-
PDF
- Split View
-
Views
-
Cite
Cite
Taiga Oka, Hideki Ishimaru, Maki Hirao, Hiroki Nagayama, Shuto Miyamura, Chika Somagawa, Takashi Nonaka, Takuya Honda, Ryo Toya, A case of chylous ascites caused by reflux from the cisterna chyli to the disrupted common iliac lymphatic vessel: fluoroscopic records during intranodal lymphangiography, BJR|Case Reports, Volume 10, Issue 1, January 2024, uaae004, https://doi.org/10.1093/bjrcr/uaae004
Close - Share Icon Share
Abstract
A 40-year-old woman underwent laparoscopic common iliac lymphadenectomy for metastasis from rectal cancer. Two weeks after the surgery, she was found to have massive chylous ascites. After failure of conservative treatment, bilateral inguinal intranodal lymphangiography was performed. No definite extravasation was observed while lipiodol injected through the left inguinal node was ascending. When we punctured the right inguinal lymph nodes and started the injection of lipiodol, extravasation of diluted lipiodol was noted at the level of the first sacrum. Careful observation revealed that the ascending lipiodol became diluted in the cisterna chyli, refluxed through the median paraaortic route, leaked from the excised left common iliac lymph vessel, and flowed into the abdominal cavity. Lipiodol used in lymphangiography did not reduce chylous ascites at all. Twenty-seven days after lymphangiography, laparoscopic lymphatic ligation was performed, and the chylous ascites disappeared completely. CT obtained 40 days after surgical repair revealed disappearance of ascites and enlargement of the thoracic duct, which had not been observed on preoperative lymphangiography. Notably, lymphatic reflux from the cisterna chili can occur without obstruction of the thoracic duct and may result in chylous ascites.
Introduction
Chylous ascites is defined as a milky peritoneal fluid rich in triglycerides.1,2 It usually occurs in cases of lymphatic system disruption as a result of traumatic injury or obstruction.2 Postoperative chylous ascites is not frequent3 but is caused by direct surgical trauma to major lymphatic tributaries.4
Lipiodol lymphangiography is a method for diagnosing chylous leakage and enables the identification of the leakage points for surgical intervention.5–7 However, lymphangiography from the legs often cannot reveal the source of chylous ascites leakage. This is because the intestinal lymphatic ducts that carry chyle and connect to the lumbar lymphatic ducts or cisterna chyli are often outside the path of the contrast agent injected from the legs.7 We herein describe the case of a patient who, after common iliac lymphadenectomy, developed severe chylous ascites involving a mechanism that was revealed by inguinal intranodal lipiodol lymphangiography.
Case report
A 40-year-old woman who underwent laparoscopic rectectomy and pelvic lymph node dissection for rectal cancer and lymph node metastases 1 year earlier was found to have common iliac node metastasis on CT. She underwent an additional lymphadenectomy without any immediate complications. Approximately 2 weeks after the second surgery, she presented with abdominal distension and tenderness, and a CT scan showed massive ascites. Abdominal paracentesis drained a milky-white fluid, which was found to have elevated triglyceride levels (855 mg/dL) and was diagnosed as chylous ascites. After admission, administration of somatostatin analogue (octreotide) and total parenteral nutrition were performed. Abdominal distension continued, and the daily drainage volume continued to exceed 1 L. Conservative treatment was deemed difficult. Intranodal lymphangiography was performed for the purpose of diagnosing and treating chyle leakage.
After ultrasound-guided puncture of the left inguinal lymph nodes with a 23G needle, lipiodol was slowly injected. Fluoroscopy obtained 10 min after initiating injection of the contrast agent showed progression of the lipiodol through the left iliac and lumbar lymphatic ducts; however, extravasation was not observed (Figure 1A). When we punctured the right inguinal lymph node 25 min after the initial injection of lipiodol at the left inguinal node, an extravasation of diluted lipiodol was noted at the level of the first sacrum (Figure 1B). Fluoroscopy obtained 85 min after the start of left inguinal injection showed diluted lipiodol descending the anterior aspect of the lumbar spine and extravasating at the level of the first sacrum, which corresponded to the resected common iliac lymph node metastasis (Figure 1C and Supplementary Movie). Careful observation revealed that the lumbar lymphatic ducts flowed into the cisterna chyli, but the thoracic duct was not observed. Lipiodol was diluted considerably in the cisterna chyli and descended in a pulsatile fashion (Figure 1C and Supplementary Movie).
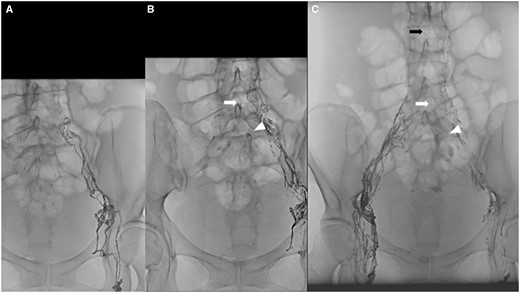
(A) Fluoroscopic images obtained 10 min after initiating injection of the contrast agent show progression of the lipiodol through the left iliac and lumbar lymphatic ducts; however, there is no definite extravasation. (B) Fluoroscopic image obtained 25 min after the initial injection of lipiodol through the left inguinal node. Extravasation of diluted lipiodol is noticeable at the level of the first sacrum (arrowhead). A linear opacity in the midline corresponding to descending lipiodol flow was also found (white arrow). (C) Fluoroscopic image obtained 85 min after the initial injection of lipiodol shows diluted lipiodol reflux from the cisterna chyli (black arrow), descent of the anterior aspect of the lumbar spine (white arrow), and extravasation at the level of the first sacrum (arrowhead).
CT obtained 135 min after the start of left inguinal injection revealed contrast extravasation at the ventral surface of the sacrum (Figure 2). From these images, we concluded that chyle entered the cisterna chyli, refluxed via the median paraaortic route, leaked from the excised left common iliac lymph vessel, and flowed into the abdominal cavity. Since the area of surgical lymphadenectomy corresponded to the area of leakage, it was strongly suspected that this chyle leakage resulted from surgical disruption of the left common iliac lymph vessels. Lipiodol used in lymphangiography was expected to exert an embolizing effect and reduce chylous ascites,5 but it did not reduce chylous ascites at all. Twenty-seven days after lymphangiography, laparoscopic lymphatic ligation was performed. After surgery, the chylous ascites disappeared completely. CT obtained 40 days after surgical repair revealed disappearance of ascites and enlargement of the thoracic duct (Figure 3).
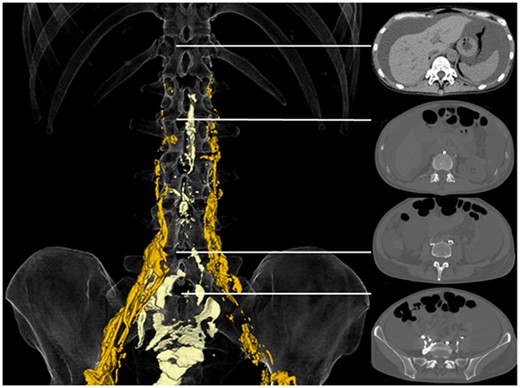
Three-dimensional volume rendering (left) shows anterograde lipiodol (yellow) and descending and refluxing lipiodol (light yellow). Cross-sectional CT images at several levels (right) show that the midline descending lipiodol corresponds to retroperitoneal paraaortic lymphatic vessels. The top image shows that lipiodol does not flow into the thoracic duct at all. The second image from the top shows the level of the cisterna chyli.

CT obtained 40 days after surgical repair shows no ascites and an enlarged thoracic duct (arrow).
Discussion
Chylous lymphatic fluid formed in the small bowel progress through the mesenteric lymphatic system to join the cisterna chyli via its intestinal trunk.8 If abdominal paracentesis shows a milky or creamy appearance, the possibility of chyle leakage should be considered. Persistent chylous leakage tends to increase morbidity because it contains higher concentrations of nutrients, and the amount of leakage is usually more excessive than that associated with nonchylous leakage. Many surgical series have shown to increase morbidity, lower survival, and prolong hospital stays in patients with chylous ascites.7
Chylous leakage is highly suggestive of damage to the mesenteric lymphatic system, the intestinal trunk, the cisterna chyli, the thoracic duct, or the retroperitoneal lymphatic network close to the aforementioned structures.8 Whether chylous leakage manifests as a retroperitoneal chylous lymphocele, chylous ascites, or chylothorax depends on the location and extent of the lymphatic injury and the integrity of the adjacent retroperitoneal structures.8
Intranodal lymphangiography can provide useful information for the treatment of lymphorrhea.9 However, the source of the leakage in chylous ascites is often not demonstrable by lymphangiography. Anatomically, intestinal lymphatic ducts that carry chyle to join lumbar lymphatic ducts or cisterna chyli are often outside the pathway of the contrast that is injected in the lower extremities.7 The intestinal trunk and its upstream mesenteric lymphatic system are rarely visualized in any lymphatic examination because contrast medium injected through inguinal or retroperitoneal lymph nodes usually does not oppose the flow direction of the chylous lymphatics.8
In the present case, however, lymphography confirmed retrograde flow of lymph from the cisterna chyli and the source of the leak. Lipiodol was observed to ascend the bilateral lumbar lymphatics, mix with chyle from the intestinal lymphatics at the cisterna chyli, become diluted, retrogradely descend the retroperitoneal lymphatics, and leak from the common iliac lymphatics into the peritoneal cavity. To our knowledge, this is the first report including fluoroscopic video recording of retrograde flow from the cisterna chyli for a height of two or more vertebral bodies and chyle leakage into the abdominal cavity.
The extravasation site was 7 cm below the cisterna chyli, and percutaneous embolization following catheterization through the cisterna chyli was not considered possible. Because the area of leakage corresponded to the area of surgical lymphadenectomy, surgical repair was performed, and chyle leakage was stopped.
Yamagami et al reported chylous ascites caused by leakage from the common iliac lymphatics.5 In that case, lymphangiography confirmed leakage originating from the lymph vessel running in the left common iliac lymph vessel, but lipiodol did not ascend beyond the level of the fifth lumbar vertebra. We speculate that retrograde flow of lymph from the cisterna chyli into the iliac lymphatics may have caused chylous ascites in that case. They also reported that lymphangiography alone stopped chyle leakage.5 They hypothesized that lipiodol accumulation at the point of leakage outside the lymphatic vessel caused a regional inflammatory reaction adjacent to the area of lipiodol retention, and the point of leakage of the lymphatic vessel was obstructed. In the present case, it is possible that regional inflammation was insufficient to occlude the lymphatic vessels, as lipiodol accumulated at the point of leakage was so diluted by chyle.
Hur et al reported an overall clinical success rate of 85% using lipiodol lymphangiography combined with lymphopseudoaneurysm embolization, closest upstream lymph node embolization, or direct upstream lymphatic vessel embolization in a group of patients with chylous ascites, lymphocele, or chylothorax.6 They also stated that glue embolization of one or two lymph nodes using n-butyl cyanoacrylate diluted up to 1:9 did not cause clinically significant lymphedema. In the present case, we could try injecting ultradiluted glue through the inguinal lymph nodes prior to surgical repair. However, we did not try this because it was concerned that the glue might polymerize before it reaches the leakage point via the lumbar lymphatic vessels and cisterna chyli. This approach is considered to work when intestinal lymphatic ducts are connected to the retroperitoneal lymphatics below the chyle leakage point.7
Dynamic contrast-enhanced magnetic resonance lymphangiography is a technique with high spatial resolution technique that does not involve the use of ionizing radiation and is increasingly used for evaluating lymphatic disease evaluation and preoperatively planning.10 This method could have delineated the lymphatic reflux from the cisterna chyli.
Because the thoracic duct was not seen on intranodal lymphangiography in the case we presented, we assumed that chylous reflux into the retroperitoneal lymphatics might be due to obstruction of the thoracic duct. However, CT after surgical repair revealed an enlargement of the thoracic duct diameter, suggesting that the anterograde flow of the thoracic duct had been restored. We believe that lipiodol did not flow into the thoracic duct because the pressure of fluid leaking from the ruptured lymphatic vessel was much lower than that of fluid in the thoracic duct.
Conclusion
We presented a case of refractory chylous ascites after common iliac lymphadenectomy in which lymphography confirmed retrograde flow of lymph from the cisterna chyli and leakage. Notably, lymphatic injury after retroperitoneal lymphadenectomy may result in chylous ascites due to lymphatic reflux from the cisterna chili.
Learning points
Postoperative chylous ascites is not a frequent but an important clinical issue.
Lymphatic injury after retroperitoneal lymphadenectomy may result in chylous ascites due to lymphatic reflux from the cisterna chili.
Inguinal intranodal lymphangiography from the legs may demonstrate the source of the leak in chylous ascites
Supplementary material
Supplementary material is available at BJR|Case Reports online.
Funding
None declared.
Conflicts of interest
None declared.
Consent for publication
Written informed consent from the patient for the publication of this case report, including the history and accompanying images is taken.



