-
PDF
- Split View
-
Views
-
Cite
Cite
Ruth Barbour, Papari Deka, Paediatric anaesthesia for low-resource settings, BJA Education, Volume 17, Issue 11, November 2017, Pages 351–356, https://doi.org/10.1093/bjaed/mkx030
Close - Share Icon Share
Key points
An anaesthetist working in a low-resource setting will encounter many paediatric patients within their practice.
The wide range of equipment sizes needed to provide safe, high-quality anaesthesia to children is often absent or lacking.
Thorough preoperative assessment and planning are vital to optimize patient care and decide whether local resources are sufficient for surgery to proceed safely.
Intraoperative temperature and blood glucose control are challenging because of a lack of active warming and monitoring devices.
Postoperative analgesia is a challenge and the use of local or regional anaesthetic techniques where appropriate and safe to do so is strongly recommended.
Core surgical indicators and targets as outlined by the Lancet Commission on Global Surgery to be achieved by 2030
| Indicator name . | Target . |
|---|---|
| Access to timely essential surgery | A minimum of 80% coverage of essential surgical and anaesthesia services per country by 2030 |
| Specialist surgical workforce density | 100% of countries with at least 20 surgical, anaesthesia and obstetric physicians per 100 000 population by 2030 |
| Surgical volume | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; 5000 procedures per 100 000 population by 2030 |
| Perioperative mortality rate (POMR) | 80% of countries by 2020 and 100% of countries by 2030 tracking perioperative mortality rate (POMR); in 2020, assess global data and set national targets for 2030 |
| Protection against impoverishing expenditure | 100% protection against impoverishment for out-of-pocket (OOP) payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | 100% protection against catastrophic expenditure from OOP payments for surgical and anaesthesia care by 2030 |
| Indicator name . | Target . |
|---|---|
| Access to timely essential surgery | A minimum of 80% coverage of essential surgical and anaesthesia services per country by 2030 |
| Specialist surgical workforce density | 100% of countries with at least 20 surgical, anaesthesia and obstetric physicians per 100 000 population by 2030 |
| Surgical volume | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; 5000 procedures per 100 000 population by 2030 |
| Perioperative mortality rate (POMR) | 80% of countries by 2020 and 100% of countries by 2030 tracking perioperative mortality rate (POMR); in 2020, assess global data and set national targets for 2030 |
| Protection against impoverishing expenditure | 100% protection against impoverishment for out-of-pocket (OOP) payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | 100% protection against catastrophic expenditure from OOP payments for surgical and anaesthesia care by 2030 |
Core surgical indicators and targets as outlined by the Lancet Commission on Global Surgery to be achieved by 2030
| Indicator name . | Target . |
|---|---|
| Access to timely essential surgery | A minimum of 80% coverage of essential surgical and anaesthesia services per country by 2030 |
| Specialist surgical workforce density | 100% of countries with at least 20 surgical, anaesthesia and obstetric physicians per 100 000 population by 2030 |
| Surgical volume | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; 5000 procedures per 100 000 population by 2030 |
| Perioperative mortality rate (POMR) | 80% of countries by 2020 and 100% of countries by 2030 tracking perioperative mortality rate (POMR); in 2020, assess global data and set national targets for 2030 |
| Protection against impoverishing expenditure | 100% protection against impoverishment for out-of-pocket (OOP) payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | 100% protection against catastrophic expenditure from OOP payments for surgical and anaesthesia care by 2030 |
| Indicator name . | Target . |
|---|---|
| Access to timely essential surgery | A minimum of 80% coverage of essential surgical and anaesthesia services per country by 2030 |
| Specialist surgical workforce density | 100% of countries with at least 20 surgical, anaesthesia and obstetric physicians per 100 000 population by 2030 |
| Surgical volume | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; 5000 procedures per 100 000 population by 2030 |
| Perioperative mortality rate (POMR) | 80% of countries by 2020 and 100% of countries by 2030 tracking perioperative mortality rate (POMR); in 2020, assess global data and set national targets for 2030 |
| Protection against impoverishing expenditure | 100% protection against impoverishment for out-of-pocket (OOP) payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | 100% protection against catastrophic expenditure from OOP payments for surgical and anaesthesia care by 2030 |
High-quality perioperative care and outcomes are inextricably linked to the provision of safe anaesthesia, and thus anaesthetists have an important role to play in the improvement of surgical services in low- and middle-income countries (LMICs).4 To this end, an anaesthetist may choose to spend a period of time working and delivering training in an LMIC, where he or she will undoubtedly be presented with the challenge of anaesthetizing a child in the context of limited resources. In most sub-Saharan African countries, over 40% of the population is aged 0–14 years,5 and it has been estimated that 85% of children in low-income countries are likely to require treatment for a surgical condition by the time they reach the age of 15 years.6
Perioperative paediatric mortality in LMICs
Precise figures for global paediatric mortality related to anaesthesia are difficult to obtain because of a paucity of data and a lack of consensus in the literature regarding the definition of anaesthesia-related mortality.7 However, it is well described that the rates of perioperative mortality and adverse perioperative respiratory events in children are highest among neonates and infants and additional risk factors for perioperative paediatric mortality include complex congenital heart disease, an American Association of Anaesthesia (ASA) status greater than three, emergency surgery, and general vs neuraxial anaesthesia.7–9
Data collected from individual LMICs imply that perioperative mortality in these countries remains unacceptably high.10 A recent multicentre, international, prospective, cohort study identified that paediatric-adjusted mortality after emergency abdominal surgery in LMICs may be as great as seven times that of high-income countries.11 Older studies report similarly high mortality rates. A cross-sectional survey of 29 hospitals in Uganda in 2008 that performed major surgery in children revealed an overall in-theatre mortality of 7.7 deaths per 10 000 cases.12 Between 1996 and 2004, a Brazilian tertiary teaching hospital reported rates of perioperative cardiac arrest in children of 22.9:10 000 with 4.58 being attributable to anaesthesia (2.62 totally and 1.96 partially).9 In 2007, the two main university hospitals in Benin reported an incidence of perioperative cardiac arrest of 156:10 000.7
Although the perioperative mortality rate solely attributable to anaesthesia has declined in all age groups over the past 50 years, this predominantly applies to high-income countries.13 The data described above indicate the need for urgent improvement in the quality and effective delivery of essential emergency and elective surgery to children in LMICs. Factors identified in the literature as contributing to high perioperative morbidity and mortality rates include a paucity of trained anaesthesia providers (particularly physician anaesthetists), staff working in isolation without medical supervision, equipment problems, system factors, and patient factors.10 Lack of adequately trained personnel is a huge problem, and a survey conducted among anaesthesia providers in Uganda in 2006 showed that only 13% were thought to be able to provide safe anaesthesia to children under the age of 5 years on the basis of training and available resources.14
Challenges to paediatric anaesthesia in resource poor settings
Practising a technology-based specialty in an environment where facilities are limited requires flexibility and an adaptive approach. The spectrum of problems encountered is vast and can be divided into patient factors, equipment factors, local system factors, and wider infrastructural factors. It should be recognized, however, that huge variety in available resources exists between and within different LMICs and that the conditions described in the following may not always apply.
Patient factors
Pathologies that present for surgery are numerous and include congenital defects, infection, common paediatric surgical emergencies, and the consequences of trauma such as road traffic accidents, burns, armed conflict, or natural disasters. Patients will often have travelled long distances to reach hospital and commonly present late with advanced disease or as an emergency.15 Cultural and language barriers are common. Children who present for surgery in LMICs are often anaemic, malnourished, small for their age, and their precise age may not even be known.
Equipment factors
A wide range of equipment sizes (face masks, oropharyngeal airways, laryngeal mask airways, tracheal tubes, laryngoscopes, and i.v. cannulae) are needed to adequately anaesthetize a diverse paediatric population.15,16 In a low-resource setting, there are often shortages or absences of equipment and what is available might have been reused many times after rudimentary decontamination procedures with disinfectants such as chlorine. The range of anaesthestic drugs available may be narrow and sometimes unfamiliar. Drug preparations may be out of date and those that require refrigeration may have been stored at ambient temperature, hampering their efficacy. Piped oxygen is often unavailable with oxygen usually being provided by cylinders. End-tidal agent and carbon dioxide monitoring is almost universally absent. Whether other forms of non-invasive monitoring, such as non-invasive blood pressure, electrocardiogram, and pulse oximetry, are available will vary between centres.
Local system and infrastructural factors
There is likely to be an inconsistent supply of homologous blood components. Standard infection control precautions are not always followed because of a lack of understanding or training, and sterilization facilities may be unreliable because of lack of servicing of equipment. Patients may face delays in receiving their surgery because of waiting lists, lack of beds, inadequate finances to pay for their treatment, or the lack of a local surgeon resulting in them having to travel further afield. Post-anaesthetic care facilities, if present, are usually very basic and consist of an area where the patient is kept for a very brief period of time prior to returning to the parent or ward. The presence of nursing staff, monitoring equipment, an oxygen supply, or suction in this area is not always guaranteed.
Systems for clinical governance are unlikely to exist and the degree of documentation of anaesthesia and anaesthesia-related events will be highly variable. Power outages and interruptions to water supply may be frequent and unpredictable.
It is well recognized that many LMICs are unable to meet the standards for anaesthesia provision set by international organizations such as the WHO and World Federation of Societies of Anesthesiologists (WFSA).17 Rather than imposing unachievable standards on systems operating within tight constraints, more recent and realistic approaches suggest focusing on the provision of guidance as to the bare minimum requirements for the delivery of safe anaesthesia care while simultaneously encouraging aiming for a higher standard through better education and local engagement.
Addressing the challenges
Although it is impossible to predict every eventuality or prescribe a ‘recipe’ for every scenario, some of these challenges can be addressed through careful planning and clear communication within teams. Patient factors can to a certain extent be addressed through the preoperative workup and perioperative care as described in the next section. Equipment factors are difficult for the individual visiting anaesthetist to address in a sustainable way. It may be worth contacting local anaesthesia providers or colleagues who have recently visited the centre to see what is needed and whether such equipment can be sourced through donations to provide immediate relief in the short term. Local system and widespread infrastructural factors are beyond the capacity of the individual short-term visiting anaesthetist to address; however, it is important that said individual makes himself or herself aware of the current situation in the hospital and country that they are visiting.
Preoperative assessment and planning
The importance of the clinical history and physical examination by the responsible anaesthesia provider cannot be overemphasized. Previously undiagnosed congenital abnormalities may be detected for the first time at pre-assessment, which may impact on anaesthesia conduct and planning, e.g. the child with congenital cardiac disease or the anticipated difficult paediatric airway. Anaemia is common and the child may suffer from concomitant infectious diseases such as tuberculosis, malaria, parasitic or diarrhoeal illnesses, or human immunodeficiency virus. There may be a history of treatment with traditional medicines that may have further delayed presentation. To tackle cultural and language barriers and optimize doctor–patient and doctor–parent communication, the use of an interpreter such as a local member of staff is strongly advised.
Often little can be done to improve the nutritional state of the child in the short term before surgery; however, efforts should be made to obtain an accurate weight to ensure appropriate dosing of drugs, estimation of blood volume, administration of i.v. fluids or blood components, and selection of appropriate equipment. If using age-based formulae to estimate weight, the practitioner should be mindful that these formulae have been validated in children from high-income countries. Although malnutrition in children is much more common in LMICs, obesity is also on the rise in urban areas.18 Weight estimation tools such as the Broselow tape can be extremely valuable19 though rarely available; therefore, it may be prudent for the visiting anaesthetist to bring one with them.
A visiting anaesthetist should familiarize himself or herself with what resources are available locally within the hospital as well as in the wider community or country. There may be occasions when it is unsafe to proceed, e.g. a child requiring a laparotomy for splenectomy, where there is no local blood bank or intensive care facility. Surgery may need to be postponed, cancelled, or referred to another ‘more resourced’ centre if this is an option. Such decisions can lead to conflict and should be carefully considered while keeping patient safety paramount.
Induction
As in paediatric practice worldwide, inhalational induction of anaesthesia is common and can be advantageous when attempting to secure intravenous access. In the context of severe dehydration, however, profound hypotension can result, thus caution should be exercised and inhalational induction may not be the safest technique in those circumstances.
The visiting anaesthetist should familiarize himself or herself with the pharmacology of the drugs available to them and consult local experience. The use of halothane remains commonplace in low-resource settings and anaesthetists should be familiar with the properties of this agent before using it. Deep halothane anaesthesia can be hazardous for the hypovolaemic patient and the combination of halothane and hypercarbia can lead to arrhythmias. Treatment includes a period of hyperventilation to decrease the carbon dioxide levels. Nitrous oxide as a co-induction agent is not usually available. Oxygen is often provided from cylinder supplies; however, some anaesthetic machines designed for poorly resourced environments, such as the Glostavent® Anaesthetic Machine (Fig. 1), feature oxygen concentrators.
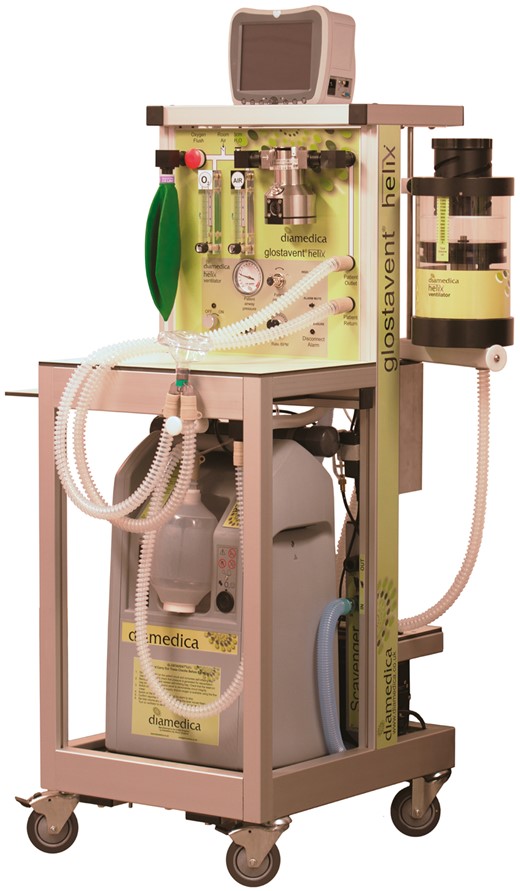
If using this piece of equipment, the practitioner should be mindful that increasing the fresh gas flow as during gaseous induction will adversely affect the inspired oxygen concentration; therefore, a balance must be struck between oxygen delivery and desired speed of onset. The Glostavent® anaesthetic machine is designed for remote environments and can function without a supply of compressed gas or electricity and can work as a continuous-flow or draw-over anaesthetic machine.20 Under normal circumstances, when electricity is available, the concentrator supplies both oxygen for the patient and compressed air to drive the ventilator. The uninterruptible power supply enables it to continue to function normally despite wide voltage fluctuations. If the electricity supply fails completely, the reserve oxygen cylinder automatically becomes the source of oxygen for the patient and pressure to drive the ventilator, so that mechanical ventilation can continue without interruption. In this mode, it is extremely economical; a standard size E cylinder can drive the ventilator and supply oxygen for 12 h.
For i.v. inductions, ketamine or propofol are the commonly used agents. The sympathomimetic properties of ketamine are advantageous in the haemodynamically unstable patient, and it has wider uses in the context of sedation and analgesia. The maintenance of anaesthesia under i.m. or i.v. ketamine for emergency and elective surgery is also commonplace particularly in remote rural areas. Ketamine provides anaesthesia while maintaining airway reflexes and spontaneous ventilation; therefore, in areas where there is no equipment with which to deliver volatile anaesthesia or secure the airway, this may be the only way anaesthesia can be provided to facilitate surgical procedures. Any excess salivation that may occur with ketamine anaesthesia can be managed by concomitant treatment with an anti-sialagogue, such as atropine or glycopyrrolate. Muscle relaxants are often avoided in favour of a spontaneously breathing patient but may be necessary for certain procedures.
The continued availability of low-cost of drugs, such as halothane and ketamine, is paramount to ensuring delivery of safe anaesthesia in LMICs. In 2015, attempts were made to impose international control over ketamine use; however, the WHO Expert Committee on Drug Dependence concluded that ‘ketamine abuse does not pose a global public health threat, while controlling it could limit access to the only anaesthetic and pain killer available in large areas of the developing world’.21
In the absence of gas analysis monitoring, extra care should be taken to ensure correct tracheal tube placement and avoid excessive depth of anaesthesia and hypoventilation. Correct tracheal tube placement should be confirmed clinically through chest auscultation and visual observation of chest wall expansion on positive pressure ventilation.
Maintenance
Maintenance of anaesthesia is usually with volatile agents or ketamine. Ketamine anaesthesia can be delivered through repeated i.m. or i.v. doses of the drug. Alternatively, in the absence of infusion pumps and short-acting opiates such as remifentanil, some practitioners may choose to run total i.v. anaesthesia by adding ketamine to a bag of fluid and controlling the infusion rate through counting the number of drips. Traditionally, low-resistance in-circuit draw-over vaporizers were used throughout the developing world; however, in contrast to 10 years ago, many low-resource settings are now equipped with anaesthetic machines that resemble those used in more highly resourced settings. These usually consist of an oxygen source, a variable bypass draw-over vaporizer, and some may even have incorporated ventilators with advanced ventilation settings. Regular maintenance and calibration of these machines, however, is not performed and inability to repair faults is common because of a lack of local technical expertise and access to machine parts. The visiting anaesthetist should carefully check any equipment before using it, be vigilant for inaccuracies in monitoring equipment, and keep a watchful eye clinically on the patient at all times.
For intraoperative fluid administration, balanced crystalloid and hypotonic dextrose-containing solutions are cheap and almost always available. When anaesthetizing smaller children, blood glucose management may be complicated by the lack of a blood glucose monitor. The supply of blood components is likely to be severely restricted, and whole blood is often used rather than individual components. When transfusing whole blood, a volume of 8 ml kg−1 is considered to raise the serum haemoglobin concentration by 1 g dL−1. The most commonly available vasoactive drugs are likely to be epinephrine and atropine with more selective agents being only intermittently obtainable.
Temperature control in children undergoing anaesthesia in low-resource settings can be problematic because of a lack of active warming devices, an inability to regulate ambient temperature, and perhaps an inability to measure temperature accurately. Working in a warm or tropical climate does not reduce or eliminate the risk of hypothermia from occurring in a child under anaesthesia; therefore, all reasonable measures should be undertaken to keep the child normothermic.
Postoperative care
Patients generally spend a minimal period of time in the recovery area and return directly to the ward where there is often no monitoring and patients may have to share a bed. The visiting anaesthetist should satisfy himself or herself that the patient has recovered consciousness to a level where it is appropriate for them to be discharged back to the ward before starting the next case. An available nurse to administer postoperative analgesia is a rare commodity; thus, it is strongly advisable to use local and regional anaesthetic techniques where possible and safe to do so as part of a multimodal analgesia approach. Good postoperative analgesia in low-resource settings is a huge challenge, and visiting and resident anaesthetists may find staff reluctant to administer opiates because of fear of opioid-induced side-effects such as respiratory depression. Doses of opioid should be cautiously titrated to effect, and cultural attitudes and pain behaviour must be considered when making a pain assessment. Opioid metabolism can vary markedly between individuals, with populations being stratified by age, gender, and ethnicity.22 Some Chinese patients may demonstrate a higher clearance of morphine or Asian or African populations an altered metabolism of codeine. Continuing education of local nursing and medical staff as to the benefits of good postoperative analgesia, such as improved patient comfort, suppression of the neuroendocrine stress response, reduction in postoperative pulmonary complications, and earlier mobilization and hospital discharge, should be undertaken to combat these challenges.
Availability of postoperative high dependency or intensive care facilities will depend on the individual centre; however, when these are available, the standard of such facilities is likely to be well below what is found in more developed health systems. The problems of lack of adequately trained staff, lack of equipment, poor maintenance, and frequent failure of existing equipment, and the wider infrastructural inadequacies that also exist outside of the theatre setting should be borne in mind when planning postoperative care.
Clinical example
This case was encountered by one of the authors while working in an LMIC.
Case description
A 7-year-old girl with sickle cell disease and a haemoglobin of 8 g dL−1 presented to theatre for a splenectomy having been cancelled twice previously because of lack of available blood products. The patient was malnourished, dehydrated, tachypnoeic, anxious, and distressed. As blood was now available, a decision was made to proceed. I.V. access was difficult to perform in the awake child; therefore, the patient underwent a gaseous induction using halothane and oxygen. Although attempts to secure i.v. access were ongoing, there was a sudden power outage and the theatre complex was plunged into complete darkness apart from some light provided by the anaesthetic machine.
Author’s account
‘It was important to remain calm, call for help, maintain the airway, and adequate oxygenation. The anaesthetic machine in use required electricity but ran on a battery of unknown duration therefore halothane and oxygen could still be delivered. Torches on mobile phones provided light while attempts to establish i.v. access continued. When this was achieved, a laryngeal mask airway was inserted, and the patient was allowed to breathe spontaneously while a staff member fetched a self-inflating bag and organized an extra oxygen cylinder in the event of anaesthetic machine failure. Although the surgeons were keen to start surgery as soon as possible, it was agreed to wait while the cause of the outage was being established and additional equipment could be obtained. Hospital management was contacted, the cause of the outage established, and the electricity supply reconnected after 40 min. The patient was intubated and ventilated for the procedure and ensuing surgery and recovery was uneventful.’
Author’s reflections
‘This case would be challenging in any environment, but a setting where resources are low presents additional challenges. At the hospital where this case occurred three paediatric theatres were usually in operation, two for elective work and one for emergencies. The level of supervision was inadequate, it being common practice that one consultant would supervise three anaesthesia trainees or non-physician anaesthesia providers with complex paediatric cases occurring simultaneously. All of the equipment issues described above were present with limited access to smaller sized tracheal tubes, frequent reuse of single-use equipment, poor equipment maintenance, an inconsistent supply of anaesthetic drugs, lack of basic monitoring, and inability to keep patients warm. As well as these challenges, human factors presented significant difficulty. Communication between surgeons, scrub staff, and anaesthetists was often inadequate and particularly vulnerable to break down in an emergency scenario. Institution of the WHO checklist played an important role in improving the organization of cases coming to theatre and empowered staff to become more proactive in highlighting potential problems especially with regard to emergency cases. This had not previously been a routine practice in theatre but resulted in better patient outcomes and reduction number of critical incidents and I believe a reduction in morbidity and mortality.’
Personal and professional aspects of working in LMICs
The personal and professional gains from spending a period of time practising anaesthesia in an LMIC are numerous. Professional gains include exposure to a wide range of advanced pathology and further development of skills in communication, teaching, and teamwork through working cross-culturally. Experience of a less developed system will also provide greater insight into how more ‘developed’ systems have evolved with regard to patient safety and improved productivity. Personal gains include appreciation of the challenges faced by colleagues working within resource limitations, the opportunity for the bidirectional sharing of knowledge and experience, and the making of new friends and networks in the global anaesthesia community. Being confronted with the effects and injustices of extreme poverty and inequality while working in a low-income country can be difficult. Nevertheless, the visiting anaesthetist can make a contribution to the system, with short-term trips helping to offload some of the surgical burden in the immediate term through service provision.
There is much to be done to raise the standards of anaesthesia and perioperative care provision in LMICs to that comparable with developed health systems. The introduction and continuation of sustainable improvement requires long-term commitment, and initiatives to improve anaesthesia provision in Africa through postgraduate training and the establishment of anaesthesia as a recognized medical specialty are already under way. Through training, government investment, and support from the international anaesthetic community, it is hoped that the phenomenon of avoidable perioperative deaths in LMICs will be abolished and safe, high-quality perioperative care will be accessible to all children (and indeed adults) throughout the world.23
Declaration of interest
None declared.
MCQs
The associated MCQs (to support CME/CPD activity) can be accessed at http://www.oxforde-learning.com/journals/ by subscribers to BJA Education.
References
The Glostavent® Anaesthesia Machine [Internet site]. Available from http://www.diamedica.co.uk/english/product_details.cfm?id=196 (accessed 23 March 2017)





