-
PDF
- Split View
-
Views
-
Cite
Cite
Jon Stone, Unfeignable biomarkers in functional neurological disorder: drifting back to Pierre Janet, Brain, Volume 143, Issue 2, February 2020, Pages 393–395, https://doi.org/10.1093/brain/awz420
Close - Share Icon Share
This scientific commentary refers to ‘Reduced drift rate: a biomarker of impaired information processing in functional movement disorders’, by Sadnicka et al. (doi: 10.1093/brain/awz387).
Any scholar digging around long enough in the history of functional neurological disorder (FND) and its older name, hysteria, will eventually find the work of Pierre Janet (1859–1947), neurologist and proto-psychologist. Many who do, tend to agree that Janet, more so than Freud and Charcot, has the most to offer the modern clinician and researcher in FND. What stands out in his work are the sheer number of patients, and the depth with which he studied them. As a consequence, his books, regardless of outmoded terminology, offer clinical guidance and scientific intuitions that still have relevance today (Janet, 1907). Janet gave us the concept of dissociation, which still persists to describe a kind of cognitive or mental deficit in which different functions of the brain, including ideas, sensation and actions, become abnormally separated from each other. Janet did not view dissociation as a form of psychological defence, more as a ‘decomposition’ of the ‘psychophysiological system’. For example, he noticed that the patient with functional visual loss would typically retain central vision, but lose peripheral vision, something routinely seen still in Goldmann charts showing spiralling or small central fields (Fig. 1). Peripheral vision must at some level still be occurring in the brain, but the quality and quantity of that experience are reduced.
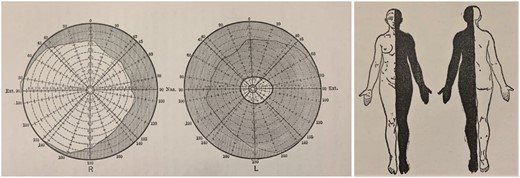
Contracted visual field and left hemianaesthesia. Extreme examples of reduced information processing in functional neurological disorder. From Janet (1907).
Janet highlighted the role of abnormal attentional focus in FND. This is most evident during the assessment for positive signs such as the tremor entrainment test or Hoover’s sign. A functional tremor improves when attention is diverted to the contralateral limb. In functional leg weakness, weak hip extension improves with attention diverted to contralateral hip flexion. But Janet was also interested in another aspect of attentional dysfunction of patients with FND separate from this. This was a general quality of ‘absent mindedness’ or ‘abstraction’, which he thought was common across patients with a variety of functional disorders:
‘While paying attention to something, we turn from some other thing and cease to interest ourselves in other phenomena, which however reach our minds. While I am paying attention to what I am reading, I abstract myself from the noises in the street, though I still perceive them. This abstraction exists in hysteria in an astonishing degree. It was noticed early that it presents itself in regard to the sensations and to ideas. In fact, it is not so, for absent-mindedness is not suggested to these patients and often is not even noticed. They have not the idea of this phenomenon, the importance of which they do not suspect.’ (Janet, 1907).
Here, Janet was suggesting that there may be a generalized deficit in attentional processing in patients with functional disorders, which might perhaps help to explain a range of potential symptoms, from numbness to weakness and the loss of peripheral vision.
Mechanistic neuropsychological hypotheses such as these had been around since the early 19th century. Brodie, Ross Reynolds and Paget all contributed important insights (Stone, 2016), but such concepts became superseded for most of the 20th century by psychoanalytic concepts, although vestiges remained, for example, the ‘hypnoid state’ of Breuer and Freud.
Whitlock (1967) and Ludwig (1972) agreed with Janet that paradoxically, FND was associated with a ‘selective depression of awareness of a bodily function’ and that such patients had a characteristic ‘subtle disturbance in cognitive functioning’. In the past 20 years more sophisticated models have emerged to try to explain the symptoms of FND. Those invoking the ‘Bayesian brain’ suggest that such symptoms are the inevitable consequence of an organ which works primarily by predicting sensation and action. Those predictions generally match up with reality, but if they become too strong, either because of excessive neural ‘top-down’ activity, or become less sensitive to normal visual and sensory ‘bottom-up’ feedback, then symptoms will arise (Edwards et al., 2012). This is a model of functional disorders not as an unexplained anomaly, but as disorders whose existence is a natural consequence of how the brain works.
In this issue of Brain, Sadnicka et al. (2020) explore these ideas in 36 patients with a functional movement disorder subtype of FND and 36 healthy controls using a temporal discrimination task. Participants had to decide whether one or two tactile stimuli were being applied to their index fingers, with varying interstimulus intervals for the trials with two stimulations. This task allows a measure of accuracy, and also reaction time. Sadnicka et al. found that patients with FND had slowed reaction times compared to controls and a higher threshold, on average, for being able to discriminate two stimuli from one. Accuracy was lower in the FND group, but importantly, accuracy had the same relationship to reaction time in both groups. The combination of accuracy and response allows some inference of the role of sensory processing compared to decision making in the outcome. At what point does the individual have sufficient information quality to decide that they can make an accurate response? In this study, ‘drift rate’ is a quantification of that process and it was systematically lower in the group with FND. There must be something about the internal processing of information in patients with FND that is amiss. The patients’ uncertainty persisted over a wider range of interstimulus intervals than in the healthy controls and it did not improve with practice or ease of task as you would typically expect. Although performance across the group with FND varied considerably, each individual with FND tended to show strong consistency in reaction time and accuracy across different levels of difficulty of the temporal discrimination task.
The authors conclude that the data suggest a problem in the quality of the sensory information that patients with FND have available to them to make decisions, rather than the decision making itself. This could relate to a problem in which excess ‘top-down’ attention elsewhere reduces capacity, or it could be that, because of strong predictions, ‘bottom-up’ information quality is poor.
Could the data simply be a consequence of comorbidity? Individuals with FND have higher rates of psychological comorbidity, physical symptoms and medication use than the healthy population. The effect in the current study remained after controlling for measures of anxiety and depression. Controlling for the other two factors is more difficult, but the observed effect did not depend upon disease duration, motor phenotype or disability, all of which suggest a more intrinsic psychophysiological quality.
Could it be that the subjects with FND were not trying hard enough? Perhaps they wanted to demonstrate consciously or otherwise to the assessors that they had trouble doing things? After all, if there was a disorder of voluntary movement and sensation, it would presumably look similar to individuals pretending to have the same problem. The difficulty of resolving issues of voluntariness is a major reason why neurologists in particular have been so reluctant to engage with this patient population over so many decades. Henry Miller, a neurologist in Newcastle, concluded that working out whether a symptom was consciously or unconsciously produced was ‘quite insusceptible to any form of scientific enquiry, and that it depends on nothing more infallible than one man’s assessment of what is probably going on in another man’s mind’ (Miller, 1961). The striking thing about the current data is how difficult they would be to feign. How would an individual be able to consciously or otherwise correlate their drift rate to the task difficulty? If someone did try to feign, we would expect them to do so equally for all levels of difficulty or to have higher false positive rates, neither of which occurred. It is hard enough for most of us to understand the data, let alone try and ‘break the bank’. In fact, when marshalled together there is now a range of data from a variety of sources that show that patients with FND, both as a group and individually, perform differently in certain tasks in a way that is arguably unfeignable. The same research group have previously published a study on sensory attenuation in Brain, featuring similar ‘dose response’ results in a task in which patients with FND were more accurate than controls, not less (Pareés et al., 2014). Consistencies of symptom experience and presentation across time, as revealed by the findings of Janet, and location, for example in Tanzania (Dekker et al., 2018), as well as differential improvement in randomized controlled trials, and differences in functional neuroimaging tasks between patients with FND and those feigning, all add strong weight to the same argument. Dismissing FND as voluntary or feigned symptoms can help clinicians feel better about a clinical problem they may feel ill-equipped to deal with, but it is no longer consistent with the data.
If not comorbidity or feigning, what is the explanation? Could it be that we have found Pierre Janet’s absent mindedness? Certainly, the data fit with a deficit of sensory processing, but they cannot tell us at what level this might be occurring. It is also not possible to separate out deficits related to an excess of abnormally focused attention elsewhere in the body from a generalized predisposition to reduced attention. Other smaller studies in FND have suggested impairment in the voluntary control of attention but with preserved automatic attention, rather like a form of sensory or attentional ‘Hoover’s sign’ (Roelofs et al., 2003; McIntosh et al., 2017)
It also seems unlikely that this finding is specific for FND as opposed to other functional disorders. Janet wrote about a wider range of functional disorders including fatigue, sleep disturbance and pain, which were experienced by patients with FND probably to a greater degree than comorbid anxiety or depression. In a review of cognitive deficits found in fibromyalgia and chronic fatigue syndrome, there were commonalities in relation to poor selective and divided attention, slow information processing and vulnerability to distraction (Teodoro et al., 2018).
We are still a long way from reliable biomarkers for FND. But studies like these and others investigating the neural basis of these symptoms have had the surprising side effect of highlighting the unfeignable nature of some of the differences found. Given the frequency of the clinical problem and the huge disability and distress associated with it, they provide further rationale for exploring the problem in the way that Pierre Janet did, from multiple perspectives and as a clinical brain disorder.
Competing interests
The author reports no competing interests.


