-
PDF
- Split View
-
Views
-
Cite
Cite
Anuradha Ganesan, Octavio Mesner, Jason F. Okulicz, Thomas O'Bryan, Robert G. Deiss, Tahaniyat Lalani, Timothy J. Whitman, Amy C. Weintrob, Grace Macalino, Brian K. Agan, for the Infectious Disease Clinical Research Program HIV/STI Working Group, A Single Dose of Benzathine Penicillin G Is as Effective as Multiple Doses of Benzathine Penicillin G for the Treatment of HIV-Infected Persons With Early Syphilis, Clinical Infectious Diseases, Volume 60, Issue 4, 15 February 2015, Pages 653–660, https://doi.org/10.1093/cid/ciu888
Close - Share Icon Share
We examined treatment responses in >400 cases of early syphilis in human immunodeficiency virus-infected individuals. Serologic outcomes did not vary as a function of the treatment regimen. These results support the use of a single dose of benzathine penicillin as treatment.
Background. Treatment guidelines recommend the use of a single dose of benzathine penicillin G (BPG) for treating early syphilis in human immunodeficiency virus (HIV)-infected persons. However, data supporting this recommendation are limited. We examined the efficacy of single-dose BPG in the US Military HIV Natural History Study.
Methods. Subjects were included if they met serologic criteria for syphilis (ie, a positive nontreponemal test [NTr] confirmed by treponemal testing). Response to treatment was assessed at 13 months and was defined by a ≥4-fold decline in NTr titer. Multivariate Cox proportional hazard regression models were utilized to examine factors associated with treatment response.
Results. Three hundred fifty subjects (99% male) contributed 478 cases. Three hundred ninety-three cases were treated exclusively with BPG (141 with 1 dose of BPG). Treatment response was the same among those receiving 1 or >1 dose of BPG (92%). In a multivariate analysis, older age (hazard ratio [HR], 0.82 per 10-year increase; 95% confidence interval [CI], .73–.93) was associated with delayed response to treatment. Higher pretreatment titers (reference NTr titer <1:64; HR, 1.94 [95% CI, 1.58–2.39]) and CD4 counts (HR, 1.07 for every 100-cell increase [95% CI, 1.01–1.12]) were associated with a faster response to treatment. Response was not affected by the number of BPG doses received (reference, 1 dose of BPG; HR, 1.11 [95% CI, .89–1.4]).
Conclusions. In this cohort, additional BPG doses did not affect treatment response. Our data support the current recommendations for the use of a single dose of BPG to treat HIV-infected persons with early syphilis.
(See the Editorial Commentary by Tuddenham and Ghanem on pages 661–3.)
Current treatment guidelines recommend the use of a single dose of 2.4 million units (MU) of benzathine penicillin G (BPG) for the treatment of early stages of syphilis regardless of human immunodeficiency virus (HIV) serostatus; however, compliance with this recommendation is variable [1]. In a recent survey, infectious disease consultants belonging to a sentinel network were questioned about their syphilis treatment practices [2]. The survey focused on areas of uncertainty and with limited evidence to guide practice, such as the management of HIV-infected individuals with secondary syphilis. Contrary to the recommendations, most respondents (62%) preferred the use of 3 doses of BPG (administered weekly) for the treatment of secondary syphilis in HIV-infected individuals [2]. The reluctance to use a single dose of BPG to treat early syphilis cases in HIV-infected persons probably relate to several well-recognized features of this infection and the recommended treatment. For one, cerebrospinal fluid abnormalities (in the absence of symptoms) are a common finding in both HIV-infected and uninfected individuals with primary, secondary, and early latent disease [3, 4]. Second, standard doses of BPG fail to achieve treponemicidal concentrations in the cerebrospinal fluid, leading to concerns about the adequacy of a single dose of BPG for the treatment of a disease that even in the earliest stages is widely disseminated and often involves the central nervous system [5–8]. Finally, data that support the use of a single dose of BPG in early syphilis are primarily from the pre-HIV era [9–11]. There is a paucity of information that supports the use of 1 dose of BPG to treat early syphilis in HIV-infected persons [12]. Hence, to assess the adequacy of the current recommendation, we performed a study designed to examine whether or not the dose and duration of BPG are significant modifiers of serologic response to treatment.
METHODS
Study Population
To achieve our objectives, we used data from the US Military HIV Natural History Study (NHS), a cohort comprised of Department of Defense beneficiaries [13]. NHS visits are conducted every 6 months during which participants undergo blood draws, are examined by a physician, and are interviewed by research personnel. During these interviews and through the abstraction of medical records, research personnel collect clinical information (to include syphilis diagnoses), syphilis treatment history, and results of testing performed outside the participating military treatment facilities. This substudy included participants followed in the NHS between 1 January 1986 and 27 August 2013. NHS participants with early syphilis were included if the episode met serologic criteria for syphilis (ie, a positive nontreponemal [NTr] test that was confirmed by treponemal testing), and if treatment, pretreatment, and posttreatment NTr titers drawn within 13 months of treatment were available.
Data Analysis and Definitions
Syphilis screening is performed using a NTr test, primarily the rapid plasma reagin (RPR) test. Positive NTr tests are confirmed using a licensed treponemal test. Before 2006, screening for syphilis was conducted in accordance with the policies of the military treatment facilities; since 2006, annual serologic testing has been incorporated in the NHS.
Syphilis staging has not been captured consistently in the NHS; hence, we used duration of syphilis infection as an approximation. We defined cases as “early” if there was a documented seroconversion (ie, from a negative to a positive NTr test) in the preceding 365 days. A single subject could contribute >1 case to this analysis, provided treatment and response to treatment for each case were clearly documented in the database (ie, following treatment a ≥4-fold decline in NTr titer was achieved at any time point thereafter, followed by a ≥4-fold increase in titer). Because behavioral data is difficult to ascertain, this definition has been used by some experts to discern relapse from reinfection [14]. To be considered an early case, the increase from the nadir titer was required to have occurred within 365 days. Subjects who did not respond to their initial treatment regimen could not contribute >1 case.
A case was considered treated if the treatment was administered within 6 weeks of the positive NTr titer. Response to treatment was defined as a ≥4-fold decline in NTr titer following 1 course of treatment. Among subjects whose pretreatment titer was ≤1:4, response to treatment was defined by seroreversion (ie, a switch from a positive to a negative NTr test). To categorize treatment response, we assessed response at 13 months instead of the recommended 365 days to allow for inclusion of subjects whose visits were delayed. We used the highest titer (in the 6 months preceding or in the 30 days after completion of treatment) to assess treatment response [15]. In this analysis, variables related to demographics (age, sex, ethnicity), HIV parameters (time updated CD4 counts, HIV RNA levels, and antiretroviral therapy use), and syphilis-specific variables (treatment regimen and pretreatment NTr titers) were examined. Highly active antiretroviral therapy (HAART) was defined as the use of 3 or more drugs belonging to ≥2 classes of antiretrovirals or the use of a triple-nucleotide regimen [16]. We categorized syphilis treatment as regimens that used BPG exclusively (ie, 1 or ≥2 doses of BPG only), or “other” regimens. Other regimens included penicillin-containing regimens, that is, where a penicillin derivative was used either alone or in combination with BPG or non-penicillin-containing regimen (eg, doxycycline, azithromycin, or ceftriaxone).
Statistical Methods
Descriptive statistics were used to describe the population. Univariate P value statistics for categorical factors were calculated using χ2 or Fisher exact test depending on cell count. For continuous variables, t tests and Wilcoxon tests were used, respectively, for variables with normal and nonnormal distribution.
Baseline for this analysis was defined as the date of treatment. Follow-up time was calculated from the start of therapy. The latest follow-up date was 27 August 2013.
Multivariate Cox proportional hazards models were used to assess factors associated with time to treatment response. Cases were censored at the time of their second course of treatment for the same episode, at last record of RPR titer, or death. Covariates were included based on clinical importance. These models were adjusted for within patient clustering. Significance of the multivariate model was set at P < .05; all P values are 2-sided. Hazard rates and ratios are presented with 95% confidence intervals (CIs). Analyses were conducted using the R package version 2.13.2.
To evaluate the effect of missing data (25% of all cases) we performed 2 sensitivity analyses. In the first, we evaluated syphilis cases after 1 January 2006. This date was chosen as routine syphilis screening was incorporated in the NHS after 1 January 2006, allowing for a more complete dataset. In the second, as missing pretreatment titers resulted in the exclusion of 14% of the cases, we used the first documented titer in lieu of the pretreatment titer. To evaluate whether the inclusion of multiple cases per subject affected our results, we performed an analysis restricted to subjects who contributed a single case. Finally we performed a sensitivity analysis to examine the effect of intercurrent antibiotics on treatment response.
RESULTS
Study Population
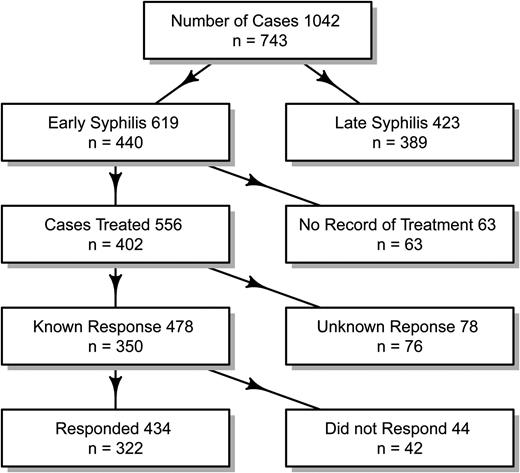
Graphical representation of the cases selected for this analysis. Although subjects could contribute >1 case to this analysis, subsequent cases were not included if treatment was not recorded for the preceding case. For this figure, response was assessed at 13 months following treatment.
Included subjects were predominantly men (99%); 63% self-identified as African American, 22% as white, and 14% as Hispanic/other (Table 1). Subjects were followed for a median of 11 years from their HIV diagnosis (IQR, 6–18 years). The median number of NTr tests recorded during follow up was 24 (IQR, 16–36). Participants excluded because of insufficient data (n = 90) were likely to be diagnosed with both their HIV infection (median, 1992 [IQR, 1987–2002] vs 1999 [IQR, 1991–2004]) and their first case of syphilis after their HIV diagnosis at an earlier calendar time (median, 2004 [1992–2009]) vs 2006 [IQR, 2002–2009]). As expected with an earlier year of diagnosis, they were less likely to be receiving HAART (37% vs 59%), had a higher viral load (3.4 log10 copies/mL [1.7–4.5] vs 2.4 log10 copies/mL [1.7–4.2]), and received an “other” regimen as treatment for their first case of syphilis (29% vs 18%). Of note, participants excluded from the analysis were as likely as included participants to have received a single dose of BPG (32% vs 30%) for treatment, and had similar CD4 counts when diagnosed with their first case of syphilis (503 cells/µL [IQR, 292–635] vs 483 cells/µL [IQR, 376–636]).
Baseline Characteristics of All Subjects With a Diagnosis of Early Syphilis in the Natural History Study
| Characteristics . | Total (n = 440) . | Includeda (n = 350) . | Excluded (n = 90) . | P Valueb . |
|---|---|---|---|---|
| Demographic | ||||
| Age at HIV diagnosis, y, median (IQR) | 28 (24–34) | 28 (24–33) | 29 (25–35) | .10 |
| Ethnicity | ||||
| White | 107 (24%) | 78 (22%) | 29 (32%) | .16 |
| African American | 276 (63%) | 222 (63%) | 54 (60%) | |
| Hispanic | 36 (8%) | 31 (9%) | 5 (6%) | |
| Other | 21 (5%) | 19 (5%) | 2 (2%) | |
| Sex | ||||
| Male | 435 (99%) | 347 (99%) | 88 (98%) | .27 |
| Female | 5 (1%) | 3 (1%) | 2 (2%) | |
| HIV-related variables | ||||
| Calendar year of HIV diagnosis, median (IQR) | 1997 (1989–2004) | 1999 (1991–2004) | 1992 (1987–2002) | <.001 |
| CD4 at HIV diagnosis, cells/µL, median (IQR) | 509 (348–649) | 506 (348–649) | 531 (356–653) | .48 |
| CD4 at first syphilis case, cells/µL, median (IQR) | 486 (362–636) | 483 (376–636) | 503 (292–635) | .47 |
| VL at first syphilis case, log10 copies/mL | 2.6 (1.7–4.3) | 2.4 (1.7–4.2) | 3.4 (1.7–4.5) | .04 |
| HAART use at first syphilis case | 55% | 59% | 37% | <.001 |
| Syphilis-related variables | ||||
| Calendar year of first syphilis case, median (IQR) | 2005 (2001–2009) | 2006 (2002–2009) | 2004 (1992–2009) | <.001 |
| Number of NTr tests recorded since HIV diagnosis, median (IQR) | 24 (15–35) | 24 (16–36) | 20 (10–28) | <.001 |
| Treatment | ||||
| 1 dose of BPG | 127 (31%) | 106 (30%) | 21 (32%) | .07 |
| ≥2 doses of BPG | 205 (50%) | 180 (52%) | 25 (38%) | |
| Other | 82 (20%) | 63 (18%) | 19 (29%) | |
| Characteristics . | Total (n = 440) . | Includeda (n = 350) . | Excluded (n = 90) . | P Valueb . |
|---|---|---|---|---|
| Demographic | ||||
| Age at HIV diagnosis, y, median (IQR) | 28 (24–34) | 28 (24–33) | 29 (25–35) | .10 |
| Ethnicity | ||||
| White | 107 (24%) | 78 (22%) | 29 (32%) | .16 |
| African American | 276 (63%) | 222 (63%) | 54 (60%) | |
| Hispanic | 36 (8%) | 31 (9%) | 5 (6%) | |
| Other | 21 (5%) | 19 (5%) | 2 (2%) | |
| Sex | ||||
| Male | 435 (99%) | 347 (99%) | 88 (98%) | .27 |
| Female | 5 (1%) | 3 (1%) | 2 (2%) | |
| HIV-related variables | ||||
| Calendar year of HIV diagnosis, median (IQR) | 1997 (1989–2004) | 1999 (1991–2004) | 1992 (1987–2002) | <.001 |
| CD4 at HIV diagnosis, cells/µL, median (IQR) | 509 (348–649) | 506 (348–649) | 531 (356–653) | .48 |
| CD4 at first syphilis case, cells/µL, median (IQR) | 486 (362–636) | 483 (376–636) | 503 (292–635) | .47 |
| VL at first syphilis case, log10 copies/mL | 2.6 (1.7–4.3) | 2.4 (1.7–4.2) | 3.4 (1.7–4.5) | .04 |
| HAART use at first syphilis case | 55% | 59% | 37% | <.001 |
| Syphilis-related variables | ||||
| Calendar year of first syphilis case, median (IQR) | 2005 (2001–2009) | 2006 (2002–2009) | 2004 (1992–2009) | <.001 |
| Number of NTr tests recorded since HIV diagnosis, median (IQR) | 24 (15–35) | 24 (16–36) | 20 (10–28) | <.001 |
| Treatment | ||||
| 1 dose of BPG | 127 (31%) | 106 (30%) | 21 (32%) | .07 |
| ≥2 doses of BPG | 205 (50%) | 180 (52%) | 25 (38%) | |
| Other | 82 (20%) | 63 (18%) | 19 (29%) | |
Data are presented as No. (%) unless otherwise specified. The numbers in bold represent statistically significant differences or associations.
Abbreviations: BPG, benzathine penicillin G; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; IQR, interquartile range; NTr, nontreponemal test; VL, viral load.
a Refers to subjects who contributed at least 1 evaluable episode.
b Comparing included and excluded subjects, using χ2 tests for categorical variables and Wilcoxon 2-sample tests for continuous variables.
Baseline Characteristics of All Subjects With a Diagnosis of Early Syphilis in the Natural History Study
| Characteristics . | Total (n = 440) . | Includeda (n = 350) . | Excluded (n = 90) . | P Valueb . |
|---|---|---|---|---|
| Demographic | ||||
| Age at HIV diagnosis, y, median (IQR) | 28 (24–34) | 28 (24–33) | 29 (25–35) | .10 |
| Ethnicity | ||||
| White | 107 (24%) | 78 (22%) | 29 (32%) | .16 |
| African American | 276 (63%) | 222 (63%) | 54 (60%) | |
| Hispanic | 36 (8%) | 31 (9%) | 5 (6%) | |
| Other | 21 (5%) | 19 (5%) | 2 (2%) | |
| Sex | ||||
| Male | 435 (99%) | 347 (99%) | 88 (98%) | .27 |
| Female | 5 (1%) | 3 (1%) | 2 (2%) | |
| HIV-related variables | ||||
| Calendar year of HIV diagnosis, median (IQR) | 1997 (1989–2004) | 1999 (1991–2004) | 1992 (1987–2002) | <.001 |
| CD4 at HIV diagnosis, cells/µL, median (IQR) | 509 (348–649) | 506 (348–649) | 531 (356–653) | .48 |
| CD4 at first syphilis case, cells/µL, median (IQR) | 486 (362–636) | 483 (376–636) | 503 (292–635) | .47 |
| VL at first syphilis case, log10 copies/mL | 2.6 (1.7–4.3) | 2.4 (1.7–4.2) | 3.4 (1.7–4.5) | .04 |
| HAART use at first syphilis case | 55% | 59% | 37% | <.001 |
| Syphilis-related variables | ||||
| Calendar year of first syphilis case, median (IQR) | 2005 (2001–2009) | 2006 (2002–2009) | 2004 (1992–2009) | <.001 |
| Number of NTr tests recorded since HIV diagnosis, median (IQR) | 24 (15–35) | 24 (16–36) | 20 (10–28) | <.001 |
| Treatment | ||||
| 1 dose of BPG | 127 (31%) | 106 (30%) | 21 (32%) | .07 |
| ≥2 doses of BPG | 205 (50%) | 180 (52%) | 25 (38%) | |
| Other | 82 (20%) | 63 (18%) | 19 (29%) | |
| Characteristics . | Total (n = 440) . | Includeda (n = 350) . | Excluded (n = 90) . | P Valueb . |
|---|---|---|---|---|
| Demographic | ||||
| Age at HIV diagnosis, y, median (IQR) | 28 (24–34) | 28 (24–33) | 29 (25–35) | .10 |
| Ethnicity | ||||
| White | 107 (24%) | 78 (22%) | 29 (32%) | .16 |
| African American | 276 (63%) | 222 (63%) | 54 (60%) | |
| Hispanic | 36 (8%) | 31 (9%) | 5 (6%) | |
| Other | 21 (5%) | 19 (5%) | 2 (2%) | |
| Sex | ||||
| Male | 435 (99%) | 347 (99%) | 88 (98%) | .27 |
| Female | 5 (1%) | 3 (1%) | 2 (2%) | |
| HIV-related variables | ||||
| Calendar year of HIV diagnosis, median (IQR) | 1997 (1989–2004) | 1999 (1991–2004) | 1992 (1987–2002) | <.001 |
| CD4 at HIV diagnosis, cells/µL, median (IQR) | 509 (348–649) | 506 (348–649) | 531 (356–653) | .48 |
| CD4 at first syphilis case, cells/µL, median (IQR) | 486 (362–636) | 483 (376–636) | 503 (292–635) | .47 |
| VL at first syphilis case, log10 copies/mL | 2.6 (1.7–4.3) | 2.4 (1.7–4.2) | 3.4 (1.7–4.5) | .04 |
| HAART use at first syphilis case | 55% | 59% | 37% | <.001 |
| Syphilis-related variables | ||||
| Calendar year of first syphilis case, median (IQR) | 2005 (2001–2009) | 2006 (2002–2009) | 2004 (1992–2009) | <.001 |
| Number of NTr tests recorded since HIV diagnosis, median (IQR) | 24 (15–35) | 24 (16–36) | 20 (10–28) | <.001 |
| Treatment | ||||
| 1 dose of BPG | 127 (31%) | 106 (30%) | 21 (32%) | .07 |
| ≥2 doses of BPG | 205 (50%) | 180 (52%) | 25 (38%) | |
| Other | 82 (20%) | 63 (18%) | 19 (29%) | |
Data are presented as No. (%) unless otherwise specified. The numbers in bold represent statistically significant differences or associations.
Abbreviations: BPG, benzathine penicillin G; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; IQR, interquartile range; NTr, nontreponemal test; VL, viral load.
a Refers to subjects who contributed at least 1 evaluable episode.
b Comparing included and excluded subjects, using χ2 tests for categorical variables and Wilcoxon 2-sample tests for continuous variables.
Characteristics of Syphilis Cases
The clinical characteristics of the 478 syphilis cases are illustrated in Table 2. A total of 141 (29%) of the studied cases were treated with 1 dose of BPG, whereas 252 (53%) cases were treated with ≥2 doses of BPG. Other regimens were used to treat 85 (18%) cases (70 used a penicillin-containing regimen and 15 a non-penicillin-based regimen). A majority of the cases occurred when patients were receiving HAART (69%), had a low viral load (median, 1.9 log10 copies/mL [IQR, 1.7–2.9]), and preserved CD4 counts (median, 494 cells/µL [IQR, 383–675]). The median pretreatment NTr titer for these cases was 1:64 [IQR, 1:16–1:128].
Clinical Characteristics of 478 Early Syphilis Cases Included in the Analysis
| Characteristic . | No. (%) or Median (IQR) . |
|---|---|
| Demographic | |
| Age at case, y | 37 (30–42) |
| Syphilis-related variables | |
| Calendar year of syphilis diagnosis | 2007 (2003–2010) |
| Calendar year of syphilis diagnosis | |
| 1986–2005 | 187 (39%) |
| 2006–2013 | 291 (61%) |
| RPR titer before treatment | 1:64 (1:16–1:128) |
| RPR titer before treatment <1:4 | 20 (4%) |
| Treatment regimens | |
| 1 dose of BPG | 141 (29%) |
| ≥2 doses of BPG | 252 (53%) |
| Other PCN regimens | 70 (15%) |
| Non PCN regimens | 15 (3%) |
| HAART use at the time of syphilis cases | 328 (69%) |
| CD4 at syphilis case, cells/µL | 494 (383–675) |
| Viral load at syphilis case, log10 copies/mL | 1.9 (1.7–3.9) |
| Characteristic . | No. (%) or Median (IQR) . |
|---|---|
| Demographic | |
| Age at case, y | 37 (30–42) |
| Syphilis-related variables | |
| Calendar year of syphilis diagnosis | 2007 (2003–2010) |
| Calendar year of syphilis diagnosis | |
| 1986–2005 | 187 (39%) |
| 2006–2013 | 291 (61%) |
| RPR titer before treatment | 1:64 (1:16–1:128) |
| RPR titer before treatment <1:4 | 20 (4%) |
| Treatment regimens | |
| 1 dose of BPG | 141 (29%) |
| ≥2 doses of BPG | 252 (53%) |
| Other PCN regimens | 70 (15%) |
| Non PCN regimens | 15 (3%) |
| HAART use at the time of syphilis cases | 328 (69%) |
| CD4 at syphilis case, cells/µL | 494 (383–675) |
| Viral load at syphilis case, log10 copies/mL | 1.9 (1.7–3.9) |
Abbreviations: BPG, benzathine penicillin G; HAART, highly active antiretroviral therapy; IQR, interquartile range; PCN, penicillin; RPR, rapid plasma reagin.
Clinical Characteristics of 478 Early Syphilis Cases Included in the Analysis
| Characteristic . | No. (%) or Median (IQR) . |
|---|---|
| Demographic | |
| Age at case, y | 37 (30–42) |
| Syphilis-related variables | |
| Calendar year of syphilis diagnosis | 2007 (2003–2010) |
| Calendar year of syphilis diagnosis | |
| 1986–2005 | 187 (39%) |
| 2006–2013 | 291 (61%) |
| RPR titer before treatment | 1:64 (1:16–1:128) |
| RPR titer before treatment <1:4 | 20 (4%) |
| Treatment regimens | |
| 1 dose of BPG | 141 (29%) |
| ≥2 doses of BPG | 252 (53%) |
| Other PCN regimens | 70 (15%) |
| Non PCN regimens | 15 (3%) |
| HAART use at the time of syphilis cases | 328 (69%) |
| CD4 at syphilis case, cells/µL | 494 (383–675) |
| Viral load at syphilis case, log10 copies/mL | 1.9 (1.7–3.9) |
| Characteristic . | No. (%) or Median (IQR) . |
|---|---|
| Demographic | |
| Age at case, y | 37 (30–42) |
| Syphilis-related variables | |
| Calendar year of syphilis diagnosis | 2007 (2003–2010) |
| Calendar year of syphilis diagnosis | |
| 1986–2005 | 187 (39%) |
| 2006–2013 | 291 (61%) |
| RPR titer before treatment | 1:64 (1:16–1:128) |
| RPR titer before treatment <1:4 | 20 (4%) |
| Treatment regimens | |
| 1 dose of BPG | 141 (29%) |
| ≥2 doses of BPG | 252 (53%) |
| Other PCN regimens | 70 (15%) |
| Non PCN regimens | 15 (3%) |
| HAART use at the time of syphilis cases | 328 (69%) |
| CD4 at syphilis case, cells/µL | 494 (383–675) |
| Viral load at syphilis case, log10 copies/mL | 1.9 (1.7–3.9) |
Abbreviations: BPG, benzathine penicillin G; HAART, highly active antiretroviral therapy; IQR, interquartile range; PCN, penicillin; RPR, rapid plasma reagin.
Serologic Response to Treatment
| Serologic Response . | Total (N = 478) . | 1 Dose of BPGa (n = 141) . | ≥2 Doses of BPGa (n = 252) . | Othera (n = 85) . |
|---|---|---|---|---|
| Serologic responseb | ||||
| 3 mo | 31% | 33% | 29% | 33% |
| 6 mo | 66% | 69% | 66% | 60% |
| 9 mo | 84% | 86% | 85% | 80% |
| 12 mo | 91% | 92% | 92% | 86% |
| 18 mo | 96% | 94% | 96% | 96% |
| 24 mo | 97% | 96% | 97% | 96% |
| Seroconversionsc | ||||
| 3 mo | 5% | 8% | 4% | 4% |
| 6 mo | 21% | 28% | 18% | 15% |
| 9 mo | 35% | 43% | 32% | 28% |
| 12 mo | 46% | 56% | 44% | 34% |
| 18 mo | 63% | 68% | 63% | 54% |
| 24 mo | 67% | 73% | 57% | 60% |
| Serologic Response . | Total (N = 478) . | 1 Dose of BPGa (n = 141) . | ≥2 Doses of BPGa (n = 252) . | Othera (n = 85) . |
|---|---|---|---|---|
| Serologic responseb | ||||
| 3 mo | 31% | 33% | 29% | 33% |
| 6 mo | 66% | 69% | 66% | 60% |
| 9 mo | 84% | 86% | 85% | 80% |
| 12 mo | 91% | 92% | 92% | 86% |
| 18 mo | 96% | 94% | 96% | 96% |
| 24 mo | 97% | 96% | 97% | 96% |
| Seroconversionsc | ||||
| 3 mo | 5% | 8% | 4% | 4% |
| 6 mo | 21% | 28% | 18% | 15% |
| 9 mo | 35% | 43% | 32% | 28% |
| 12 mo | 46% | 56% | 44% | 34% |
| 18 mo | 63% | 68% | 63% | 54% |
| 24 mo | 67% | 73% | 57% | 60% |
Abbreviations: BPG, benzathine penicillin G; HIV, human immunodeficiency virus.
a The results displayed refer to 3 different regimens, namely, 1 dose of BPG, ≥2 doses of BPG, or an “other regimen.”
b Proportion of subjects who exhibited response to therapy defined as a ≥4-fold decline in nontreponemal titer.
c Proportion of subjects who seroreverted following therapy (ie, a negative nontreponemal titer following therapy).
| Serologic Response . | Total (N = 478) . | 1 Dose of BPGa (n = 141) . | ≥2 Doses of BPGa (n = 252) . | Othera (n = 85) . |
|---|---|---|---|---|
| Serologic responseb | ||||
| 3 mo | 31% | 33% | 29% | 33% |
| 6 mo | 66% | 69% | 66% | 60% |
| 9 mo | 84% | 86% | 85% | 80% |
| 12 mo | 91% | 92% | 92% | 86% |
| 18 mo | 96% | 94% | 96% | 96% |
| 24 mo | 97% | 96% | 97% | 96% |
| Seroconversionsc | ||||
| 3 mo | 5% | 8% | 4% | 4% |
| 6 mo | 21% | 28% | 18% | 15% |
| 9 mo | 35% | 43% | 32% | 28% |
| 12 mo | 46% | 56% | 44% | 34% |
| 18 mo | 63% | 68% | 63% | 54% |
| 24 mo | 67% | 73% | 57% | 60% |
| Serologic Response . | Total (N = 478) . | 1 Dose of BPGa (n = 141) . | ≥2 Doses of BPGa (n = 252) . | Othera (n = 85) . |
|---|---|---|---|---|
| Serologic responseb | ||||
| 3 mo | 31% | 33% | 29% | 33% |
| 6 mo | 66% | 69% | 66% | 60% |
| 9 mo | 84% | 86% | 85% | 80% |
| 12 mo | 91% | 92% | 92% | 86% |
| 18 mo | 96% | 94% | 96% | 96% |
| 24 mo | 97% | 96% | 97% | 96% |
| Seroconversionsc | ||||
| 3 mo | 5% | 8% | 4% | 4% |
| 6 mo | 21% | 28% | 18% | 15% |
| 9 mo | 35% | 43% | 32% | 28% |
| 12 mo | 46% | 56% | 44% | 34% |
| 18 mo | 63% | 68% | 63% | 54% |
| 24 mo | 67% | 73% | 57% | 60% |
Abbreviations: BPG, benzathine penicillin G; HIV, human immunodeficiency virus.
a The results displayed refer to 3 different regimens, namely, 1 dose of BPG, ≥2 doses of BPG, or an “other regimen.”
b Proportion of subjects who exhibited response to therapy defined as a ≥4-fold decline in nontreponemal titer.
c Proportion of subjects who seroreverted following therapy (ie, a negative nontreponemal titer following therapy).
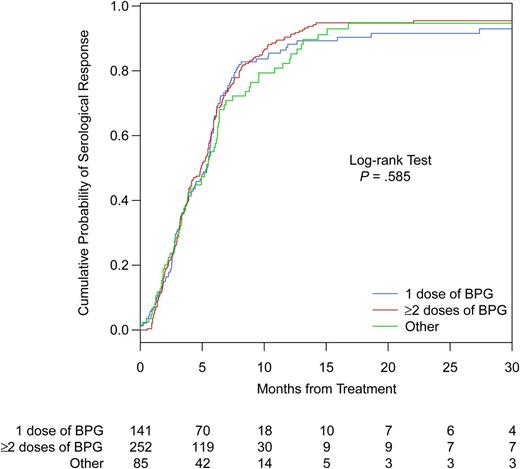
Kaplan–Meier curves, comparing time to serologic response in early syphilis cases treated with different therapeutic regimens. Abbreviation: BPG, benzathine penicillin G.
Factors Associated With Treatment Response
In a multivariate model that adjusted for baseline and time-updated covariates, older age (hazard ratio [HR], 0.82 per 10-year increase [95% CI, .73–.93]) was associated with delayed response. Higher pretreatment NTr titers (reference NTr titer <1:64: HR, 1.94 [95% CI, 1.58–2.39]) and higher CD4 counts at syphilis diagnosis (HR, 1.07 for every 100-cell increase [95% CI, 1.01–1.12]) were associated with a shorter time to observed response. Compared to single-dose BPG, response to treatment was similar among those who received ≥2 doses of BPG (reference, 1 dose of BPG: HR, 1.11 [95% CI, .89–1.4]) or an “other” regimen (reference, 1 dose of BPG: HR, 0.86 [95% CI, .62–1.2]). However, HAART use (reference not on HAART: HR, 1.24 [95% CI, .90–1.72]) and viral load (HR, 1.05 for each log increase in viral load [95% CI, .94–1.17]) were not associated with response to treatment (Table 4).
| Factor . | Multivariate HR (95% CI) . | P Value . |
|---|---|---|
| Demographics | ||
| Age at syphilis diagnosis (for every 10 y increase) | 0.82 (.73–.93) | .001 |
| Ethnicity | ||
| White | 1.0 | |
| African American | 0.87 (.66–1.15) | .33 |
| Hispanic/other | 1.29 (.89–1.87) | .17 |
| HIV-specific characteristics | ||
| CD4 cell count at syphilis diagnosis, per 100-cell increase, cells/µL | 1.07 (1.01–1.12) | .02 |
| HIV RNA load at syphilis diagnosis, per log increase | 1.05 (.94–1.17) | .36 |
| Not on HAART at syphilis diagnosis | Ref | .18 |
| HAART use at syphilis diagnosis | 1.24 (.90–1.72) | |
| Syphilis treatment | ||
| 1 dose of BPG | Ref | .36 |
| ≥2 doses of BPG | 1.11 (.89–1.4) | |
| Other | 0.86 (.62–1.2) | |
| NTr titer <1:64 | Ref | <.001 |
| NTr titer of ≥1:64 | 1.94 (1.58–2.39) | |
| Factor . | Multivariate HR (95% CI) . | P Value . |
|---|---|---|
| Demographics | ||
| Age at syphilis diagnosis (for every 10 y increase) | 0.82 (.73–.93) | .001 |
| Ethnicity | ||
| White | 1.0 | |
| African American | 0.87 (.66–1.15) | .33 |
| Hispanic/other | 1.29 (.89–1.87) | .17 |
| HIV-specific characteristics | ||
| CD4 cell count at syphilis diagnosis, per 100-cell increase, cells/µL | 1.07 (1.01–1.12) | .02 |
| HIV RNA load at syphilis diagnosis, per log increase | 1.05 (.94–1.17) | .36 |
| Not on HAART at syphilis diagnosis | Ref | .18 |
| HAART use at syphilis diagnosis | 1.24 (.90–1.72) | |
| Syphilis treatment | ||
| 1 dose of BPG | Ref | .36 |
| ≥2 doses of BPG | 1.11 (.89–1.4) | |
| Other | 0.86 (.62–1.2) | |
| NTr titer <1:64 | Ref | <.001 |
| NTr titer of ≥1:64 | 1.94 (1.58–2.39) | |
The numbers in bold represent statistically significant differences or associations.
Abbreviations: BPG, benzathine penicillin G; CI, confidence interval; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; HR, hazard ratio; NTr, nontreponemal test; Ref, reference.
| Factor . | Multivariate HR (95% CI) . | P Value . |
|---|---|---|
| Demographics | ||
| Age at syphilis diagnosis (for every 10 y increase) | 0.82 (.73–.93) | .001 |
| Ethnicity | ||
| White | 1.0 | |
| African American | 0.87 (.66–1.15) | .33 |
| Hispanic/other | 1.29 (.89–1.87) | .17 |
| HIV-specific characteristics | ||
| CD4 cell count at syphilis diagnosis, per 100-cell increase, cells/µL | 1.07 (1.01–1.12) | .02 |
| HIV RNA load at syphilis diagnosis, per log increase | 1.05 (.94–1.17) | .36 |
| Not on HAART at syphilis diagnosis | Ref | .18 |
| HAART use at syphilis diagnosis | 1.24 (.90–1.72) | |
| Syphilis treatment | ||
| 1 dose of BPG | Ref | .36 |
| ≥2 doses of BPG | 1.11 (.89–1.4) | |
| Other | 0.86 (.62–1.2) | |
| NTr titer <1:64 | Ref | <.001 |
| NTr titer of ≥1:64 | 1.94 (1.58–2.39) | |
| Factor . | Multivariate HR (95% CI) . | P Value . |
|---|---|---|
| Demographics | ||
| Age at syphilis diagnosis (for every 10 y increase) | 0.82 (.73–.93) | .001 |
| Ethnicity | ||
| White | 1.0 | |
| African American | 0.87 (.66–1.15) | .33 |
| Hispanic/other | 1.29 (.89–1.87) | .17 |
| HIV-specific characteristics | ||
| CD4 cell count at syphilis diagnosis, per 100-cell increase, cells/µL | 1.07 (1.01–1.12) | .02 |
| HIV RNA load at syphilis diagnosis, per log increase | 1.05 (.94–1.17) | .36 |
| Not on HAART at syphilis diagnosis | Ref | .18 |
| HAART use at syphilis diagnosis | 1.24 (.90–1.72) | |
| Syphilis treatment | ||
| 1 dose of BPG | Ref | .36 |
| ≥2 doses of BPG | 1.11 (.89–1.4) | |
| Other | 0.86 (.62–1.2) | |
| NTr titer <1:64 | Ref | <.001 |
| NTr titer of ≥1:64 | 1.94 (1.58–2.39) | |
The numbers in bold represent statistically significant differences or associations.
Abbreviations: BPG, benzathine penicillin G; CI, confidence interval; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; HR, hazard ratio; NTr, nontreponemal test; Ref, reference.
The results of the different sensitivity analyses were similar; the dose and duration of BPG use did not alter response to treatment (Supplementary Data).
DISCUSSION
We examined treatment responses in 478 cases of early syphilis in HIV-infected persons, including 141 cases treated with a single dose of BPG. Following treatment, 91% of the included cases exhibited serologic response by 13 months and 97% by 2 years. A systematic review of the literature suggests that between 1% and 22% of HIV-infected subjects treated for early syphilis fail therapy [17]. Response rates observed in our study fall within this range and are identical to the rates observed in 2 recent studies [18, 19].
Furthermore, the results of our study suggest that the response to therapy does not vary by regimen type. We are aware of 4 other studies that have examined the effects of dose and duration of BPG treatment on treatment responses in HIV-infected persons with early syphilis [12, 18, 20, 21]. In a randomized double-blind trial, conducted in the pre-ART era, 541 subjects with early syphilis were randomized to receive standard treatment (ie, a single dose of 2.4 MU of BPG) or high-dose therapy (standard treatment followed by a 10 days of amoxicillin and probenecid) [12]. In this study, treatment responses were similar in both arms. Whereas these results form the basis of our current recommendation, only 19% of the enrolled subjects were HIV-infected, and losses to follow up were substantial (about 50% at 1 year), reducing the applicability of these results. In the HAART era, 3 studies have examined the question [18, 20, 21]. In 2 studies, the regimen type appeared not to matter [18, 20]. However, both studies included small numbers of subjects who received 1 dose of BPG as therapy and were likely underpowered to demonstrate small differences [18, 20]. In one study, 4 of 129 HIV-infected subjects received a single dose of BPG [20], whereas in the other study, 47 (8%) subjects were treated with a single dose of BPG [18]. In comparison, about a third of our cases (n = 141) received a single dose of BPG; this number exceeds the combined total reported in the 3 prior studies (n = 92). Hence, we believe this study represents a significant addition to the limited body of literature examining this issue.
Finally, unpublished data from a third prospective study suggest that individuals treated with 3 doses of BPG have a superior response to treatment [21]. However, when the analysis was restricted to subjects exhibiting an initial response (ie, a 4-fold decline in NTr titer), response to therapy did not vary by treatment regimen. In this study, subjects exhibiting a 4-fold decline in NTr titer followed by a 4-fold increase were considered treatment failures. Thus, misclassification of cases may have occurred with subjects been classified as nonresponders when they were in fact reinfected [21].
In our study, older age, lower CD4 count, and NTr titer <1:64 were associated with delayed responses. While contextualizing our results, it is important to consider distinguishing characteristics of our cohort. For one, HIV-infected persons with syphilis had fairly preserved immune function (median CD4 count was 494 cells/µL) and low viral loads at syphilis diagnosis (median viral load, 1.9 log10 copies/mL). In addition, HAART use was common at syphilis diagnosis (nearly two-thirds were on HAART). These HIV-related factors individually and in combination have been associated with superior responses to therapy [18, 19, 22–24]. The association with CD4 count observed in our study is worth noting, as about half the subjects had CD4 counts >500 cells/µL at syphilis diagnosis. This observation suggests that ongoing immune restoration in subjects with relatively high CD4 count is associated with superior response to therapy and advocates for the universal use of antiretroviral therapy. We did not observe a relationship with HAART use, perhaps because HAART use is common in the NHS (two-thirds reported HAART use at syphilis diagnosis). In sum, our results suggest that there would be little benefit to using additional doses of BPG for the treatment of early syphilis in HIV-infected persons with preserved CD4 counts and low viral loads; however, our study is not adequately powered to answer the question in individuals with advanced immunosuppression. Future studies should focus on this group of individuals.
Strengths of this analysis include the large sample size examined, and the close follow-up of our participants. Limitations of our study were common to other similar studies of this design. We excluded approximately 25% of the cases due to missing information. To account for the missing cases, we performed sensitivity analyses; these results suggest that the missing cases would not have altered our conclusions. In addition, our exclusion rate was significantly less than other studies, where it has ranged from 38% to 52% [12, 19, 24]. Our results nonetheless suggest that retention and follow-up remain a challenge even in a setting where individuals have free access to care. This was a retrospective study, and therefore could not be controlled for residual confounding, selection biases, or laboratory variations in NTr titers as the samples were not batched. Also, it is important to note that clinical symptoms are not captured in the NHS; hence, our definition excludes individuals with symptomatic relapses.
To examine the possibility that treatment assignment was nonrandom and influenced by the health status of the patient, we evaluated factors associated with treatment choices (data not shown). The choice of treatment was influenced only by the year a case was diagnosed (recent syphilis cases were more likely to be treated with 1 dose of BPG) and not by other demographic or HIV-related variables. Treatment recommendations have varied over the 28-year period of this study. Recent guidelines recommend a single dose of BPG for treating early syphilis, treatment choices in the NHS appear to pattern these recommendations, and a selection bias appears unlikely. Prospective studies designed to examine this question are needed. Finally, in the absence of behavioral data, distinguishing relapse from reinfection is complicated and is often based on expert consensus. Some experts have suggested that late increases in NTr titers (ie, those that occur >365 days after treatment for early syphilis) are suggestive of reinfection rather than relapse [22, 25]. In our study, among patients who had a rise in titer after a documented response, the median time period between these measurements was 1.7 years, thereby favoring reinfection as the most likely mechanism. Additionally, most subjects had an intervening documented negative NTr test between their cases, again favoring reinfection as the mechanism.
In conclusion, the results of our study support the use of a single dose of BPG for the treatment of early syphilis in HIV-infected persons with preserved CD4 counts. Overall, serologic failure is uncommon. When close follow-up can be ensured, HIV-infected persons with preserved CD4 counts and delayed NTr responses can be followed safely for a year and perhaps even 2 years without additional treatment courses.
Notes
IDCRP HIV/STI Working Group members. Susan Banks, Mary Bavaro, Cathy Decker, Lynn Eberly, Susan Fraser, Heather Hairston, Joshua Hartzell, Arthur Johnson, Grace Macalino, Scott Merritt, Robert O'Connell, Sheila Peel, Michael Polis, John Powers, Timothy Whitman, and Michael Zapor.
Acknowledgments. We thank the participants and their caregivers, without whom none of this work would be possible. We would also like to thank the research coordinators and support staff who have diligently worked on the Department of Defense HIV Natural History Study, as well as the members of the Infectious Disease Clinical Research Program HIV Working Group, listed above.
Author contributions. A. G. conceived the idea for this analysis. A. G., T. J. W., J. F. O., T. L., A. C. W., and B. K. A. implemented the study, collected data, and oversaw the individual participating sites. A. G. drafted the manuscript. O. M. performed the statistical analysis. R. G. D. and T. O. provided valuable input regarding the analyses. All authors provided critical reading that helped shape the manuscript.
We certify that all individuals who qualify as authors have been listed; each has participated in the conception and design of this work, the analysis of data (when applicable), the writing of the document, and the approval of the submission of this version.
Disclaimer. The views expressed are those of the author(s) and do not necessarily reflect the official views of the Uniformed Services University of the Health Sciences, nor the Department of Defense. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States government.” Title 17 U.S.C. 101 defines a United States government work as “a work prepared by a military service member or employee of the United States government as part of that person's official duties.”
Financial support. Support for this work (IDCRP-015) was provided by the Infectious Disease Clinical Research Program, a Department of Defense program executed through the Uniformed Services University of the Health Sciences. This project has been funded in whole, or in part, with federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health (interagency agreement Y1-AI-5072).
Potential conflicts of interest. All authors: No potential conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Author notes
Presented in part: IDWeek 2013, San Francisco, California, 2–6 October 2013. Abstract 1140.
IDCRP HIV/STI group members are listed in the Acknowledgments section.




