | |||
| Hispanic | 9 (56) | 7 (29) | 5 (33) | 7 (26) | |||
| White | 2 (12) | 2 (8) | 0 (0) | 1 (4) | |||
| Multiplea | 0 (0) | 1 (4) | 0 (0) | 0 (0) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 2 (7) | .1b | ||
| Reporting state | California | 1 (6) | 6 (25) | 3 (20) | 5 (19) | ||
| New York City | 6 (37) | 2 (8) | 4 (26) | 3 (11) | |||
| Minnesota | 0 (0) | 1 (4) | 3 (20) | 3 (11) | |||
| New Jersey | 2 (13) | 2 (8) | 1 (8) | 2 (7) | |||
| Texas | 2 (13) | 2 (8) | 0 (0) | 3 (11) | |||
| North Carolina | 1 (6) | 4 (17) | 0 (0) | 0 (0) | |||
| Other (16 states ≤3 cases) | 4 (25) | 7 (30) | 4 (26) | 11 (41) | .3b | ||
| Origin | US-born | 14 (87) | 22 (92) | 7 (47) | 12 (44) | ||
| Foreign-born | 2 (13) | 2 (8) | 8 (53) | 15 (56) | .0003 | ||
| Origin region among foreign-bornb (n = 27) | Africa | 1 (50) | 0 (0) | 3 (37) | 5 (33) | ||
| Southeast Asia | 0 (0) | 1 (50) | 2 (25) | 3 (20) | |||
| Americas | 1 (50) | 0 (0) | 1 (13) | 3 (20) | |||
| Western Pacific | 0 (0) | 0 (0) | 2 (25) | 3 (20) | |||
| Europe | 0 (0) | 1 (50) | 0 (0) | 1 (7) | .8b | ||
| Born in high MDR-TB burden countryc (n = 27) | 1 (50) | 1 (50) | 3 (38) | 7 (47) | 1.0b | ||
| Lived in US <1 y (n = 24) | 1 (100) | 2 (100) | 4 (57) | 9 (64) | .8d | ||
| Previous diagnosis of TB disease | Yes | 0 (0) | 1 (4) | 0 (0) | 2 (7) | ||
| No | 16 (100) | 22 (92) | 15 (100) | 25 (93) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 0 (0) | .8b | ||
| HIV statuse | Positive | 1 (7) | 0 (0) | 2 (15) | 2 (9) | ||
| Negative | 9 (60) | 8 (44) | 6 (46) | 16 (69) | |||
| Unknown | 5 (33) | 10 (56) | 5 (39) | 5 (22) | .3b | ||
| Site of disease | Pulmonary only | 12 (75) | 15 (62) | 7 (47) | 21 (78) | ||
| Extrapulmonary Only | 2 (12) | 5 (21) | 5 (33) | 3 (11) | |||
| Both | 2 (13) | 4 (17) | 3 (20) | 3 (11) | .5b | ||
| Abnormal initial chest radiograph | 13 (81) | 19 (79) | 9 (60) | 26 (96) | .02b | ||
| Positive culture specimen type | Sputum | 2 (13) | 4 (17) | 3 (20) | 22 (81) | ||
| Gastric aspirate | 9 (56) | 13 (54) | 5 (33) | 0 (0) | |||
| Bronchial fluid | 3 (19) | 1 (4) | 2 (13) | 1 (4) | |||
| Otherf | 2 (13) | 6 (25) | 5 (33) | 4 (15) | <.0001b | ||
| Characteristic . | Variable . | Age Group, y . | . | ||||
|---|---|---|---|---|---|---|---|
| <1 . | 1–4 . | 5–9 . | 10–14 . | P Value . | |||
| Sex | Male | 5 (31) | 9 (38) | 6 (40) | 11 (41) | ||
| Female | 11 (69) | 15 (62) | 9 (60) | 16 (59) | .9 | ||
| Race/ethnicity | Asian | 0 (0) | 8 (33) | 5 (33) | 11 (41) | ||
| Black | 5 (31) | 5 (21) | 5 (33) | 6 (22) | |||
| Hispanic | 9 (56) | 7 (29) | 5 (33) | 7 (26) | |||
| White | 2 (12) | 2 (8) | 0 (0) | 1 (4) | |||
| Multiplea | 0 (0) | 1 (4) | 0 (0) | 0 (0) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 2 (7) | .1b | ||
| Reporting state | California | 1 (6) | 6 (25) | 3 (20) | 5 (19) | ||
| New York City | 6 (37) | 2 (8) | 4 (26) | 3 (11) | |||
| Minnesota | 0 (0) | 1 (4) | 3 (20) | 3 (11) | |||
| New Jersey | 2 (13) | 2 (8) | 1 (8) | 2 (7) | |||
| Texas | 2 (13) | 2 (8) | 0 (0) | 3 (11) | |||
| North Carolina | 1 (6) | 4 (17) | 0 (0) | 0 (0) | |||
| Other (16 states ≤3 cases) | 4 (25) | 7 (30) | 4 (26) | 11 (41) | .3b | ||
| Origin | US-born | 14 (87) | 22 (92) | 7 (47) | 12 (44) | ||
| Foreign-born | 2 (13) | 2 (8) | 8 (53) | 15 (56) | .0003 | ||
| Origin region among foreign-bornb (n = 27) | Africa | 1 (50) | 0 (0) | 3 (37) | 5 (33) | ||
| Southeast Asia | 0 (0) | 1 (50) | 2 (25) | 3 (20) | |||
| Americas | 1 (50) | 0 (0) | 1 (13) | 3 (20) | |||
| Western Pacific | 0 (0) | 0 (0) | 2 (25) | 3 (20) | |||
| Europe | 0 (0) | 1 (50) | 0 (0) | 1 (7) | .8b | ||
| Born in high MDR-TB burden countryc (n = 27) | 1 (50) | 1 (50) | 3 (38) | 7 (47) | 1.0b | ||
| Lived in US <1 y (n = 24) | 1 (100) | 2 (100) | 4 (57) | 9 (64) | .8d | ||
| Previous diagnosis of TB disease | Yes | 0 (0) | 1 (4) | 0 (0) | 2 (7) | ||
| No | 16 (100) | 22 (92) | 15 (100) | 25 (93) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 0 (0) | .8b | ||
| HIV statuse | Positive | 1 (7) | 0 (0) | 2 (15) | 2 (9) | ||
| Negative | 9 (60) | 8 (44) | 6 (46) | 16 (69) | |||
| Unknown | 5 (33) | 10 (56) | 5 (39) | 5 (22) | .3b | ||
| Site of disease | Pulmonary only | 12 (75) | 15 (62) | 7 (47) | 21 (78) | ||
| Extrapulmonary Only | 2 (12) | 5 (21) | 5 (33) | 3 (11) | |||
| Both | 2 (13) | 4 (17) | 3 (20) | 3 (11) | .5b | ||
| Abnormal initial chest radiograph | 13 (81) | 19 (79) | 9 (60) | 26 (96) | .02b | ||
| Positive culture specimen type | Sputum | 2 (13) | 4 (17) | 3 (20) | 22 (81) | ||
| Gastric aspirate | 9 (56) | 13 (54) | 5 (33) | 0 (0) | |||
| Bronchial fluid | 3 (19) | 1 (4) | 2 (13) | 1 (4) | |||
| Otherf | 2 (13) | 6 (25) | 5 (33) | 4 (15) | <.0001b | ||
Data are presented as No. (%).
Abbreviations: HIV, human immunodeficiency virus; MDR-TB, multidrug-resistant tuberculosis; TB, tuberculosis.
aMultiple races reported.
bFisher’s exact test.
cBased on World Health Organization’s 27 high MDR-TB burden countries [1].
dKruskal-Wallis test.
eCalifornia HIV data missing from 2005 to 2010 (n = 13).
fOther specimen types include cerebrospinal fluid, lymph node, skeletal system, soft tissue, peritoneal fluid, pus, or unknown.
Sociodemographic and Clinical Characteristics of Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis in the United States by Age Group, 1993–2014 (n = 82)
| Characteristic . | Variable . | Age Group, y . | . | ||||
|---|---|---|---|---|---|---|---|
| <1 . | 1–4 . | 5–9 . | 10–14 . | P Value . | |||
| Sex | Male | 5 (31) | 9 (38) | 6 (40) | 11 (41) | ||
| Female | 11 (69) | 15 (62) | 9 (60) | 16 (59) | .9 | ||
| Race/ethnicity | Asian | 0 (0) | 8 (33) | 5 (33) | 11 (41) | ||
| Black | 5 (31) | 5 (21) | 5 (33) | 6 (22) | |||
| Hispanic | 9 (56) | 7 (29) | 5 (33) | 7 (26) | |||
| White | 2 (12) | 2 (8) | 0 (0) | 1 (4) | |||
| Multiplea | 0 (0) | 1 (4) | 0 (0) | 0 (0) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 2 (7) | .1b | ||
| Reporting state | California | 1 (6) | 6 (25) | 3 (20) | 5 (19) | ||
| New York City | 6 (37) | 2 (8) | 4 (26) | 3 (11) | |||
| Minnesota | 0 (0) | 1 (4) | 3 (20) | 3 (11) | |||
| New Jersey | 2 (13) | 2 (8) | 1 (8) | 2 (7) | |||
| Texas | 2 (13) | 2 (8) | 0 (0) | 3 (11) | |||
| North Carolina | 1 (6) | 4 (17) | 0 (0) | 0 (0) | |||
| Other (16 states ≤3 cases) | 4 (25) | 7 (30) | 4 (26) | 11 (41) | .3b | ||
| Origin | US-born | 14 (87) | 22 (92) | 7 (47) | 12 (44) | ||
| Foreign-born | 2 (13) | 2 (8) | 8 (53) | 15 (56) | .0003 | ||
| Origin region among foreign-bornb (n = 27) | Africa | 1 (50) | 0 (0) | 3 (37) | 5 (33) | ||
| Southeast Asia | 0 (0) | 1 (50) | 2 (25) | 3 (20) | |||
| Americas | 1 (50) | 0 (0) | 1 (13) | 3 (20) | |||
| Western Pacific | 0 (0) | 0 (0) | 2 (25) | 3 (20) | |||
| Europe | 0 (0) | 1 (50) | 0 (0) | 1 (7) | .8b | ||
| Born in high MDR-TB burden countryc (n = 27) | 1 (50) | 1 (50) | 3 (38) | 7 (47) | 1.0b | ||
| Lived in US <1 y (n = 24) | 1 (100) | 2 (100) | 4 (57) | 9 (64) | .8d | ||
| Previous diagnosis of TB disease | Yes | 0 (0) | 1 (4) | 0 (0) | 2 (7) | ||
| No | 16 (100) | 22 (92) | 15 (100) | 25 (93) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 0 (0) | .8b | ||
| HIV statuse | Positive | 1 (7) | 0 (0) | 2 (15) | 2 (9) | ||
| Negative | 9 (60) | 8 (44) | 6 (46) | 16 (69) | |||
| Unknown | 5 (33) | 10 (56) | 5 (39) | 5 (22) | .3b | ||
| Site of disease | Pulmonary only | 12 (75) | 15 (62) | 7 (47) | 21 (78) | ||
| Extrapulmonary Only | 2 (12) | 5 (21) | 5 (33) | 3 (11) | |||
| Both | 2 (13) | 4 (17) | 3 (20) | 3 (11) | .5b | ||
| Abnormal initial chest radiograph | 13 (81) | 19 (79) | 9 (60) | 26 (96) | .02b | ||
| Positive culture specimen type | Sputum | 2 (13) | 4 (17) | 3 (20) | 22 (81) | ||
| Gastric aspirate | 9 (56) | 13 (54) | 5 (33) | 0 (0) | |||
| Bronchial fluid | 3 (19) | 1 (4) | 2 (13) | 1 (4) | |||
| Otherf | 2 (13) | 6 (25) | 5 (33) | 4 (15) | <.0001b | ||
| Characteristic . | Variable . | Age Group, y . | . | ||||
|---|---|---|---|---|---|---|---|
| <1 . | 1–4 . | 5–9 . | 10–14 . | P Value . | |||
| Sex | Male | 5 (31) | 9 (38) | 6 (40) | 11 (41) | ||
| Female | 11 (69) | 15 (62) | 9 (60) | 16 (59) | .9 | ||
| Race/ethnicity | Asian | 0 (0) | 8 (33) | 5 (33) | 11 (41) | ||
| Black | 5 (31) | 5 (21) | 5 (33) | 6 (22) | |||
| Hispanic | 9 (56) | 7 (29) | 5 (33) | 7 (26) | |||
| White | 2 (12) | 2 (8) | 0 (0) | 1 (4) | |||
| Multiplea | 0 (0) | 1 (4) | 0 (0) | 0 (0) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 2 (7) | .1b | ||
| Reporting state | California | 1 (6) | 6 (25) | 3 (20) | 5 (19) | ||
| New York City | 6 (37) | 2 (8) | 4 (26) | 3 (11) | |||
| Minnesota | 0 (0) | 1 (4) | 3 (20) | 3 (11) | |||
| New Jersey | 2 (13) | 2 (8) | 1 (8) | 2 (7) | |||
| Texas | 2 (13) | 2 (8) | 0 (0) | 3 (11) | |||
| North Carolina | 1 (6) | 4 (17) | 0 (0) | 0 (0) | |||
| Other (16 states ≤3 cases) | 4 (25) | 7 (30) | 4 (26) | 11 (41) | .3b | ||
| Origin | US-born | 14 (87) | 22 (92) | 7 (47) | 12 (44) | ||
| Foreign-born | 2 (13) | 2 (8) | 8 (53) | 15 (56) | .0003 | ||
| Origin region among foreign-bornb (n = 27) | Africa | 1 (50) | 0 (0) | 3 (37) | 5 (33) | ||
| Southeast Asia | 0 (0) | 1 (50) | 2 (25) | 3 (20) | |||
| Americas | 1 (50) | 0 (0) | 1 (13) | 3 (20) | |||
| Western Pacific | 0 (0) | 0 (0) | 2 (25) | 3 (20) | |||
| Europe | 0 (0) | 1 (50) | 0 (0) | 1 (7) | .8b | ||
| Born in high MDR-TB burden countryc (n = 27) | 1 (50) | 1 (50) | 3 (38) | 7 (47) | 1.0b | ||
| Lived in US <1 y (n = 24) | 1 (100) | 2 (100) | 4 (57) | 9 (64) | .8d | ||
| Previous diagnosis of TB disease | Yes | 0 (0) | 1 (4) | 0 (0) | 2 (7) | ||
| No | 16 (100) | 22 (92) | 15 (100) | 25 (93) | |||
| Unknown | 0 (0) | 1 (4) | 0 (0) | 0 (0) | .8b | ||
| HIV statuse | Positive | 1 (7) | 0 (0) | 2 (15) | 2 (9) | ||
| Negative | 9 (60) | 8 (44) | 6 (46) | 16 (69) | |||
| Unknown | 5 (33) | 10 (56) | 5 (39) | 5 (22) | .3b | ||
| Site of disease | Pulmonary only | 12 (75) | 15 (62) | 7 (47) | 21 (78) | ||
| Extrapulmonary Only | 2 (12) | 5 (21) | 5 (33) | 3 (11) | |||
| Both | 2 (13) | 4 (17) | 3 (20) | 3 (11) | .5b | ||
| Abnormal initial chest radiograph | 13 (81) | 19 (79) | 9 (60) | 26 (96) | .02b | ||
| Positive culture specimen type | Sputum | 2 (13) | 4 (17) | 3 (20) | 22 (81) | ||
| Gastric aspirate | 9 (56) | 13 (54) | 5 (33) | 0 (0) | |||
| Bronchial fluid | 3 (19) | 1 (4) | 2 (13) | 1 (4) | |||
| Otherf | 2 (13) | 6 (25) | 5 (33) | 4 (15) | <.0001b | ||
Data are presented as No. (%).
Abbreviations: HIV, human immunodeficiency virus; MDR-TB, multidrug-resistant tuberculosis; TB, tuberculosis.
aMultiple races reported.
bFisher’s exact test.
cBased on World Health Organization’s 27 high MDR-TB burden countries [1].
dKruskal-Wallis test.
eCalifornia HIV data missing from 2005 to 2010 (n = 13).
fOther specimen types include cerebrospinal fluid, lymph node, skeletal system, soft tissue, peritoneal fluid, pus, or unknown.
Drug Resistance
Of the 82 laboratory-confirmed MDR-TB cases, all had DST results to ≥1 first-line drug in addition to isoniazid and rifampicin, and 73 (89%) had results to ≥1 second-line drug (Table 2). Most pediatric MDR-TB cases had TB with additional resistance to ≥1 other first-line drug (66 [81%]). Of those tested, almost one-third had TB resistant to ≥1 second-line drug (24/73).
Additional Drug Resistance of Mycobacterium tuberculosis Isolates From Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis in the United States, 1993–2014 (n = 82)
| Drug Category . | Tested . | Resistant . | |
|---|---|---|---|
| No. . | No. . | (%) . | |
| Other first-line drugs | 82 | 66 | (81) |
| Ethambutol | 81 | 47 | (58) |
| Pyrazinamide | 70 | 36 | (51) |
| Streptomycin | 80 | 56 | (70) |
| Second-line drugs | 73 | 24 | (33) |
| Any second-line injectable | 68 | 10 | (15) |
| Any fluoroquinolone | 57 | 5 | (9) |
| Extensive drug resistancea | 54 | 3 | (6) |
| Other second-line drugsb | 70 | 15 | (21) |
| Drug Category . | Tested . | Resistant . | |
|---|---|---|---|
| No. . | No. . | (%) . | |
| Other first-line drugs | 82 | 66 | (81) |
| Ethambutol | 81 | 47 | (58) |
| Pyrazinamide | 70 | 36 | (51) |
| Streptomycin | 80 | 56 | (70) |
| Second-line drugs | 73 | 24 | (33) |
| Any second-line injectable | 68 | 10 | (15) |
| Any fluoroquinolone | 57 | 5 | (9) |
| Extensive drug resistancea | 54 | 3 | (6) |
| Other second-line drugsb | 70 | 15 | (21) |
Multidrug-resistant tuberculosis = Mycobacterium tuberculosis resistant to isoniazid and rifampicin.
aResistance to a fluoroquinolone and ≥1 second-line injectable.
bCycloserine, ethionamide, para-aminosalicylic acid.
Additional Drug Resistance of Mycobacterium tuberculosis Isolates From Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis in the United States, 1993–2014 (n = 82)
| Drug Category . | Tested . | Resistant . | |
|---|---|---|---|
| No. . | No. . | (%) . | |
| Other first-line drugs | 82 | 66 | (81) |
| Ethambutol | 81 | 47 | (58) |
| Pyrazinamide | 70 | 36 | (51) |
| Streptomycin | 80 | 56 | (70) |
| Second-line drugs | 73 | 24 | (33) |
| Any second-line injectable | 68 | 10 | (15) |
| Any fluoroquinolone | 57 | 5 | (9) |
| Extensive drug resistancea | 54 | 3 | (6) |
| Other second-line drugsb | 70 | 15 | (21) |
| Drug Category . | Tested . | Resistant . | |
|---|---|---|---|
| No. . | No. . | (%) . | |
| Other first-line drugs | 82 | 66 | (81) |
| Ethambutol | 81 | 47 | (58) |
| Pyrazinamide | 70 | 36 | (51) |
| Streptomycin | 80 | 56 | (70) |
| Second-line drugs | 73 | 24 | (33) |
| Any second-line injectable | 68 | 10 | (15) |
| Any fluoroquinolone | 57 | 5 | (9) |
| Extensive drug resistancea | 54 | 3 | (6) |
| Other second-line drugsb | 70 | 15 | (21) |
Multidrug-resistant tuberculosis = Mycobacterium tuberculosis resistant to isoniazid and rifampicin.
aResistance to a fluoroquinolone and ≥1 second-line injectable.
bCycloserine, ethionamide, para-aminosalicylic acid.
Initial Treatment Regimen, Duration, and Treatment Outcomes
Among 80 pediatric MDR-TB cases alive at diagnosis, most (n = 77 [96%]) were initially treated with only first-line drugs (Supplementary Figure 2). Median duration of treatment was 20 months (IQR, 15–24 months) (Table 3). Among the 77 who started treatment prior to 2013, 66 (86%) completed treatment; 4 (5%) died; 5 (6%) were lost, refused treatment, or moved; and 2 (3%) had no treatment outcome documented. Among the 21 (68%) with documented culture conversion, the median time to conversion was 2 months (IQR, 1–4 months).
Treatment Characteristics and Outcomes Among Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis Started on Treatment, 1993–2012a (n = 77)
| Characteristic . | No. (%) . |
|---|---|
| Duration, mo, median (IQR) (n = 75) | 20 (15–24) |
| Sputum culture conversion (n = 31)b | |
| Yes | 21 (68) |
| No | 7 (22) |
| Unknown | 3 (10) |
| Months to culture conversion, median (IQR) (n = 21) | 2 (1–4) |
| Reason therapy stopped | |
| Completed therapy | 66 (86) |
| Died | 4 (5) |
| Lost or refused | 2 (3) |
| Moved, unknown outcome | 3 (3) |
| Not documented | 2 (3) |
| Characteristic . | No. (%) . |
|---|---|
| Duration, mo, median (IQR) (n = 75) | 20 (15–24) |
| Sputum culture conversion (n = 31)b | |
| Yes | 21 (68) |
| No | 7 (22) |
| Unknown | 3 (10) |
| Months to culture conversion, median (IQR) (n = 21) | 2 (1–4) |
| Reason therapy stopped | |
| Completed therapy | 66 (86) |
| Died | 4 (5) |
| Lost or refused | 2 (3) |
| Moved, unknown outcome | 3 (3) |
| Not documented | 2 (3) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviation: IQR, interquartile range.
aAnalysis limited to 1993–2012 to allow for patients to complete 2 years of treatment for multidrug-resistant tuberculosis.
bCases with initial sputum culture positive.
Treatment Characteristics and Outcomes Among Children With Laboratory-Confirmed Multidrug-Resistant Tuberculosis Started on Treatment, 1993–2012a (n = 77)
| Characteristic . | No. (%) . |
|---|---|
| Duration, mo, median (IQR) (n = 75) | 20 (15–24) |
| Sputum culture conversion (n = 31)b | |
| Yes | 21 (68) |
| No | 7 (22) |
| Unknown | 3 (10) |
| Months to culture conversion, median (IQR) (n = 21) | 2 (1–4) |
| Reason therapy stopped | |
| Completed therapy | 66 (86) |
| Died | 4 (5) |
| Lost or refused | 2 (3) |
| Moved, unknown outcome | 3 (3) |
| Not documented | 2 (3) |
| Characteristic . | No. (%) . |
|---|---|
| Duration, mo, median (IQR) (n = 75) | 20 (15–24) |
| Sputum culture conversion (n = 31)b | |
| Yes | 21 (68) |
| No | 7 (22) |
| Unknown | 3 (10) |
| Months to culture conversion, median (IQR) (n = 21) | 2 (1–4) |
| Reason therapy stopped | |
| Completed therapy | 66 (86) |
| Died | 4 (5) |
| Lost or refused | 2 (3) |
| Moved, unknown outcome | 3 (3) |
| Not documented | 2 (3) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviation: IQR, interquartile range.
aAnalysis limited to 1993–2012 to allow for patients to complete 2 years of treatment for multidrug-resistant tuberculosis.
bCases with initial sputum culture positive.
Estimating Pediatric Multidrug-Resistant Tuberculosis
Of the 6 highest pediatric MDR-TB burden states/jurisdictions surveyed, 3 responded with information about empirically treated MDR-TB cases. California began recording such cases in 2002, Minnesota in 2010, and New York City (NYC) in 1993. Pediatric MDR-TB was underestimated by 55% (6 empiric MDR/11 total MDR), 50% (1/2), and 42% (11/26) in California, Minnesota, and NYC, respectively. All empiric MDR-TB cases received MDR-TB treatment because of known contact with an MDR-TB source case, in addition to clinical evidence of active TB disease. Children receiving empiric MDR-TB treatment were more likely to be 1–4 years old (78% vs 14%; P < .0001), have unknown HIV status (67% vs 28%; P = .04), or have received ethionamide in the initial regimen (50% vs 15%; P = .02) compared with laboratory-confirmed MDR-TB cases (Table 4).
Characteristics of Laboratory-Confirmed Versus Empiric Pediatric Multidrug-Resistant Tuberculosis, Participating US Jurisdictions (n = 39)
| Characteristic . | Laboratory-Confirmed MDR-TB (n = 21) . | Empiric MDR-TB (n = 18) . | P Value . |
|---|---|---|---|
| Female sex | 9 (43) | 12 (67) | .1 |
| Age, y | |||
| <1 | 6 (29) | 1 (6) | |
| 1–4 | 3 (14) | 14 (78) | |
| 5–9 | 7 (33) | 1 (6) | |
| 10–14 | 5 (24) | 2 (11) | <.0001a |
| Reporting state/jurisdiction | |||
| California | 5 (24) | 6 (33) | |
| Minnesota | 1 (5) | 1 (6) | |
| New York City | 15 (71) | 11 (61) | .8a |
| Race/ethnicity | |||
| Asian | 7 (33) | 2 (11) | |
| Black | 4 (19) | 8 (44) | |
| Hispanic | 9 (43) | 6 (33) | |
| White | 0 (0) | 1 (6) | |
| Multiple | 0 (0) | 1 (6) | |
| Unknown | 1 (5) | 0 (0) | .1a |
| US born | 17 (81) | 17 (94) | .3a |
| Previous TB diagnosis | 1 (5) | 0 (0) | 1a |
| Known HIV statusb (n = 30) | 13 (72) | 4 (33) | .04 |
| HIV positive among known statusb (n = 17) | 3 (23) | 0 (0) | .5a |
| Disease site | |||
| Pulmonary only | 13 (62) | 15 (83) | |
| Extrapulmonary only | 4 (19) | 1 (6) | |
| Both | 4 (19) | 2 (11) | .4a |
| Abnormal initial chest radiograph | 14 (67) | 17 (94) | .05a |
| Verification criteria | |||
| Laboratory confirmed | 21 (100) | 0 (0) | |
| Clinical case | 0 (0) | 9 (50) | |
| Provider diagnosis | 0 (0) | 9 (50) | <.0001a |
| Initial drug regimen (n = 38) | |||
| IR | 1 (5) | 0 (0) | |
| IRZ | 2 (10) | 0 (0) | |
| IRZE | 8 (38) | 6 (33) | |
| Multiple other drugs | 9 (43) | 12 (67) | .6a |
| Drugs/drug groups in initial regimen (n = 38) | |||
| Any first-line drug | 19 (95) | 16 (89) | .6a |
| Isoniazid | 14 (70) | 6 (33) | .02 |
| Rifampicin | 15 (75) | 7 (39) | .02 |
| Pyrazinamide | 16 (80) | 13 (72) | .7a |
| Ethambutol | 12 (60) | 12 (67) | .7 |
| Streptomycin | 3 (15) | 1 (6) | .6a |
| Any second-line drug | 7 (35) | 10 (56) | .2 |
| Fluoroquinolone | 3 (15) | 4 (22) | .7a |
| Second-line injectable | 5 (25) | 4 (22) | 1.0a |
| Ethionamide | 3 (15) | 9 (50) | .02 |
| Cycloserine | 6 (30) | 5 (28) | .9 |
| PAS | 0 (0) | 1 (6) | .5a |
| Treatment duration, mo, median (IQR) (n = 35)c | 20 (16–24) | 19 (18–21) | .8d |
| End of treatment outcome (n = 35)c | |||
| Completed | 14 (78) | 15 (88) | |
| Died | 2 (11) | 0 (0) | |
| Moved | 2 (11) | 2 (12) | .5a |
| Characteristic . | Laboratory-Confirmed MDR-TB (n = 21) . | Empiric MDR-TB (n = 18) . | P Value . |
|---|---|---|---|
| Female sex | 9 (43) | 12 (67) | .1 |
| Age, y | |||
| <1 | 6 (29) | 1 (6) | |
| 1–4 | 3 (14) | 14 (78) | |
| 5–9 | 7 (33) | 1 (6) | |
| 10–14 | 5 (24) | 2 (11) | <.0001a |
| Reporting state/jurisdiction | |||
| California | 5 (24) | 6 (33) | |
| Minnesota | 1 (5) | 1 (6) | |
| New York City | 15 (71) | 11 (61) | .8a |
| Race/ethnicity | |||
| Asian | 7 (33) | 2 (11) | |
| Black | 4 (19) | 8 (44) | |
| Hispanic | 9 (43) | 6 (33) | |
| White | 0 (0) | 1 (6) | |
| Multiple | 0 (0) | 1 (6) | |
| Unknown | 1 (5) | 0 (0) | .1a |
| US born | 17 (81) | 17 (94) | .3a |
| Previous TB diagnosis | 1 (5) | 0 (0) | 1a |
| Known HIV statusb (n = 30) | 13 (72) | 4 (33) | .04 |
| HIV positive among known statusb (n = 17) | 3 (23) | 0 (0) | .5a |
| Disease site | |||
| Pulmonary only | 13 (62) | 15 (83) | |
| Extrapulmonary only | 4 (19) | 1 (6) | |
| Both | 4 (19) | 2 (11) | .4a |
| Abnormal initial chest radiograph | 14 (67) | 17 (94) | .05a |
| Verification criteria | |||
| Laboratory confirmed | 21 (100) | 0 (0) | |
| Clinical case | 0 (0) | 9 (50) | |
| Provider diagnosis | 0 (0) | 9 (50) | <.0001a |
| Initial drug regimen (n = 38) | |||
| IR | 1 (5) | 0 (0) | |
| IRZ | 2 (10) | 0 (0) | |
| IRZE | 8 (38) | 6 (33) | |
| Multiple other drugs | 9 (43) | 12 (67) | .6a |
| Drugs/drug groups in initial regimen (n = 38) | |||
| Any first-line drug | 19 (95) | 16 (89) | .6a |
| Isoniazid | 14 (70) | 6 (33) | .02 |
| Rifampicin | 15 (75) | 7 (39) | .02 |
| Pyrazinamide | 16 (80) | 13 (72) | .7a |
| Ethambutol | 12 (60) | 12 (67) | .7 |
| Streptomycin | 3 (15) | 1 (6) | .6a |
| Any second-line drug | 7 (35) | 10 (56) | .2 |
| Fluoroquinolone | 3 (15) | 4 (22) | .7a |
| Second-line injectable | 5 (25) | 4 (22) | 1.0a |
| Ethionamide | 3 (15) | 9 (50) | .02 |
| Cycloserine | 6 (30) | 5 (28) | .9 |
| PAS | 0 (0) | 1 (6) | .5a |
| Treatment duration, mo, median (IQR) (n = 35)c | 20 (16–24) | 19 (18–21) | .8d |
| End of treatment outcome (n = 35)c | |||
| Completed | 14 (78) | 15 (88) | |
| Died | 2 (11) | 0 (0) | |
| Moved | 2 (11) | 2 (12) | .5a |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: HIV, human immunodeficiency virus; IQR, interquartile range; IR, isoniazid and rifampicin only; IRZ, isoniazid, rifampicin, and pyrazinamide; IRZE, isoniazid, rifampicin, pyrazinamide, and ethambutol; MDR-TB, multidrug-resistant tuberculosis; PAS, para-aminosalicylic acid; TB, tuberculosis; US, United States.
aFisher’s exact test.
bCalifornia HIV data missing from 2005 to 2010 (n = 9).
cAlive at diagnosis, started treatment prior to 2013, and had a documented reason that therapy stopped.
dKruskal-Wallis test.
Characteristics of Laboratory-Confirmed Versus Empiric Pediatric Multidrug-Resistant Tuberculosis, Participating US Jurisdictions (n = 39)
| Characteristic . | Laboratory-Confirmed MDR-TB (n = 21) . | Empiric MDR-TB (n = 18) . | P Value . |
|---|---|---|---|
| Female sex | 9 (43) | 12 (67) | .1 |
| Age, y | |||
| <1 | 6 (29) | 1 (6) | |
| 1–4 | 3 (14) | 14 (78) | |
| 5–9 | 7 (33) | 1 (6) | |
| 10–14 | 5 (24) | 2 (11) | <.0001a |
| Reporting state/jurisdiction | |||
| California | 5 (24) | 6 (33) | |
| Minnesota | 1 (5) | 1 (6) | |
| New York City | 15 (71) | 11 (61) | .8a |
| Race/ethnicity | |||
| Asian | 7 (33) | 2 (11) | |
| Black | 4 (19) | 8 (44) | |
| Hispanic | 9 (43) | 6 (33) | |
| White | 0 (0) | 1 (6) | |
| Multiple | 0 (0) | 1 (6) | |
| Unknown | 1 (5) | 0 (0) | .1a |
| US born | 17 (81) | 17 (94) | .3a |
| Previous TB diagnosis | 1 (5) | 0 (0) | 1a |
| Known HIV statusb (n = 30) | 13 (72) | 4 (33) | .04 |
| HIV positive among known statusb (n = 17) | 3 (23) | 0 (0) | .5a |
| Disease site | |||
| Pulmonary only | 13 (62) | 15 (83) | |
| Extrapulmonary only | 4 (19) | 1 (6) | |
| Both | 4 (19) | 2 (11) | .4a |
| Abnormal initial chest radiograph | 14 (67) | 17 (94) | .05a |
| Verification criteria | |||
| Laboratory confirmed | 21 (100) | 0 (0) | |
| Clinical case | 0 (0) | 9 (50) | |
| Provider diagnosis | 0 (0) | 9 (50) | <.0001a |
| Initial drug regimen (n = 38) | |||
| IR | 1 (5) | 0 (0) | |
| IRZ | 2 (10) | 0 (0) | |
| IRZE | 8 (38) | 6 (33) | |
| Multiple other drugs | 9 (43) | 12 (67) | .6a |
| Drugs/drug groups in initial regimen (n = 38) | |||
| Any first-line drug | 19 (95) | 16 (89) | .6a |
| Isoniazid | 14 (70) | 6 (33) | .02 |
| Rifampicin | 15 (75) | 7 (39) | .02 |
| Pyrazinamide | 16 (80) | 13 (72) | .7a |
| Ethambutol | 12 (60) | 12 (67) | .7 |
| Streptomycin | 3 (15) | 1 (6) | .6a |
| Any second-line drug | 7 (35) | 10 (56) | .2 |
| Fluoroquinolone | 3 (15) | 4 (22) | .7a |
| Second-line injectable | 5 (25) | 4 (22) | 1.0a |
| Ethionamide | 3 (15) | 9 (50) | .02 |
| Cycloserine | 6 (30) | 5 (28) | .9 |
| PAS | 0 (0) | 1 (6) | .5a |
| Treatment duration, mo, median (IQR) (n = 35)c | 20 (16–24) | 19 (18–21) | .8d |
| End of treatment outcome (n = 35)c | |||
| Completed | 14 (78) | 15 (88) | |
| Died | 2 (11) | 0 (0) | |
| Moved | 2 (11) | 2 (12) | .5a |
| Characteristic . | Laboratory-Confirmed MDR-TB (n = 21) . | Empiric MDR-TB (n = 18) . | P Value . |
|---|---|---|---|
| Female sex | 9 (43) | 12 (67) | .1 |
| Age, y | |||
| <1 | 6 (29) | 1 (6) | |
| 1–4 | 3 (14) | 14 (78) | |
| 5–9 | 7 (33) | 1 (6) | |
| 10–14 | 5 (24) | 2 (11) | <.0001a |
| Reporting state/jurisdiction | |||
| California | 5 (24) | 6 (33) | |
| Minnesota | 1 (5) | 1 (6) | |
| New York City | 15 (71) | 11 (61) | .8a |
| Race/ethnicity | |||
| Asian | 7 (33) | 2 (11) | |
| Black | 4 (19) | 8 (44) | |
| Hispanic | 9 (43) | 6 (33) | |
| White | 0 (0) | 1 (6) | |
| Multiple | 0 (0) | 1 (6) | |
| Unknown | 1 (5) | 0 (0) | .1a |
| US born | 17 (81) | 17 (94) | .3a |
| Previous TB diagnosis | 1 (5) | 0 (0) | 1a |
| Known HIV statusb (n = 30) | 13 (72) | 4 (33) | .04 |
| HIV positive among known statusb (n = 17) | 3 (23) | 0 (0) | .5a |
| Disease site | |||
| Pulmonary only | 13 (62) | 15 (83) | |
| Extrapulmonary only | 4 (19) | 1 (6) | |
| Both | 4 (19) | 2 (11) | .4a |
| Abnormal initial chest radiograph | 14 (67) | 17 (94) | .05a |
| Verification criteria | |||
| Laboratory confirmed | 21 (100) | 0 (0) | |
| Clinical case | 0 (0) | 9 (50) | |
| Provider diagnosis | 0 (0) | 9 (50) | <.0001a |
| Initial drug regimen (n = 38) | |||
| IR | 1 (5) | 0 (0) | |
| IRZ | 2 (10) | 0 (0) | |
| IRZE | 8 (38) | 6 (33) | |
| Multiple other drugs | 9 (43) | 12 (67) | .6a |
| Drugs/drug groups in initial regimen (n = 38) | |||
| Any first-line drug | 19 (95) | 16 (89) | .6a |
| Isoniazid | 14 (70) | 6 (33) | .02 |
| Rifampicin | 15 (75) | 7 (39) | .02 |
| Pyrazinamide | 16 (80) | 13 (72) | .7a |
| Ethambutol | 12 (60) | 12 (67) | .7 |
| Streptomycin | 3 (15) | 1 (6) | .6a |
| Any second-line drug | 7 (35) | 10 (56) | .2 |
| Fluoroquinolone | 3 (15) | 4 (22) | .7a |
| Second-line injectable | 5 (25) | 4 (22) | 1.0a |
| Ethionamide | 3 (15) | 9 (50) | .02 |
| Cycloserine | 6 (30) | 5 (28) | .9 |
| PAS | 0 (0) | 1 (6) | .5a |
| Treatment duration, mo, median (IQR) (n = 35)c | 20 (16–24) | 19 (18–21) | .8d |
| End of treatment outcome (n = 35)c | |||
| Completed | 14 (78) | 15 (88) | |
| Died | 2 (11) | 0 (0) | |
| Moved | 2 (11) | 2 (12) | .5a |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: HIV, human immunodeficiency virus; IQR, interquartile range; IR, isoniazid and rifampicin only; IRZ, isoniazid, rifampicin, and pyrazinamide; IRZE, isoniazid, rifampicin, pyrazinamide, and ethambutol; MDR-TB, multidrug-resistant tuberculosis; PAS, para-aminosalicylic acid; TB, tuberculosis; US, United States.
aFisher’s exact test.
bCalifornia HIV data missing from 2005 to 2010 (n = 9).
cAlive at diagnosis, started treatment prior to 2013, and had a documented reason that therapy stopped.
dKruskal-Wallis test.
DISCUSSION
This is the first nationally representative description of the epidemiology of pediatric MDR-TB in the United States. The prevalence of laboratory-confirmed MDR-TB among children with TB from 1993 to 2014 (1.7%) was lower than the estimated Americas regional (2.2%) and global (3.2%) prevalence, and similar to the overall prevalence of MDR-TB in the United States (1.5%) [5, 16]. Although MDR-TB treatment is complicated and toxic, children in this cohort responded to treatment better than adults with MDR-TB in the United States and globally, and similarly to other cohorts of children receiving individualized MDR-TB treatment [20–23]. Importantly, two-thirds of all pediatric MDR-TB cases were US-born and nearly all younger children (<5 years) were US-born, likely reflecting transmission of MDR-TB in the United States. TB disease in children often represents recent transmission, with most disease manifestations in children occurring in the first 6–12 months following primary infection [2, 24]. Our findings underscore the importance of quickly starting appropriate treatment and initiating active contact investigation of all pulmonary MDR-TB cases to prevent transmission to children and others in the home or in the community.
Diagnosing MDR-TB in children can be challenging due to paucibacillary disease and difficulty with sputum expectoration. We found that children aged <5 years with confirmed MDR-TB were less likely to have positive cultures from sputum specimens. Most positive cultures among this age group were from specimens that require more invasive procedures (ie, gastric aspiration). Induced sputum has been shown to have similar yield to gastric aspirate and offers a safe, simple alternative that can be done in an outpatient setting with proper staff training [25]. Newer molecular diagnostics may decrease time to detection of TB and drug resistance compared to culture-based methods, but the sensitivity of these tests are less than culture and the difficulty of specimen collection among young children remains [26]. Studies are needed, and some are under way, to determine biomarkers of TB disease in specimens that are easily obtainable from young children [27].
Because MDR-TB diagnosis requires laboratory confirmation, MDR-TB burden among children may be underdiagnosed and, therefore, underestimated worldwide. Of all pediatric TB cases in the United States since 1993, only 25% were culture confirmed and 23% had DST results. Thus, case counts that rely solely on laboratory diagnosis are likely to represent a fraction of the actual burden. Our study sought to expand the definition of pediatric MDR-TB to include clinically diagnosed cases who were treated for MDR-TB based on epidemiologic and clinical criteria, similar to “probable MDR-TB disease” defined by the Sentinel Project on Pediatric Drug-Resistant Tuberculosis [28]. Our survey of several states/jurisdictions found that 42%–55% of children treated for MDR-TB would not be counted as MDR-TB cases using current case definitions reliant on laboratory confirmation. A previous study in NYC similarly found that 13 of 20 (65%) pediatric TB cases treated for MDR-TB did not have laboratory confirmation and treatment instead relied on source-case DST [22]. Considering only laboratory-confirmed MDR-TB among children fails to capture the complex treatment and case management work performed by the state and local health departments. A more inclusive definition would help national, state, and local health departments understand their MDR-TB burden and better align program and funding needs.
All children treated empirically for MDR-TB were contacts to an MDR-TB case and met the clinical case definition for TB. Most were <5 years of age, reflecting the difficulty of laboratory diagnosis in young children. Whereas most laboratory-confirmed MDR-TB cases received rifampicin and isoniazid in the initial regimen, most empiric MDR-TB cases did not. According to national guidelines, children found to have MDR-TB through contact tracing should receive treatment according to the source case’s DST results [29]. Children without a known MDR-TB contact or other risk factors for MDR-TB would be started on first-line therapy until DST results are available. As DST can take weeks to months for results, the initial regimen reported likely does not reflect the effective regimen that the patient received. Treatment outcomes were good in both groups; however, quicker diagnoses and source case investigation to guide effective treatment may improve outcomes further.
We recognize that a more inclusive case definition could result in overestimation and misdiagnosis of pediatric MDR-TB without clearly defined epidemiologic and clinical criteria to guide treatment decisions. Even though children often have few side effects from second-line drugs and none of the children in this cohort stopped treatment due to adverse drug reactions, the risk of hearing loss and other adverse drug reactions is greater than with first-line treatment [30]. To lessen the risk of overdiagnosis, thorough clinical investigation is imperative. Thorough source case investigation may be more critical when the clinical investigation is not successful in determining drug susceptibility. Even in locations with high TB transmission, the presumed source case’s DST results have been found to be highly relevant and should guide initial management [31]. Frontline health workers are a key aspect of complete source case investigations and contact tracing. For example, understanding community dynamics and childcare strategies can help identify others who spend time with the child but may not be part of the household.
This cohort may represent an underestimation of confirmed MDR-TB among children for 2013 and 2014 due to delays in DST result reporting. Initial DST results are sometimes reported months after the initial case report, and final DST results are reported once treatment has stopped. However, children often do not have many, if any, follow-up DST results due to specimen collection difficulties, paucibacillary nature of disease, and quick response to effective treatment. In addition, NTSS does not collect information about phenotypic DST results between initial and final DST, or any molecular assays that detect MDR-TB-associated mutations. These assays have become routine in the past decade, which may result in underestimation of confirmed MDR-TB in more-recent years. The small sample size of this cohort limited statistical power. Our analysis of MDR-TB treatment was limited to the initial regimen at the time the case was reported. This initial regimen likely does not represent the MDR-TB regimen because of inherent delays in diagnosis of drug resistance. This points to the need to collect supplemental surveillance information on treatment of MDR-TB cases. A study on MDR-TB treatment practices in the United States found a median of 7 regimen changes per patient during treatment [20]. Additional surveillance information on the treatment of MDR-TB cases may improve accuracy of national estimates, particularly for pediatric MDR-TB case counts.
Over the past 2 decades, the proportion of foreign-born individuals among all TB cases has increased to 66% and nearly all adult MDR-TB cases are foreign-born [16, 20]. However, this study illustrates that there is still MDR-TB transmission occurring in the United States as children serve as “sentinel” cases indicating recent transmission. Analyses of pediatric drug-resistant TB can be an additional tool to monitor changing DST profile of circulating strains. As the TB epidemic in the United States changes to mirror TB epidemics elsewhere, MDR-TB may become a greater concern. Providers should not only consider laboratory and clinical characteristics, but also epidemiologic characteristics, when deciding how to treat pediatric TB cases. Children who are clinically diagnosed and treated for MDR-TB most likely represent true cases of MDR-TB and should be monitored for case counts, not only to help TB control programs better forecast program needs, but to more accurately determine the burden of MDR-TB among children.
Until there are better laboratory diagnostics for children, pediatric MDR-TB will be underestimated globally. Including empiric MDR-TB diagnoses in national estimates may close the gap between the estimated burden and the reported burden.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank Sapna Bamrah Morris, Dawn Tuckey, Bruce Bradley, Vern Green, and Mark Miner from the Field Services Branch in the Division of Tuberculosis Elimination at the US Centers for Disease Control and Prevention (CDC) for facilitating communication with the state/jurisdiction TB programs. We acknowledge Doug Proops and Felicia Dworkin from the Bureau of Tuberculosis Control, NYC Department of Health and Mental Hygiene, for reviewing the regimens and helping characterize clinical MDR-TB cases. We also acknowledge all the state and local public health departments for their continuous efforts toward TB surveillance, control and elimination. Finally, we acknowledge all the children who have had the unfortunate circumstance of living with this disease and the caretakers who helped to diagnose and treat them.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References




