-
PDF
- Split View
-
Views
-
Cite
Cite
Orr Shauly, Troy Marxen, Ambika Menon, Courtney Swan, Erica Smearman, Daniel J Gould, Multimodal Pain Control in Abdominoplasty: A Systematic Review and Algorithm of Optimal Pain Management, Aesthetic Surgery Journal, Volume 44, Issue Supplement_1, September 2024, Pages S22–S30, https://doi.org/10.1093/asj/sjad381
Close - Share Icon Share
Abstract
The procedure with the highest rate of opioid prescription in plastic surgery is abdominoplasty. Additionally, plastic surgery patients are at a particularly elevated risk of becoming opioid-dependent. The main objective of this study was to perform a systematic review and create an algorithm for a multimodal pain regimen specific to patients undergoing abdominoplasty. A systematic search of the research literature was performed to summarize the prevailing understanding of multimodal pain control in the management of abdominoplasty. The initial search yielded 448 articles. Sixty-eight manuscripts were identified for full-text review. The effectiveness of current strategies was evaluated by way of pain scores, opioid usage, and length of stay, as well as other measures of physical function such as time to early mobilization. In 32 studies involving 2451 patients, the efficacy of different pain regimens during abdominoplasty was evaluated. Among nontraditional, opioid-sparing analgesia, efficacy of treatment interventions for improved pain and decreased opioid usage was found inall studies. Among local infusion studies, efficacy of treatment interventions for improved pain and decreased opioid usage was found in 78% of studies. Last, among regional block studies, efficacy of treatment interventions for improved pain was found in 87%, with 73% efficacy for decreased opioid usage. Multimodal pain regimens in abdominoplasty have the potential to play an important role in opioid-sparing practices in medicine by incorporating nonopioid pain adjuvants such as nonsteroidal anti-inflammatory drugs and transversus abdominis plane blocks in the preoperative, perioperative, and postoperative periods.

Postoperative pain remains 1 of the most significant deterrents to patients seeking abdominoplasty. Anxiety may be elicited in patients who have seen their friends or family undergo similar procedures that entail long recoveries requiring medications and possibly the use of a wheelchair or walker. This coupled with changes in the way we view opioid use in medicine has pushed us to seek better pain control methods for surgery. The opioid epidemic is a well-known challenge in American healthcare. Since the beginning of the COVID-19 pandemic, opioid deaths have increased at an alarming rate.1 Primary care physicians have decreased opioid prescriptions for the management of chronic pain, however opioids are still commonly required for the management of postoperative pain at an elevated rate.2 Among aesthetic plastic surgeons, opioid-prescribing practices are heavily dependent upon the procedure. The procedure with the highest rate of opioid prescription is abdominoplasty (91%), and the procedure with the lowest rate is blepharoplasty (58%).3 Additionally, patients who undergo plastic surgery are at a particularly elevated risk of becoming opioid-dependent.3,4 While the recent increase in Enhanced Recovery After Surgery (ERAS) protocols have resulted in decreased opioid-prescribing practices, it is still less than common for plastic surgeons to engage in opioid counseling habits with patients.5
As medicine has engaged in opioid-sparing strategies over the last 2 decades, the standard of care for pain management regimens has begun to shift toward a multimodal approach. Multimodal pain management from a surgical perspective should include differing amounts of nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, opioids, local infiltration, regional blocks, regional infusion, and epidurals.6 The exact combination depends upon the specific patient and procedure. For surgeons, the multimodal approach to pain management can be broken down into 3 distinct time periods: preoperative induction, intraoperative interventions, and postoperative management. While much of the focus surrounding opioid-prescribing practices has been on the postoperative period, preoperative oral and intraoperative intravenous multimodal pain regimens can also decrease subsequent postoperative pain scores and opioid use.7 Furthermore, changing from opioid to nonopioid adjuvants can similarly reduce pain scores while also maintaining opioid-sparing practices.8
Nonopioid pain adjuvants are the backbone of a multimodal pain regimen that is shifting toward an opioid-sparing approach. Traditional oral pain adjuvants include NSAID medications, acetaminophen, gabapentin, and dexamethasone. Additional nonopioid adjuvants include local and regional anesthesia, which can be administered by local injections, catheter pumps, and ultrasound-guided nerve blocks in the preoperative and intraoperative periods.9
Oral pain adjuvants are a critical component of a multimodal pain regimen. NSAIDs and selective COX-2 inhibitors are very effective and have been shown to reduce opioid consumption after plastic surgery procedures and can be safely incorporated into all 3 perioperative periods.8,10 Similarly, acetaminophen by several routes is highly effective and can be given preoperatively to reduce pain and opioid consumption.11 Gabapentinoids, such as gabapentin, are anticonvulsants that are commonly administered as pain adjuncts and can also be given perioperatively to reduce postoperative pain and opioid consumption.7,12 Glucocorticoids, such as dexamethasone, are another pain adjunct that can be given intraoperatively to reduce postoperative pain, opioid consumption, and postoperative nausea or vomiting.13,14
Non-oral pain adjuvants include local and regional anesthesia. Local injections have been a mainstay of surgical site anesthesia for decades and have recently started to incorporate longer lasting formulations, as have catheter infusions, to help mitigate the main downside of a short half-life.15 Local injections have been able to improve postoperative nausea and vomiting, in addition to reducing pain scores, opioid usage, and length of hospital stays.16,17 Regional anesthesia as part of a multimodal pain regimen consists of various nerve blocks, differing based on location.18 The optimal site of nerve block has been an area of active research, although the most common site, the transversus abdominis plane, has been shown to reduce opioid usage, length of stay, and pain scores.19-21
Multimodal pain regimens incorporate different combinations of pain adjuvants integrated over the course of the preoperative, intraoperative, and postoperative periods. As a result, patients ideally have shorter length of hospital or postoperative recovery stays, require fewer opioids, and experience less overall pain. The outcomes that help determine the success of the multimodal pain approach are measured by pain scores (0-10), opioid usage (mg equivalents) in the immediate postoperative period and 1 to 30 days after surgery, and various measures of functional status that are often delayed by prolonged opioid use, such as time to driving, time to ambulation, and length of hospital stay.22
The main objective of this review was to identify the current strategies of care and synthesize an algorithm for multimodal pain control in abdominoplasty. The effectiveness of current strategies was evaluated by way of pain scores, opioid usage, and length of stay, as well as other measures of physical function such as time to early mobilization.
METHODS
A systematic search of the research literature was performed by authors A.M. and T.M. on December 31, 2021, to summarize the prevailing understanding of multimodal pain control in the management of abdominoplasty. The review was performed with the electronic databases Cochrane (Wiley, Hoboken, NJ); Medline/PubMed (National Institutes of Health, Bethesda, MD); and Google Scholar (Mountain View, CA). The following search terms were entered: ((((Multimodal) OR (pain)) OR (recovery) OR (post-operative)) AND (abdominoplasty)).
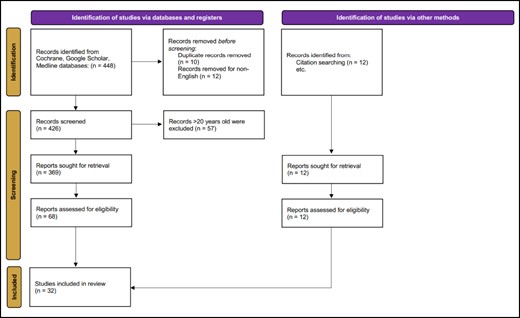
The initial search yielded 448 articles. This initial search was reviewed by author O.S. and conflicts were resolved by author D.G. After excluding duplicates and non-English articles, there were a total of 426 articles. Narrowing the time frame to articles written over the past 20 years left 369 articles. The remaining 369 articles were screened for review based on title and abstract for further manuscript evaluation. Sixty-eight manuscripts were identified for full-text review. Of the 68 manuscripts, 12 were identified through citation searches (Figure 1). Articles were identified by those that included objective data of opioid use in postabdominoplasty patients, those that specified their postoperative pain regimen for these patients, and those that objectively measured pain scores or efficacy of treatment.
RESULTS
Nontraditional Opioid-Sparing Analgesia
Eight studies involving 1023 patients met the criteria for investigation of nontraditional opioid-sparing analgesia in abdominoplasty. In all studies we found efficacy of treatment interventions for improved pain and decreased opioid usage. One study reported efficacy for improved functional status.21 Seven studies were prospective, randomized trials.9,21-26 One study was a review on multimodal pain regimens in plastic surgery.8 All 8 studies reported an efficacy for improved pain control and decreased opioid usage. In 3 studies, efficacy for ketamine was demonstrated. Two studies reported efficacy for meloxicam.25,26 One study reported efficacy for with tramadol (Table 1).24
Studies That Investigated Nontraditional Opioid-Sparing Analgesia for Abdominoplasty
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Ali et al25 | 34150574 | 2021 | Prospective, Randomized | Ketamine is similar to morphine in analgesia | 160 | Decreased | Decreased | No Change |
| Barker et al9 | 334225573 | 2020 | Review | NSAIDs, acetaminophen, gabapentin, dexamethasone are safe and preferrable to opioids | NA | Decreased | Decreased | No Change |
| Leiman27 | NA | 2017 | Prospective, Randomized | Mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No Change |
| Mansour et al28 | 34754346 | 2021 | Prospective, Randomized | Ketamine added to TAP demonstrated greater pain control than TAP alone | 50 | Decreased | Decreased | No Change |
| Minkowitz29 | 32409981 | 2020 | Prospective, Randomized | IV tramadol > IV morphine for postoperative pain | 370 | Decreased | Decreased | No Change |
| Singla30 | 30276064 | 2018 | Prospective, Randomized | IV meloxicam is beneficial | 219 | Decreased | Decreased | No Change |
| Sun et al10 | 18292445 | 2008 | Prospective, Randomized | Celecoxib is beneficial perioperatively and postoperatively | 120 | Decreased | Decreased | No Change |
| Varas31 | 33235492 | 2020 | Prospective, Randomized | IV ketamine + magnesium is beneficial | 63 | Decreased | Decreased | Increased |
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Ali et al25 | 34150574 | 2021 | Prospective, Randomized | Ketamine is similar to morphine in analgesia | 160 | Decreased | Decreased | No Change |
| Barker et al9 | 334225573 | 2020 | Review | NSAIDs, acetaminophen, gabapentin, dexamethasone are safe and preferrable to opioids | NA | Decreased | Decreased | No Change |
| Leiman27 | NA | 2017 | Prospective, Randomized | Mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No Change |
| Mansour et al28 | 34754346 | 2021 | Prospective, Randomized | Ketamine added to TAP demonstrated greater pain control than TAP alone | 50 | Decreased | Decreased | No Change |
| Minkowitz29 | 32409981 | 2020 | Prospective, Randomized | IV tramadol > IV morphine for postoperative pain | 370 | Decreased | Decreased | No Change |
| Singla30 | 30276064 | 2018 | Prospective, Randomized | IV meloxicam is beneficial | 219 | Decreased | Decreased | No Change |
| Sun et al10 | 18292445 | 2008 | Prospective, Randomized | Celecoxib is beneficial perioperatively and postoperatively | 120 | Decreased | Decreased | No Change |
| Varas31 | 33235492 | 2020 | Prospective, Randomized | IV ketamine + magnesium is beneficial | 63 | Decreased | Decreased | Increased |
IV, intravenous; NSAID, nonsteroidal anti-inflammatory drug, TAP, transversus abdominis plane nerve block.
Studies That Investigated Nontraditional Opioid-Sparing Analgesia for Abdominoplasty
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Ali et al25 | 34150574 | 2021 | Prospective, Randomized | Ketamine is similar to morphine in analgesia | 160 | Decreased | Decreased | No Change |
| Barker et al9 | 334225573 | 2020 | Review | NSAIDs, acetaminophen, gabapentin, dexamethasone are safe and preferrable to opioids | NA | Decreased | Decreased | No Change |
| Leiman27 | NA | 2017 | Prospective, Randomized | Mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No Change |
| Mansour et al28 | 34754346 | 2021 | Prospective, Randomized | Ketamine added to TAP demonstrated greater pain control than TAP alone | 50 | Decreased | Decreased | No Change |
| Minkowitz29 | 32409981 | 2020 | Prospective, Randomized | IV tramadol > IV morphine for postoperative pain | 370 | Decreased | Decreased | No Change |
| Singla30 | 30276064 | 2018 | Prospective, Randomized | IV meloxicam is beneficial | 219 | Decreased | Decreased | No Change |
| Sun et al10 | 18292445 | 2008 | Prospective, Randomized | Celecoxib is beneficial perioperatively and postoperatively | 120 | Decreased | Decreased | No Change |
| Varas31 | 33235492 | 2020 | Prospective, Randomized | IV ketamine + magnesium is beneficial | 63 | Decreased | Decreased | Increased |
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Ali et al25 | 34150574 | 2021 | Prospective, Randomized | Ketamine is similar to morphine in analgesia | 160 | Decreased | Decreased | No Change |
| Barker et al9 | 334225573 | 2020 | Review | NSAIDs, acetaminophen, gabapentin, dexamethasone are safe and preferrable to opioids | NA | Decreased | Decreased | No Change |
| Leiman27 | NA | 2017 | Prospective, Randomized | Mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No Change |
| Mansour et al28 | 34754346 | 2021 | Prospective, Randomized | Ketamine added to TAP demonstrated greater pain control than TAP alone | 50 | Decreased | Decreased | No Change |
| Minkowitz29 | 32409981 | 2020 | Prospective, Randomized | IV tramadol > IV morphine for postoperative pain | 370 | Decreased | Decreased | No Change |
| Singla30 | 30276064 | 2018 | Prospective, Randomized | IV meloxicam is beneficial | 219 | Decreased | Decreased | No Change |
| Sun et al10 | 18292445 | 2008 | Prospective, Randomized | Celecoxib is beneficial perioperatively and postoperatively | 120 | Decreased | Decreased | No Change |
| Varas31 | 33235492 | 2020 | Prospective, Randomized | IV ketamine + magnesium is beneficial | 63 | Decreased | Decreased | Increased |
IV, intravenous; NSAID, nonsteroidal anti-inflammatory drug, TAP, transversus abdominis plane nerve block.
Local Infusions
Nine studies investigating 600 patients met the criteria for investigation of local and regional infusion analgesia in abdominoplasty. A total of 78% of studies reported efficacy of treatment interventions for improved pain and decreased opioid usage. In addition, 44% of studies reported efficacy for improved functional status. One study was a review on multimodal pain regimens in plastic surgery.16 Three studies were retrospective.27-29 Four studies were prospective, randomized trials.26,30-32 One study was a mixed retrospective/prospective study (Table 2).33
Studies That Investigated Local and Regional Infusion Analgesia for Abdominoplasty
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Bray et al32 | 17312513 | 2007 | Retrospective | Pain pumps are not beneficial | 73 | No change | No change | No change |
| Chavez-Abraham et al33 | 21136251 | 2011 | Retrospective | Pain pumps are beneficial | 215 | Decrease | Decrease | No change |
| Giordano et al34 | 31864888 | 2020 | Retrospective | Pain pumps are beneficial and may also shorten LOS in patients with obesity | 61 | Decreased | Decreased | Increased |
| Kakagia et al35 | 17205251 | 2007 | Prospective | Levobupivacaine is beneficial | 46 | Decreased | No change | No change |
| Randomized | ||||||||
| Leiman et al27 | NA | 2017 | Prospective | Extended-release mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Mentz et al36 | 16177875 | 2005 | Prospective | Pain pumps are beneficial and may allow early mobilization | 20 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Patel et al37 | 18176268 | 2008 | Retrospective | Pain pumps are beneficial and may decrease LOS | 54 | Decreased | Decreased | Increased |
| Prospective | ||||||||
| Roy et al17 | 31192870 | 2019 | Review | Continuous local wound infusion is beneficial | NA/28 | Decreased | Decreased | No change |
| Salama38 | 29962527 | 2018 | Prospective | Continuous local wound infusion with bilateral TAP is superior | 90 | No changea | Decreased | Increased |
| Randomized |
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Bray et al32 | 17312513 | 2007 | Retrospective | Pain pumps are not beneficial | 73 | No change | No change | No change |
| Chavez-Abraham et al33 | 21136251 | 2011 | Retrospective | Pain pumps are beneficial | 215 | Decrease | Decrease | No change |
| Giordano et al34 | 31864888 | 2020 | Retrospective | Pain pumps are beneficial and may also shorten LOS in patients with obesity | 61 | Decreased | Decreased | Increased |
| Kakagia et al35 | 17205251 | 2007 | Prospective | Levobupivacaine is beneficial | 46 | Decreased | No change | No change |
| Randomized | ||||||||
| Leiman et al27 | NA | 2017 | Prospective | Extended-release mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Mentz et al36 | 16177875 | 2005 | Prospective | Pain pumps are beneficial and may allow early mobilization | 20 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Patel et al37 | 18176268 | 2008 | Retrospective | Pain pumps are beneficial and may decrease LOS | 54 | Decreased | Decreased | Increased |
| Prospective | ||||||||
| Roy et al17 | 31192870 | 2019 | Review | Continuous local wound infusion is beneficial | NA/28 | Decreased | Decreased | No change |
| Salama38 | 29962527 | 2018 | Prospective | Continuous local wound infusion with bilateral TAP is superior | 90 | No changea | Decreased | Increased |
| Randomized |
aPain scores at rest were equivocal. LOS, length of hospital stay; TAP, transversus abdominis plane nerve block.
Studies That Investigated Local and Regional Infusion Analgesia for Abdominoplasty
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Bray et al32 | 17312513 | 2007 | Retrospective | Pain pumps are not beneficial | 73 | No change | No change | No change |
| Chavez-Abraham et al33 | 21136251 | 2011 | Retrospective | Pain pumps are beneficial | 215 | Decrease | Decrease | No change |
| Giordano et al34 | 31864888 | 2020 | Retrospective | Pain pumps are beneficial and may also shorten LOS in patients with obesity | 61 | Decreased | Decreased | Increased |
| Kakagia et al35 | 17205251 | 2007 | Prospective | Levobupivacaine is beneficial | 46 | Decreased | No change | No change |
| Randomized | ||||||||
| Leiman et al27 | NA | 2017 | Prospective | Extended-release mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Mentz et al36 | 16177875 | 2005 | Prospective | Pain pumps are beneficial and may allow early mobilization | 20 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Patel et al37 | 18176268 | 2008 | Retrospective | Pain pumps are beneficial and may decrease LOS | 54 | Decreased | Decreased | Increased |
| Prospective | ||||||||
| Roy et al17 | 31192870 | 2019 | Review | Continuous local wound infusion is beneficial | NA/28 | Decreased | Decreased | No change |
| Salama38 | 29962527 | 2018 | Prospective | Continuous local wound infusion with bilateral TAP is superior | 90 | No changea | Decreased | Increased |
| Randomized |
| . | PMID . | Year . | Type of study . | Summary . | No. patients/studies . | Pain scores . | Opioid usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Bray et al32 | 17312513 | 2007 | Retrospective | Pain pumps are not beneficial | 73 | No change | No change | No change |
| Chavez-Abraham et al33 | 21136251 | 2011 | Retrospective | Pain pumps are beneficial | 215 | Decrease | Decrease | No change |
| Giordano et al34 | 31864888 | 2020 | Retrospective | Pain pumps are beneficial and may also shorten LOS in patients with obesity | 61 | Decreased | Decreased | Increased |
| Kakagia et al35 | 17205251 | 2007 | Prospective | Levobupivacaine is beneficial | 46 | Decreased | No change | No change |
| Randomized | ||||||||
| Leiman et al27 | NA | 2017 | Prospective | Extended-release mixed ratio of meloxicam/bupivacaine is beneficial | 41 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Mentz et al36 | 16177875 | 2005 | Prospective | Pain pumps are beneficial and may allow early mobilization | 20 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Patel et al37 | 18176268 | 2008 | Retrospective | Pain pumps are beneficial and may decrease LOS | 54 | Decreased | Decreased | Increased |
| Prospective | ||||||||
| Roy et al17 | 31192870 | 2019 | Review | Continuous local wound infusion is beneficial | NA/28 | Decreased | Decreased | No change |
| Salama38 | 29962527 | 2018 | Prospective | Continuous local wound infusion with bilateral TAP is superior | 90 | No changea | Decreased | Increased |
| Randomized |
aPain scores at rest were equivocal. LOS, length of hospital stay; TAP, transversus abdominis plane nerve block.
Regional Blocks
Fifteen studies involving 828 patients met the criteria for investigation of regional nerve blocks in abdominoplasty. In 66% of the studies the transversus abdominis plane (TAP) block was primarily evaluated or found to have highest efficacy.32,34-42 Two studies primarily considered the quadratus lumborum (QL) block.5,43 Two additional studies reported on combination blocks, consisting of multiple regions.18,44-49 One study reported on intercostal (rib) blocks.20
Outcomes of different regional blocks were also evaluated. The majority of studies (87%) reported efficacy of treatment interventions for improved pain and 73% of studies reported efficacy for decreased opioid usage. In addition, 47% of studies reported efficacy for improved functional status (Table 3).
| . | PMID . | Year . | Type of study . | Type of Nerve Block . | No. patients/studies . | Pain Scores . | Opioid Usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Abo-Zeid et al39 | 30429742 | 2018 | Prospective | TAP | 48 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Alotaibi et al40 | 33397174 | 2021 | Prospective | TAP | 60 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Araco et al41 | 20798634 | 2010 | Prospective | TAP | 75 | Decreased | No change | No change |
| Randomized | ||||||||
| Bjelland et al6 | 31112512 | 2019 | Prospective | QL | 50 | No change | No change | No change |
| Randomized | ||||||||
| Fiala42 | 25536505 | 2015 | Prospective | TAP | 32 | Decreased | Decreased | No change |
| Randomized | ||||||||
| El Hawary et al26 | 334225573 | 2020 | Review | TAP | NA/126 | Decreased | Decreased | No change |
| Feng22 | 21042130 | 2010 | Retrospective | Combination | 209 | Decreased | Decreased | Increased |
| Gravante et al43 | 20517653 | 2011 | Prospective | TAP | 51 | Decreased | No change | No change |
| Randomized | ||||||||
| Michaels and Eko24 | 19644285 | 2009 | Retrospective | IC | 68 | Decreased | Decreased | Increased |
| Meouchy et al44 | 33710163 | 2021 | Prospective | QL | 40 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Morales et al45 | 24214950 | 2013 | Retrospective | Combination | 64 | Decreased | Decreased | Increased |
| Oppenheimer et al46 | 26545224 | 2016 | Pilot | TAP | 13 | Decreased | No change | No change |
| Salama38 | 29962527 | 2018 | Prospective | TAP | 90 | No changea | Decreased | Increased |
| Randomized | ||||||||
| Sforza et al47 | 21788846 | 2011 | Prospective | TAP | 28 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Vonu et al48 | 30680144 | 2020 | Review | TAP | NA/8 | Decreased | Decreased | No change |
| . | PMID . | Year . | Type of study . | Type of Nerve Block . | No. patients/studies . | Pain Scores . | Opioid Usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Abo-Zeid et al39 | 30429742 | 2018 | Prospective | TAP | 48 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Alotaibi et al40 | 33397174 | 2021 | Prospective | TAP | 60 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Araco et al41 | 20798634 | 2010 | Prospective | TAP | 75 | Decreased | No change | No change |
| Randomized | ||||||||
| Bjelland et al6 | 31112512 | 2019 | Prospective | QL | 50 | No change | No change | No change |
| Randomized | ||||||||
| Fiala42 | 25536505 | 2015 | Prospective | TAP | 32 | Decreased | Decreased | No change |
| Randomized | ||||||||
| El Hawary et al26 | 334225573 | 2020 | Review | TAP | NA/126 | Decreased | Decreased | No change |
| Feng22 | 21042130 | 2010 | Retrospective | Combination | 209 | Decreased | Decreased | Increased |
| Gravante et al43 | 20517653 | 2011 | Prospective | TAP | 51 | Decreased | No change | No change |
| Randomized | ||||||||
| Michaels and Eko24 | 19644285 | 2009 | Retrospective | IC | 68 | Decreased | Decreased | Increased |
| Meouchy et al44 | 33710163 | 2021 | Prospective | QL | 40 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Morales et al45 | 24214950 | 2013 | Retrospective | Combination | 64 | Decreased | Decreased | Increased |
| Oppenheimer et al46 | 26545224 | 2016 | Pilot | TAP | 13 | Decreased | No change | No change |
| Salama38 | 29962527 | 2018 | Prospective | TAP | 90 | No changea | Decreased | Increased |
| Randomized | ||||||||
| Sforza et al47 | 21788846 | 2011 | Prospective | TAP | 28 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Vonu et al48 | 30680144 | 2020 | Review | TAP | NA/8 | Decreased | Decreased | No change |
aPain scores at rest were equivocal. IC, intercostal; QL, quadratus lumborum; TAP, transversus abdominis plane.
| . | PMID . | Year . | Type of study . | Type of Nerve Block . | No. patients/studies . | Pain Scores . | Opioid Usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Abo-Zeid et al39 | 30429742 | 2018 | Prospective | TAP | 48 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Alotaibi et al40 | 33397174 | 2021 | Prospective | TAP | 60 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Araco et al41 | 20798634 | 2010 | Prospective | TAP | 75 | Decreased | No change | No change |
| Randomized | ||||||||
| Bjelland et al6 | 31112512 | 2019 | Prospective | QL | 50 | No change | No change | No change |
| Randomized | ||||||||
| Fiala42 | 25536505 | 2015 | Prospective | TAP | 32 | Decreased | Decreased | No change |
| Randomized | ||||||||
| El Hawary et al26 | 334225573 | 2020 | Review | TAP | NA/126 | Decreased | Decreased | No change |
| Feng22 | 21042130 | 2010 | Retrospective | Combination | 209 | Decreased | Decreased | Increased |
| Gravante et al43 | 20517653 | 2011 | Prospective | TAP | 51 | Decreased | No change | No change |
| Randomized | ||||||||
| Michaels and Eko24 | 19644285 | 2009 | Retrospective | IC | 68 | Decreased | Decreased | Increased |
| Meouchy et al44 | 33710163 | 2021 | Prospective | QL | 40 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Morales et al45 | 24214950 | 2013 | Retrospective | Combination | 64 | Decreased | Decreased | Increased |
| Oppenheimer et al46 | 26545224 | 2016 | Pilot | TAP | 13 | Decreased | No change | No change |
| Salama38 | 29962527 | 2018 | Prospective | TAP | 90 | No changea | Decreased | Increased |
| Randomized | ||||||||
| Sforza et al47 | 21788846 | 2011 | Prospective | TAP | 28 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Vonu et al48 | 30680144 | 2020 | Review | TAP | NA/8 | Decreased | Decreased | No change |
| . | PMID . | Year . | Type of study . | Type of Nerve Block . | No. patients/studies . | Pain Scores . | Opioid Usage . | Functional status . |
|---|---|---|---|---|---|---|---|---|
| Abo-Zeid et al39 | 30429742 | 2018 | Prospective | TAP | 48 | Decreased | Decreased | No change |
| Randomized | ||||||||
| Alotaibi et al40 | 33397174 | 2021 | Prospective | TAP | 60 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Araco et al41 | 20798634 | 2010 | Prospective | TAP | 75 | Decreased | No change | No change |
| Randomized | ||||||||
| Bjelland et al6 | 31112512 | 2019 | Prospective | QL | 50 | No change | No change | No change |
| Randomized | ||||||||
| Fiala42 | 25536505 | 2015 | Prospective | TAP | 32 | Decreased | Decreased | No change |
| Randomized | ||||||||
| El Hawary et al26 | 334225573 | 2020 | Review | TAP | NA/126 | Decreased | Decreased | No change |
| Feng22 | 21042130 | 2010 | Retrospective | Combination | 209 | Decreased | Decreased | Increased |
| Gravante et al43 | 20517653 | 2011 | Prospective | TAP | 51 | Decreased | No change | No change |
| Randomized | ||||||||
| Michaels and Eko24 | 19644285 | 2009 | Retrospective | IC | 68 | Decreased | Decreased | Increased |
| Meouchy et al44 | 33710163 | 2021 | Prospective | QL | 40 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Morales et al45 | 24214950 | 2013 | Retrospective | Combination | 64 | Decreased | Decreased | Increased |
| Oppenheimer et al46 | 26545224 | 2016 | Pilot | TAP | 13 | Decreased | No change | No change |
| Salama38 | 29962527 | 2018 | Prospective | TAP | 90 | No changea | Decreased | Increased |
| Randomized | ||||||||
| Sforza et al47 | 21788846 | 2011 | Prospective | TAP | 28 | Decreased | Decreased | Increased |
| Randomized | ||||||||
| Vonu et al48 | 30680144 | 2020 | Review | TAP | NA/8 | Decreased | Decreased | No change |
aPain scores at rest were equivocal. IC, intercostal; QL, quadratus lumborum; TAP, transversus abdominis plane.
DISCUSSION
Goal-directed therapy with nonopiate alternatives is the best and most reasonable way to rapidly taper opiates (Figure 2). This coupled with other postoperative interventions to improve wound healing and reduce inflammation such as hyperbaric oxygen chamber treatment, nutrition supplements, and red-light therapy all serve to help reduce the opiate consumption and burden.
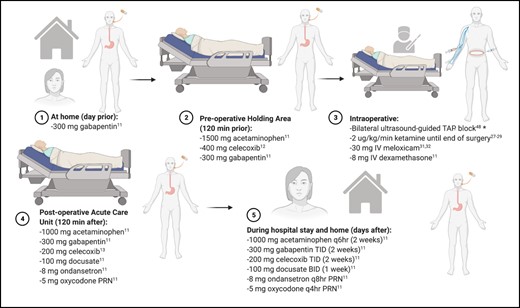
In the field of plastic and reconstructive surgery, there is a great responsibility to reduce the opioid burden on the community, while also improving postoperative pain and thereby increasing patient satisfaction.3 Because abdominoplasty can now be safely performed in an outpatient setting, reducing opioids in this procedure may help pave the way for similar multimodal pain regimens in other procedures in plastic surgery.23,24 In the post-COVID era, incorporating ERAS into plastic surgery protocols may help facilitate faster discharges and reduce the healthcare burden of prolonged hospital stays as well.25 This study is unique in that it is the first to perform a systematic review and present an algorithm for the ideal multimodal pain regimen specific to those patients undergoing abdominoplasty.
No doubt, in the future a prospective multiarm study will help elucidate the best interventions, however at this point many practices already incorporate several of these approaches to improve care. The senior author of this article (D.G.) utilizes all of the interventions with evidence described here in his practice to reduce postoperative pain and has published a retrospective review of cases and pain outcomes utilizing these approaches.50 However, over time these interventions will change; new medications may become available, and as the market changes access to resources may also change. It is incumbent on practitioners to continue to innovate and adapt their practices to further improve the patient experience. Pain control does not just affect opiate consumption; in fact, adequate pain control can lead to reduction in downtime and faster return to work as well as improved perception of the experience. Anecdotally, it has revolutionized the practice of the senior author (D.G.), with a specialized and personalized approach to each patient's needs and outcomes. Although there can be an additional cost burden to the patient, with insurance often not covering liposomal bupivacaine or intravenous acetaminophen administration, reliable postoperative pain reduction, decreased opioid use, and higher patient satisfaction are often worthwhile to the patient.
Additionally, there are surgical techniques that may reduce pain and improve recovery. These include progression tension sutures that offset tension on the closure site and allow for early upright mobilization. Pollock and Pollock anecdotally comment on improvements in the recovery phase and the senior author of this study agrees with those findings. In the future there may be a strategy to allow for completely painless abdominoplasty, and when that time comes it will allow for improved patient experience, care, and outcomes, while also allowing for improvements in plastic and reconstructive surgery.
There were several limitations to this review. While many studies show reduced opioid consumption and pain scores in the initial postoperative period, few studies allow effective assessment of pain over the weeks that follow due to the inherent limitations of retrospective questionnaires. Careful consideration should also be given to the side effects of a multimodal pain regimen, particularly bleeding, liver toxicity, dizziness, and respiratory depression. While rare, there are complications of anesthetic adjuvants that must be weighed against the possible benefits. In addition, thoughtful adoption of less intrusive forms of airway management (laryngeal mask airway), ventilation (spontaneous), and tissue-based anesthesia (infusions) all act together to minimize physiologic alterations during surgery, expedite recovery, and improve safety.49 These are being adopted nationwide in many ambulatory surgery centers and may be a confounding factor to these findings.
CONCLUSIONS
A multimodal approach to pain control in the preoperative, perioperative, and postoperative periods has been demonstrated to improve patient recovery after surgery, improve overall pain, and reduce the burden of opiate use. In the management of patients in plastic and reconstructive surgery, providers should strive to implement pain protocols that focus more heavily on nonopiate interventions in the perioperative course of the patient.
Acknowledgments
Development of figures in this article was possible with assistance from PRISMA guidelines and biorender.com (Toronto, Ontario, Canada), with a publication license.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
Funding for this supplement was provided by Pacira BioSciences, Inc. (Tampa, FL).
REFERENCES
Author notes
Drs Shauly, Marxen, Swan, and Smearman are residents and Ms Menon is a medical student, Division of Plastic and Reconstructive Surgery, Emory University, Atlanta, GA, USA.
Dr Gould is a plastic surgeon in private practice in Beverly Hills, CA and is the Research section co-editor for ASJ Open Forum.
- analgesics, non-narcotic
- anesthesia, conduction
- anti-inflammatory agents, non-steroidal
- length of stay
- pain
- perioperative care
- preoperative care
- pain management
- plastic surgery procedures
- abdominoplasty
- opioids
- pain score
- infusion procedures
- physical function
- early mobilization
- transversus abdominis plane block
- treatment effectiveness



