-
PDF
- Split View
-
Views
-
Cite
Cite
Jianglei Ma, Yifan Chang, Weidong Xu, Wanli Cao, Zongqin Zhang, Yihaoyun Lou, Duocai Li, Zifang Ma, Junhui Jiang, Shancheng Ren, Pelvic drain placement after robot-assisted radical prostatectomy: meta-analysis, BJS Open, Volume 7, Issue 6, December 2023, zrad143, https://doi.org/10.1093/bjsopen/zrad143
Close - Share Icon Share
Abstract
It is not clear whether the routine placement of a pelvic drain after robot-assisted radical prostatectomy is a necessity. The aim of this study was to investigate this through a meta-analysis of RCTs and non-randomized studies.
A search was performed in PubMed/MEDLINE, Embase, the Cochrane Library, and the Web of Science, up to 9 March 2023, for clinical trials comparing no drain with pelvic drain placement for patients with prostate cancer after robot-assisted radical prostatectomy. Two researchers independently conducted literature screening, data extraction, and quality assessment. A random-effect model was assumed for all analyses. The Cochrane Collaboration’s risk-of-bias tool was used to evaluate the methodological quality of RCTs and, for non-randomized studies, the ROBINS-I tool was used (where ROBINS-I stands for Risk Of Bias In Non-randomized Studies - of Interventions). This meta-analysis was prospectively registered in PROSPERO, the international prospective register of systematic reviews (CRD42023406429).
A total of six studies with 1480 patients were included in the meta-analysis. Both the meta-analysis of RCTs and the meta-analysis of non-randomized studies showed that patients without drains had a similar estimated blood loss (mean difference 40.49 ml, 95% c.i. −59.75 to 140.74 ml, P = 0.430, and mean difference −14.20 ml, 95% c.i. −32.26 to 3.87 ml, P = 0.120 respectively), overall complication rate (OR 0.60, 95% c.i. 0.35 to 1.04, P = 0.070, and OR 0.90, 95% c.i. 0.59 to 1.39, P = 0.640 respectively), Clavien–Dindo grade I–II complication rate (OR 0.62, 95% c.i. 0.34 to 1.13, P = 0.120, and OR 0.83, 95% c.i. 0.28 to 2.51, P = 0.750 respectively), Clavien–Dindo grade III–V complication rate (OR 0.60, 95% c.i. 0.10 to 3.69, P = 0.590, and OR 0.92, 95% c.i. 0.25 to 3.39, P = 0.900 respectively), and duration of hospital stay (mean difference −0.08 days, 95% c.i. −0.45 to 0.29 days, P = 0.670, and mean difference −0.64 days, 95% c.i. −2.67 to 1.39 days, P = 0.540 respectively) compared with routinely drained patients. Meta-analysis of non-randomized studies revealed that the duration of operation for patients without drains was shorter than that for patients with drains (mean difference −34.88 min, 95% c.i. −43.58 to –26.18 min, P < 0.001), but the meta-analysis of RCTs indicated that there was no significant difference between the two groups (mean difference −7.64 min, 95% c.i. −15.61 to 0.32 min, P = 0.060).
The intraoperative and postoperative outcomes of patients without drains were not inferior to those of patients with drains. In selected patients, pelvic drains can be omitted after robot-assisted radical prostatectomy.
Introduction
Radical prostatectomy (RP) is the standard surgical procedure for men with moderate-risk or high-risk prostate cancer1. From the initial open surgery to the current minimally invasive surgery, both surgical technology and the procedure have undergone significant development in the past 120 years1. Dating back to the introduction of robot-assisted RP (RARP) in 2000, RARP has generally become the dominant surgical approach for prostate cancer in the USA and most high-resource countries because it has inherent advantages to reduce unnecessary injuries, such as three-dimensional images and flexible robotic arms2–4.
Nevertheless, there is some uncertainty whether routine practices recommended by guidelines are necessary. One such practice is the routine placement of a pelvic drain (PD) after surgery to remove blood, lymph, urine, and other fluid. Although previous studies have revealed that patients undergoing RARP may not need the placement of drains, there is an absence of definitively confirmed evidence5–14. To the best of the authors’ knowledge, there is currently no meta-analysis on this topic that performs separate pooled analyses of RCTs and non-randomized studies. Therefore, the aim of this study was to provide systematic and comprehensive high-level evidence for clinical decision-making.
Methods
This meta-analysis was prospectively registered in PROSPERO, the international prospective register of systematic reviews (CRD42023406429), and was strictly performed in accordance with PRISMA guidelines15. Methodological evaluation using the AMSTAR 2 tool demonstrated a high-quality study (where AMSTAR stands for A MeaSurement Tool to Assess systematic Reviews)16.
Search strategy
PubMed/MEDLINE, Embase, the Cochrane Library, and the Web of Science were searched up to 9 March 2023. There was no restriction concerning article language. The search strategy is described in detail in the Supplementary Methods. The reference lists of potential articles were also checked to find other eligible articles.
Inclusion criteria and exclusion criteria
Two researchers individually screened the literature in accordance with the inclusion and exclusion criteria, and disputes were solved by discussion. The inclusion criteria were as follows: clinical trials comparing no drain (ND) with PD placement for patients with prostate cancer after RARP; full-text literature reporting at least one of the outcomes of interest; and if the studies reported by the same teams or institutions contained overlapping cases, the latest or largest studies were included. The earlier or smaller studies could be included to analyse the outcomes not reported by the latest or largest studies. If the reports from the same institutions included different cases, these studies were included. A study was excluded if it met one of the following criteria: case reports, reviews, meeting abstracts, editorials, comments, videos, guidelines, protocols, animal experiments, and other non-related studies; articles not yet published; and included patients who had any other malignant tumours and serious diseases, or had received surgery for benign prostatic hyperplasia, radiation of the pelvis, and androgen deprivation therapy for prostate cancer.
Data extraction
Two investigators independently extracted the data from all of the included studies and controversial results were settled by discussion. The following data were recorded: baseline characteristics (first author, publication year, country, study design, and sample size (ND group and PD group)); characteristics of participants (age, BMI, preoperative prostate-specific antigen, clinical tumour stage (cT), and D’Amico risk classification); intraoperative outcomes (duration of operation and estimated blood loss); and postoperative outcomes (overall complication rate (Clavien–Dindo grade I–V complications), Clavien–Dindo grade I–II and III–V complication rates, and duration of hospital stay).
Quality assessment of the included studies
Likewise, two investigators who were blinded from each other performed the assessment of the methodological quality of the included studies and handled the inconsistent results by discussion. The Cochrane Collaboration’s risk-of-bias tool was used to evaluate the methodological quality of RCTs; the tool covers seven elements (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias)17. Each element is rated as having a ‘low’, ‘high’, or ‘unclear’ risk of bias based on specific criteria. For non-randomized studies, the ROBINS-I tool18 was used (where ROBINS-I stands for Risk Of Bias In Non-randomized Studies - of Interventions). The tool consists of seven domains (bias due to confounding, bias in selection of participants into the study, bias in classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported result)18. Based on answers to the signalling questions, judgements for each bias domain and overall risk of bias can be ‘low’, ‘moderate’, ‘serious’, or ‘critical’ risk of bias.
Statistical analysis
Separate pooled analyses of the included RCTs and non-randomized studies19 were first performed. If the separate pooled results of RCTs and non-randomized studies were consistent, the two types of studies were synthesized for further analysis. Given the potential heterogeneity that existed among studies, a random-effect model was assumed for all analyses. Dichotomous variables were pooled using the Mantel–Haenszel method, with results given as OR and 95% confidence interval, and meta-analyses of continuous variables were conducted using the inverse-variance method, with results given as weighted mean difference (MD) and 95% confidence interval. If the mean and standard deviation for continuous variables were directly reported, they were used for meta-analysis. Otherwise, if the study provided the median, range, and interquartile range, the mean and standard deviation were calculated as described by Luo et al.20 and Wan et al.21 respectively. The I2 statistic was used to assess the heterogeneity. A value of 0% suggests no observed heterogeneity and larger values reveal increasing heterogeneity, with 25% indicating low heterogeneity, 50% indicating moderate heterogeneity, and 75% indicating high heterogeneity22. Publication bias was assessed by visually examining whether the funnel plot was symmetrical. When evidence suggesting publication bias was observed, the trim-and-fill method was used to adjust for funnel plot asymmetry and evaluate the impact of publication bias on the overall effect size, which can be considered as a sensitivity analysis method to verify whether the overall effect size is robust23. In addition, sensitivity analyses were performed by removing articles one by one to explore the robustness of the overall effect size. In forest plots, the results of analyses were reported with the random-effect model as the primary effect estimate. For all meta-analyses, sensitivity analyses were also conducted using the fixed-effect model. Two-sided P values <0.050 were considered statistically significant. All analyses were performed using Review Manager 5.4 (Cochrane Collaboration, Oxford, UK) and R with the ‘meta’ package.
Results
Selected studies and characteristics of studies
A total of six studies with 1480 patients, of which 672 patients were in the ND group and 808 patients were in the PD group, were included in the final meta-analysis9–14. Among the included studies, two were RCTs9,12 and four were non-randomized studies10,11,13,14. The language of five articles was English9,10,12–14 and the language of one article was Japanese11. There were four studies conducted in the USA10,12–14, there was one study conducted in Italy9, and there was one study conducted in Japan11. The detailed screening process of the literature is shown in Fig. 1. The basic characteristics of RCTs and non-randomized studies are shown in Table S1.
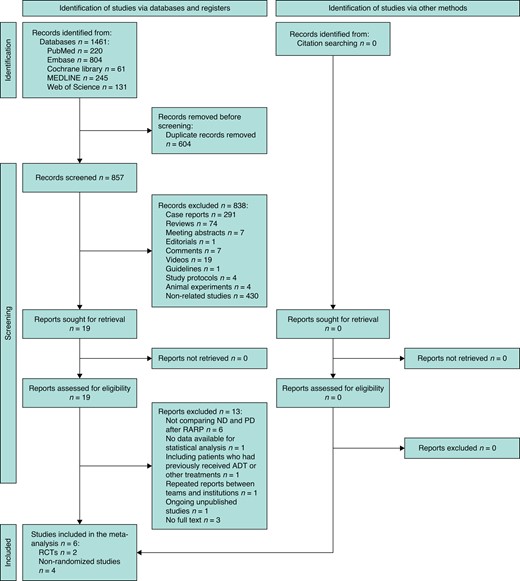
PRISMA flow chart showing selection of articles for review
ND, no drain; PD, pelvic drain; RARP, robot-assisted radical prostatectomy; ADT, androgen deprivation therapy.
Quality assessment of the included studies
Each domain of the two RCTs was judged as having a low risk of bias (shown in Fig. S1 and Fig. 2). For the four non-randomized studies, the overall risk of bias of two studies was low, whereas that of the remaining two studies was moderate. Detailed domain-level bias assessment results of non-randomized studies are shown in Table S2.
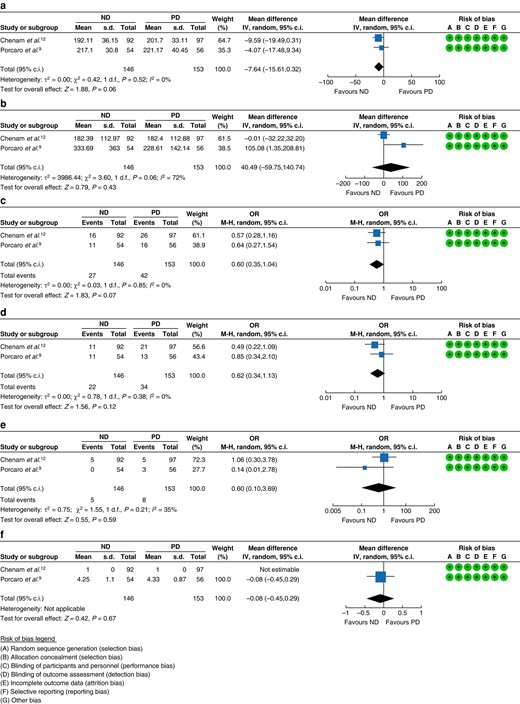
Forest plot of meta-analysis of RCTs
a Duration of operation. b Estimated blood loss. c Overall complication rate. d Clavien–Dindo grade I–II complication rate. e Clavien–Dindo grade III–V complication rate. f Duration of hospital stay. ND, no drain; PD, pelvic drain; IV, inverse-variance method; MH, Mantel–Haenszel method.
Meta-analysis of RCTs
No statistical difference was found between the ND group and the PD group in terms of duration of operation (MD −7.64 min, 95% c.i. −15.61 to 0.32 min, P = 0.060, I2 = 0%) (Fig. 2a) and estimated blood loss (MD 40.49 ml, 95% c.i. −59.75 to 140.74 ml, P = 0.430, I2 = 72%) (Fig. 2b). The results of the meta-analysis of the two RCTs showed no statistical difference between the two groups in the incidences of overall complications (OR 0.60, 95% c.i. 0.35 to 1.04, P = 0.070) (Fig. 2c) and Clavien–Dindo grade I–II complications (OR 0.62, 95% c.i. 0.34 to 1.13, P = 0.120) (Fig. 2d), with no heterogeneity (I2 = 0%). Concerning the incidence of Clavien–Dindo grade III–V complications, no statistically significant difference was observed between the two groups (OR 0.60, 95% c.i. 0.10 to 3.69, P = 0.590), but there was moderate heterogeneity (I2 = 35%) (Fig. 2e). Additionally, it was not possible to demonstrate a difference in the duration of hospital stay between patients who received PDs and those who did not (MD −0.08 days, 95% c.i. −0.45 to 0.29 days, P = 0.670) (Fig. 2f).
Meta-analysis of non-randomized studies
The pooled results of two studies showed that patients without drains had a shorter duration of operation (MD −34.88 min, 95% c.i. −43.58 to −26.18 min, P < 0.001) (Fig. 3a) and a similar estimated blood loss (MD −14.20 ml, 95% c.i. −32.26 to 3.87 ml, P = 0.120) (Fig. 3b) compared with those with drains, with no heterogeneity (I2 = 0%). The results of a pooled analysis of the four non-randomized studies revealed that the overall complication rates of the two groups were similar (OR 0.90, 95% c.i. 0.59 to 1.39, P = 0.640) and that there was low heterogeneity (I2 = 9%) (Fig. 3c). Meta-analysis of three studies indicated that the incidence of Clavien–Dindo grade I–II complications in the ND group was not statistically different from that in the PD group (OR 0.83, 95% c.i. 0.28 to 2.51, P = 0.750), but there was moderate heterogeneity (I2 = 67%) (Fig. 3d). Similarly, no statistically significant difference existed between the two groups in terms of the incidence of Clavien–Dindo grade III–V complications (OR 0.92, 95% c.i. 0.25 to 3.39, P = 0.900), with moderate heterogeneity (I2 = 66%) (Fig. 3e). The duration of hospital stay of patients in the ND group was similar to that of patients in the PD group (MD −0.64 days, 95% c.i. −2.67 to 1.39 days, P = 0.540) (Fig. 3f).
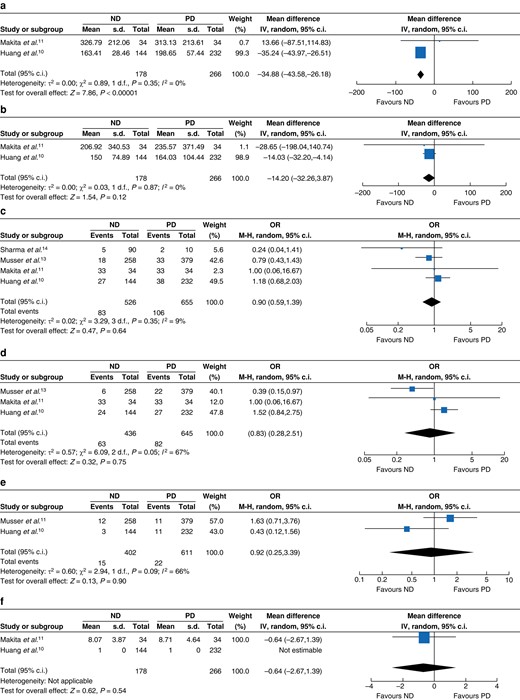
Forest plot of meta-analysis of non-randomized studies
a Duration of operation. b Estimated blood loss. c Overall complication rate. d Clavien–Dindo grade I–II complication rate. e Clavien–Dindo grade III–V complication rate. f Duration of hospital stay. ND, no drain; PD, pelvic drain; IV, inverse-variance method; MH, Mantel–Haenszel method.
Meta-analysis of synthesized RCTs and non-randomized studies
The results of the meta-analysis of synthesized RCTs and non-randomized studies exhibited that there was still no statistically significant difference between the ND and PD groups in terms of estimated blood loss (MD −0.49 ml, 95% c.i. −30.38 to 29.39 ml, P = 0.970, I2 = 43%) (Fig. 4a), overall complication rate (OR 0.80, 95% c.i. 0.58 to 1.09, P = 0.160, I2 = 0%) (Fig. 4b), Clavien–Dindo grade I–II complication rate (OR 0.75, 95% c.i. 0.41 to 1.37, P = 0.350, I2 = 52%) (Fig. 4c), Clavien–Dindo grade III–V complication rate (OR 0.87, 95% c.i. 0.38 to 1.99, P = 0.740, I2 = 37%) (Fig. 4d), and duration of hospital stay (MD −0.10 days, 95% c.i. −0.46 to 0.27 days, P = 0.600, I2 = 0%) (Fig. 4e).
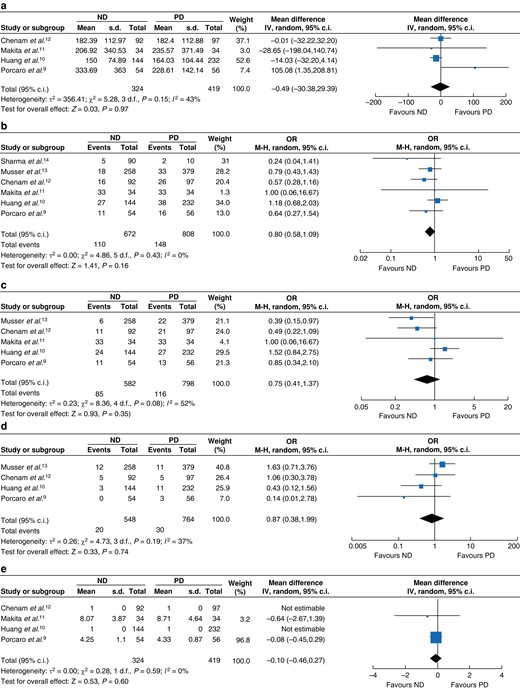
Forest plot of meta-analysis of synthesized RCTs and non-randomized studies
a Estimated blood loss. b Overall complication rate. c Clavien–Dindo grade I–II complication rate. d Clavien–Dindo grade III–V complication rate. e Duration of hospital stay. ND, no drain; PD, pelvic drain; IV, inverse-variance method; MH, Mantel–Haenszel method.
Publication bias
Asymmetrical funnel plots revealed that there was potential publication bias; however, trim-and-fill analyses indicated that potential publication bias did not have a significant impact on the overall effect sizes (Fig. S2). Furthermore, the overall effect sizes adjusted by the trim-and-fill method were consistent with the unadjusted overall effect sizes (Fig. S3).
Sensitivity analysis
Sensitivity analyses showed that the statistical results of each outcome using the fixed-effect model were consistent with those of the previous pooled analyses using the random-effect model (Figs S4–S6). When sensitivity analyses were performed by removing articles one by one, the results indicated that the patients in the ND group had a similar duration of operation and lower incidences of overall complications and Clavien–Dindo grade I–II complications compared with those in the PD group after the study by Huang et al.10 was removed (Fig. S7). However, the statistical results were unchanged when the remaining studies were individually removed. Sensitivity analyses of the remaining outcomes through omitting studies one by one showed that the statistical results were also unchanged (Figs S8–S10). Altogether, no evidence that supported the advantages of routine PD placement over ND placement was observed.
Discussion
The present study shows that the intraoperative and postoperative outcomes of ND patients are not inferior to those of PD patients. In properly selected patients, the placement of a PD after RARP can be safely omitted without significant additional morbidity.
Prophylactic PD placement has been deemed a necessary procedure since the introduction of RP24. More recently, the degree of trauma caused by RP has decreased significantly with the development of the robotic surgery system, but it is still recommended that a surgical drain needs to be placed in the pelvic cavity after RARP and removed early25. However, this routine practice may be associated with additional morbidity, such as pain and infection at the drain site, injury to the inferior epigastric vessels, and abdominal wall haematomas12. A previously published study also indicated that 24% of postoperative pain was attributed to the drain site26. Therefore, high-level evidence was required on whether a drain is indispensable after RARP.
Due to differences in design principles, research objectives, and study subjects between RCTs and non-randomized studies, synthesizing the two types of studies directly to conduct a meta-analysis may exaggerate or undermine the effectiveness of a particular intervention19. An appropriate method is to first conduct a separate quantitative synthesis of RCTs and non-randomized studies, and, if the results of the two analyses are consistent, then synthesize the two types of studies for further analysis. According to the present analyses, both the meta-analysis results of RCTs and those of non-randomized studies showed that the estimated blood loss, the incidences of overall, Clavien–Dindo grade I–II, and Clavien–Dindo grade III–V complications, and the duration of hospital stay were similar in men who underwent RARP, regardless of whether the pelvis was drained, findings consistent with the growing evidence against the routine placement of a PD9,12,27–29. After synthesizing RCTs and non-randomized studies, the meta-analysis results also demonstrated that the above outcomes were similar between the ND and PD groups, further suggesting that the placement of drains after RARP may be unnecessary. Moreover, considering the increased concern about healthcare costs, the elimination of prophylactic surgical drain placement may possess underlying economic benefits, especially in situations without a clinical indication30–32.
Interestingly, when all of the included studies, except the study by Huang et al.10, were pooled to conduct a sensitivity analysis, the incidence of overall complications in the ND group was lower than that in the PD group, a phenomenon that also occurred in the sensitivity analysis of the incidence of Clavien–Dindo grade I–II complications. The possible explanation is that the study by Huang et al.10 accounts for the largest weight in the overall effect sizes and its individual OR values are greater than 1. After it is excluded, the individual OR values of the remaining studies are either less than or equal to 1, and thus the statistical results have undergone the above changes. Moreover, sensitivity analyses of non-randomized studies showed that, after the study by Huang et al.10 was omitted, there was no significant difference regarding the duration of operation between the ND and PD groups. One of the reasons is that Huang et al.10 performed a lower percentage of lymphadenectomy in the ND arm, which potentially resulted in a shorter duration of operation in the ND arm than in the PD arm. Therefore, after the study by Huang et al.10 was excluded, the remaining studies reported no significant difference regarding the duration of operation between the two groups. Notwithstanding, the results obtained through sensitivity analyses using other methods showed that the overall effect sizes did not change, suggesting that the results were sound. Regardless, the present study could at least demonstrate that the omission of drains did not cause additional adverse intraoperative and postoperative outcomes.
Notably, although the results of this present study revealed that the omission of a PD after RARP did not induce additional complications and could reduce the postoperative pain of patients, PD placement should not be viewed as an unnecessary procedure for all cases. The placement of surgical drains might still be beneficial for certain patients, including those who receive perioperative prophylactic low-molecular-weight heparin, undergo complex bladder neck reconstruction, undergo extended pelvic lymph node dissection, or are at higher risk of anastomotic leak2,12. Therefore, the decision to place a PD should be made on a case-by-case basis, taking into account the potential risks and benefits for each patient.
The major strength of the present study is the execution of the separate pooled analyses of RCTs and non-randomized studies, minimizing the impact of methodological heterogeneity of each study to achieve a more precise and convincing conclusion. The present study also has several limitations. First, although a comprehensive literature search was performed, it is possible that relevant articles were missed. Second, potential publication bias is observed. However, trim-and-fill analyses indicate that potential publication bias did not have a significant impact on the overall effect sizes. Additionally, the overall effect sizes adjusted by the trim-and-fill method are consistent with the unadjusted overall effect sizes, which suggests that the results of the present study are robust. Finally, the number of RCTs is small, so any conclusions resulting from the analysis of RCTs require caution.
Funding
Supported by grants from the National Natural Science Foundation of China (82125025 to S.R.), the Shanghai Shen kang Hospital Development Centre (SHDC12022117 to S.R. and SHDC2022CRT005 to S.R.), and the Shanghai Municipal Education Commission (2023ZKZD46 to S.R.).
Acknowledgements
J.M., Y.C., and W.X. contributed equally to this study.
Author contributions
Jianglei Ma (Data curation, Formal analysis, Methodology, Software, Visualization, Writing—original draft, Writing—review & editing), Yifan Chang (Data curation, Formal analysis, Software, Visualization, Writing—review & editing), Weidong Xu (Data curation, Formal analysis, Software, Visualization, Writing—review & editing), Wanli Cao (Software, Visualization, Writing—review & editing), Zongqin Zhang (Software, Visualization, Writing—review & editing), Yihaoyun Lou (Writing—review & editing), Duocai Li (Writing—review & editing), Zifang Ma (Methodology, Supervision, Writing—review & editing), Junhui Jiang (Methodology, Supervision, Writing—review & editing), and Shancheng Ren (Conceptualization, Methodology, Supervision, Writing—review & editing)
Disclosure
The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.



