-
PDF
- Split View
-
Views
-
Cite
Cite
Jose L Cataneo, Sydney A Mathis, Kyle Bartelt, Allison Gelfond, Rodrigo Arias-Serrato, Parit A Patel, Developing the Aesthetic Postoperative Complication Score (APeCS) for Detecting Major Morbidity in Facial Aesthetic Surgery, Aesthetic Surgery Journal, Volume 44, Issue 5, May 2024, Pages 463–469, https://doi.org/10.1093/asj/sjad379
Close - Share Icon Share
Abstract
Facial aesthetic surgery encompasses a variety of procedures with complication rates that are difficult to estimate due to a lack of published data.
We sought to estimate major complication rates in patients undergoing facial aesthetic procedures and develop a risk assessment tool to stratify patients.
We utilized the Tracking Operation and Outcomes for Plastic Surgeons (TOPS) database from 2003-2018. The analytic database included major facial aesthetic procedures. Univariate analysis and a backward stepwise multivariate regression model identified risk factors for major complications. Regression coefficients were utilized to create the score. Performance robustness was measured with area under receiver operating characteristic curves and sensitivity analyses.
A total of 38,569 patients were identified. The major complication rate was 1.2% (460). The regression model identified risk factors including over 3 concomitant surgeries, BMI ≥25, ASA class ≥2, current or former smoker status, and age ≥45 as the variables fit for risk prediction (n = 13,004; area under curve: 0.68, standard error: 0.013, [0.62-0.67]). Each of the 5 variables counted for 1 point, except over 3 concomitant surgeries counting for 2, giving a score range from 0 to 6. Sensitivity analysis showed the cutoff point of ≥3 to best balance sensitivity and specificity, 58% and 66%, respectively. At this cutoff, 65% of cases were correctly classified as having a major complication.
We developed an acceptable risk prediction score with a cutoff value of ≥3 associated with correctly classifying approximately 65% of those at risk for major morbidity when undergoing face and neck aesthetic surgery.

See the Commentary on this article here.
Aesthetic or cosmetic surgery is growing in popularity, with over 2 million procedures performed in the United States in 2020.1,2 According to the most current Aesthetic Plastic Surgery National Databank Statistics from The Aesthetic Society, the 3 most popular surgeries performed were blepharoplasty, rhytidectomy, and rhinoplasty.2 This trend favoring facial aesthetic surgery highlights the importance of knowing the nuances of these procedures, and in particular understanding the most common complications and developing strategies to avoid them. Nevertheless, estimating morbidity for 1 or multiple facial procedures has remained challenging, because reports have been limited to small cohorts and technical or descriptive analyses.3-10 This gap in the literature can have a significant impact on how plastic surgeons communicate with patients regarding inherent complications. In addition, plastic surgeons have been unable to risk stratify certain subgroups at higher risk for morbidity, which can negatively affect patient selection for surgery.
Risk stratification models have proven to be beneficial in a myriad of surgical subspecialties.11-14 Moons et al mention that these models should provide accurate and validated estimates of probabilities of specific conditions or outcomes.12 Once validated, they help by guiding decision-making and improving patient outcomes.12 In plastic surgery, venous thromboembolism has been the sole subject of research utilizing risk assessment models.15-17 However, a risk model looking into major morbidity is lacking in the facial aesthetic literature. Morbidity rates have also been scantly studied, with a study reporting overall morbidity for rhinoplasty at 0.7% and rhytidectomy at 5.1%.10,18 To address this, we sought to estimate major morbidity rates in adults undergoing facial aesthetic surgery and develop a risk assessment tool through a national database developed by the American Society of Plastic Surgeons (ASPS).
METHODS
Database
Data were retrieved from the Tracking Operations and Outcomes for Plastic Surgeons (TOPS) national database. This is the largest aggregation of plastic surgery data assembled, including over 1.4 million plastic surgery procedures and outcomes.19 It is a Health Insurance Portability and Accountability Act (HIPAA) compliant registry available to ASPS members.10 Its main objectives are to evaluate clinical practice, to provide an evidence-based tool to compare patient outcomes, and to facilitate identification of clinical strengths and areas needing improvement.
Study Group
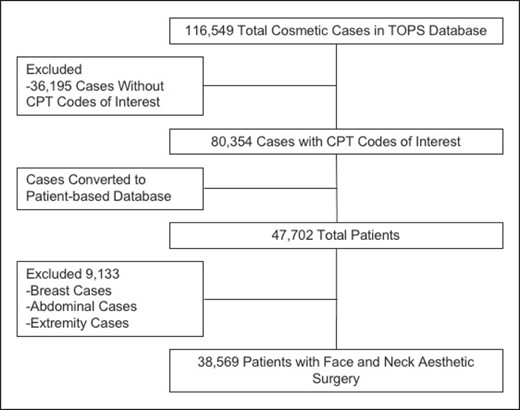
We queried the TOPS database from 2003 to 2018. The cohort included adult patients who underwent a surgical facial aesthetic procedure. The target population was isolated by Current Procedural Terminology (CPT) codes corresponding to neck lift (with or without extensive herniated fat, neck rhytidectomy with platysma tightening); upper blepharoplasty (with or without excessive skin); rhytidectomy (forehead, glabellar, cheek/chin/neck); deep plane rhytidectomy (rhytidectomy with superficial musculoaponeurotic system or SMAS flap); repair of brow ptosis; repair of blepharoptosis; medial and lateral canthopexy; genioplasty (subdivided into augmentation, single or multiple sliding osteotomy, and augmentation with bone graft); excision of excessive skin and subcutaneous tissue (including lipectomy and submental fat); primary rhinoplasty; secondary rhinoplasty; and otoplasty (Codes: 15820-15826,15828, 15829, 67900-67904, 67906, 67908, 21280, 21282, 21120-21123, 21125, 21127, 21137, 21138, 21139, 15838, 30400, 30410, 30420, 30430, 30435, 30450, 11950-11952, 11954, 15819, 69300). Patients who underwent concurrent procedures below the neck were excluded to avoid morbidity overestimation. Figure 1 illustrates the flowchart to achieve our cohort.
Variables and Outcomes
Demographic variables included were sex, age, BMI, race/ethnicity, smoking status, and American Society of Anesthesiologist (ASA) classification. A binary variable of “over 3 concomitant procedures” was created to describe concurrent facial surgical procedures. The main outcome analyzed was major complication rate. A major complication was defined as the following: if a patient presented with wound disruption, surgical site infection, return to the operating room, nerve injury, or other complication specific to a cosmetic facial procedure.
Score Development and Statistical Analysis
Continuous variables were described as means with standard error (SE) or medians with interquartile range (IQR). They were compared with t test or Wilcoxon rank-sum test, respectively. Categorical variables were described as frequencies and compared with the chi-squared test. Multivariate regression models with “major complications” as the independent variable were created to select the optimal risk factors for a risk stratification score. Goodness-of-fit test for the final model was assessed with the Pearson's chi-squared and Hosmer-Lemeshow tests. The score was created based on the regression coefficient.20,21 The coefficient from each risk factor was approximated to the closest integer and the sum of the integers was the score. Receiver operating characteristic (ROC) curve was performed to assess the diagnostic capability of the risk model, and sensitivity analysis measured its robustness. No statistical technique was employed for imputations on missing data. We assessed a final model with only observations that had all the risk factors available. Additionally, there was a “Total” column demonstrating the total available observations performed on each analysis. Statistical significance was established at an alpha value of 0.05. Statistical analyses were performed with StataCorp. 2015, Release 14 (College Station, TX). J.L.C., S.A.M., K.B., A.G., R.A.S., and P.A.P. performed the data retrieval and search for variables. J.L.C. and P.A.P. reviewed the final results, and no disagreements were encountered.
RESULTS
A total of 38,569 patients were included. Sex distribution showed a majority of female patients [83.6%, n = 32,233, Male: n = 6336 (16.4)] within our cohort. Median age was 54 years (IQR 41-62), median BMI was 23.5 kg/m2 (IQR 21-26), white race had the highest race proportion (69.3%, n = 26,731), smoking status showed patients with a higher rate of never smoking (86.8%) and the majority of patients showed a low rate of systemic comorbidities (79.1%), as reflected by an ASA score of <2 (Table 1).
| Patient characteristics . | n (%) . |
|---|---|
| Female sex | 32,233 (83.6) |
| Age, median (IQR) | 54 (41-62) |
| BMI, median (IQR) | 23.5 (21-26) |
| White race | 26,731 (69.3) |
| Black race | 396 (1.0) |
| Asian race | 2496 (6.5) |
| Hispanic ethnicity | 1601 (4.2) |
| Current smoker | 844 (5.4) |
| Former smoker | 1201 (7.8) |
| Never smoker | 13,475 (86.8) |
| ASA ≥2 | 8057 (20.9) |
| Patient characteristics . | n (%) . |
|---|---|
| Female sex | 32,233 (83.6) |
| Age, median (IQR) | 54 (41-62) |
| BMI, median (IQR) | 23.5 (21-26) |
| White race | 26,731 (69.3) |
| Black race | 396 (1.0) |
| Asian race | 2496 (6.5) |
| Hispanic ethnicity | 1601 (4.2) |
| Current smoker | 844 (5.4) |
| Former smoker | 1201 (7.8) |
| Never smoker | 13,475 (86.8) |
| ASA ≥2 | 8057 (20.9) |
ASA, American Society of Anesthesiologists classification grade; IQR, interquartile range.
| Patient characteristics . | n (%) . |
|---|---|
| Female sex | 32,233 (83.6) |
| Age, median (IQR) | 54 (41-62) |
| BMI, median (IQR) | 23.5 (21-26) |
| White race | 26,731 (69.3) |
| Black race | 396 (1.0) |
| Asian race | 2496 (6.5) |
| Hispanic ethnicity | 1601 (4.2) |
| Current smoker | 844 (5.4) |
| Former smoker | 1201 (7.8) |
| Never smoker | 13,475 (86.8) |
| ASA ≥2 | 8057 (20.9) |
| Patient characteristics . | n (%) . |
|---|---|
| Female sex | 32,233 (83.6) |
| Age, median (IQR) | 54 (41-62) |
| BMI, median (IQR) | 23.5 (21-26) |
| White race | 26,731 (69.3) |
| Black race | 396 (1.0) |
| Asian race | 2496 (6.5) |
| Hispanic ethnicity | 1601 (4.2) |
| Current smoker | 844 (5.4) |
| Former smoker | 1201 (7.8) |
| Never smoker | 13,475 (86.8) |
| ASA ≥2 | 8057 (20.9) |
ASA, American Society of Anesthesiologists classification grade; IQR, interquartile range.
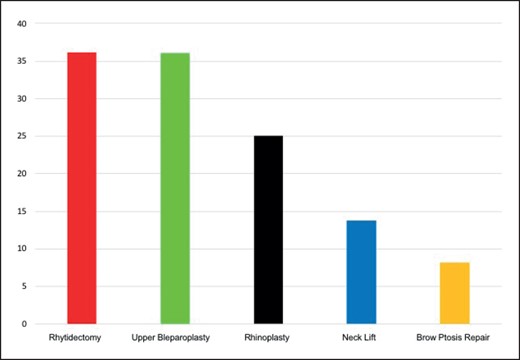
The most common procedures performed were rhytidectomy (grouped), upper blepharoplasty, primary rhinoplasty, neck lift, and brow ptosis repair; 13,943 (36.2%), 13,912 (36.1%), 9677 (25.1%), 5328 (13.8), and 3171 (8.2%), respectively (Figure 2). The detailed prevalence of all the procedures performed is provided in Table 2. Having at least 3 concomitant surgeries was seen in 18.4% of cases. The overall major complication rate was 1.2%. The procedures with the highest complication rates were canthoplasty (3.3%), blepharoptosis repair (2.4%), rhytidectomy (1.9%), and neck lift (1.9%) (Table 3). A final stepwise logistic regression model showed BMI ≥25, ASA score ≥2, over 3 concomitant procedures, current or former smoking status, and age ≥45 were independent risk factors for major complications (Table 4). Pearson's chi-squared and Hosmer-Lemeshow tests for goodness of fit resulted in P values of 0.77 and 0.16, respectively. Last, multiplying the regression coefficients (Table 4) by 2 and approximating the number to its closest integer was utilized to develop the risk score.
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 1281 (3.3) |
| Canthoplasty | 509 (1.3) |
| Blepharoptosis repair | 286 (0.7) |
| Brow ptosis repair | 3171 (8.2) |
| Rhytidectomy | 8535 (22.1) |
| Rhytidectomy deep plane | 6891 (17.9) |
| Otoplasty | 1207 (3.1) |
| Neck lift | 5328 (13.8) |
| Primary rhinoplasty | 9677 (25.1) |
| Revisional rhinoplasty | 1440 (3.7) |
| Submental lipectomy | 119 (0.3) |
| Upper blepharoplasty | 13,912 (36.1) |
| Lower blepharoplasty | 11,848 (30.7) |
| Over 3 procedures | 7095 (18.4) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 1281 (3.3) |
| Canthoplasty | 509 (1.3) |
| Blepharoptosis repair | 286 (0.7) |
| Brow ptosis repair | 3171 (8.2) |
| Rhytidectomy | 8535 (22.1) |
| Rhytidectomy deep plane | 6891 (17.9) |
| Otoplasty | 1207 (3.1) |
| Neck lift | 5328 (13.8) |
| Primary rhinoplasty | 9677 (25.1) |
| Revisional rhinoplasty | 1440 (3.7) |
| Submental lipectomy | 119 (0.3) |
| Upper blepharoplasty | 13,912 (36.1) |
| Lower blepharoplasty | 11,848 (30.7) |
| Over 3 procedures | 7095 (18.4) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 1281 (3.3) |
| Canthoplasty | 509 (1.3) |
| Blepharoptosis repair | 286 (0.7) |
| Brow ptosis repair | 3171 (8.2) |
| Rhytidectomy | 8535 (22.1) |
| Rhytidectomy deep plane | 6891 (17.9) |
| Otoplasty | 1207 (3.1) |
| Neck lift | 5328 (13.8) |
| Primary rhinoplasty | 9677 (25.1) |
| Revisional rhinoplasty | 1440 (3.7) |
| Submental lipectomy | 119 (0.3) |
| Upper blepharoplasty | 13,912 (36.1) |
| Lower blepharoplasty | 11,848 (30.7) |
| Over 3 procedures | 7095 (18.4) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 1281 (3.3) |
| Canthoplasty | 509 (1.3) |
| Blepharoptosis repair | 286 (0.7) |
| Brow ptosis repair | 3171 (8.2) |
| Rhytidectomy | 8535 (22.1) |
| Rhytidectomy deep plane | 6891 (17.9) |
| Otoplasty | 1207 (3.1) |
| Neck lift | 5328 (13.8) |
| Primary rhinoplasty | 9677 (25.1) |
| Revisional rhinoplasty | 1440 (3.7) |
| Submental lipectomy | 119 (0.3) |
| Upper blepharoplasty | 13,912 (36.1) |
| Lower blepharoplasty | 11,848 (30.7) |
| Over 3 procedures | 7095 (18.4) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 21 (1.6) |
| Canthoplasty | 17 (3.3) |
| Blepharoptosis repair | 7 (2.4) |
| Brow ptosis repair | 40 (1.3) |
| Rhytidectomy | 164 (1.9) |
| Rhytidectomy deep plane | 132 (1.9) |
| Otoplasty | 8 (0.7) |
| Neck lift | 101 (1.9) |
| Primary rhinoplasty | 50 (0.6) |
| Revisional rhinoplasty | 13 (0.9) |
| Submental lipectomy | 1 (0.8) |
| Upper blepharoplasty | 182 (1.3) |
| Lower blepharoplasty | 180 (1.5) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 21 (1.6) |
| Canthoplasty | 17 (3.3) |
| Blepharoptosis repair | 7 (2.4) |
| Brow ptosis repair | 40 (1.3) |
| Rhytidectomy | 164 (1.9) |
| Rhytidectomy deep plane | 132 (1.9) |
| Otoplasty | 8 (0.7) |
| Neck lift | 101 (1.9) |
| Primary rhinoplasty | 50 (0.6) |
| Revisional rhinoplasty | 13 (0.9) |
| Submental lipectomy | 1 (0.8) |
| Upper blepharoplasty | 182 (1.3) |
| Lower blepharoplasty | 180 (1.5) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 21 (1.6) |
| Canthoplasty | 17 (3.3) |
| Blepharoptosis repair | 7 (2.4) |
| Brow ptosis repair | 40 (1.3) |
| Rhytidectomy | 164 (1.9) |
| Rhytidectomy deep plane | 132 (1.9) |
| Otoplasty | 8 (0.7) |
| Neck lift | 101 (1.9) |
| Primary rhinoplasty | 50 (0.6) |
| Revisional rhinoplasty | 13 (0.9) |
| Submental lipectomy | 1 (0.8) |
| Upper blepharoplasty | 182 (1.3) |
| Lower blepharoplasty | 180 (1.5) |
| Procedure . | n (%) . |
|---|---|
| Genioplasty | 21 (1.6) |
| Canthoplasty | 17 (3.3) |
| Blepharoptosis repair | 7 (2.4) |
| Brow ptosis repair | 40 (1.3) |
| Rhytidectomy | 164 (1.9) |
| Rhytidectomy deep plane | 132 (1.9) |
| Otoplasty | 8 (0.7) |
| Neck lift | 101 (1.9) |
| Primary rhinoplasty | 50 (0.6) |
| Revisional rhinoplasty | 13 (0.9) |
| Submental lipectomy | 1 (0.8) |
| Upper blepharoplasty | 182 (1.3) |
| Lower blepharoplasty | 180 (1.5) |
| . | Coefficient . | (95% CI) . | P value . |
|---|---|---|---|
| Over 3 concomitant surgeries | 0.799 | 0.488-1.108 | <.001 |
| Overweight | 0.354 | 0.049-0.661 | .023 |
| ASA ≥2 | 0.525 | 0.217-0.834 | .001 |
| Current or former smoker | 0.336 | −0.017-0.691 | .063 |
| Age ≥45 | 0.501 | 0.057-0.945 | .027 |
| . | Coefficient . | (95% CI) . | P value . |
|---|---|---|---|
| Over 3 concomitant surgeries | 0.799 | 0.488-1.108 | <.001 |
| Overweight | 0.354 | 0.049-0.661 | .023 |
| ASA ≥2 | 0.525 | 0.217-0.834 | .001 |
| Current or former smoker | 0.336 | −0.017-0.691 | .063 |
| Age ≥45 | 0.501 | 0.057-0.945 | .027 |
CI, confidence interval.
| . | Coefficient . | (95% CI) . | P value . |
|---|---|---|---|
| Over 3 concomitant surgeries | 0.799 | 0.488-1.108 | <.001 |
| Overweight | 0.354 | 0.049-0.661 | .023 |
| ASA ≥2 | 0.525 | 0.217-0.834 | .001 |
| Current or former smoker | 0.336 | −0.017-0.691 | .063 |
| Age ≥45 | 0.501 | 0.057-0.945 | .027 |
| . | Coefficient . | (95% CI) . | P value . |
|---|---|---|---|
| Over 3 concomitant surgeries | 0.799 | 0.488-1.108 | <.001 |
| Overweight | 0.354 | 0.049-0.661 | .023 |
| ASA ≥2 | 0.525 | 0.217-0.834 | .001 |
| Current or former smoker | 0.336 | −0.017-0.691 | .063 |
| Age ≥45 | 0.501 | 0.057-0.945 | .027 |
CI, confidence interval.
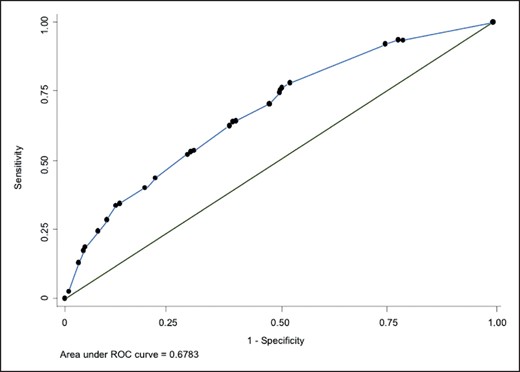
The risk score resulted in having ≥3 concurrent surgeries awarding 2 points, while BMI ≥25, ASA score ≥2, current or former smoking status, and age ≥45 each contributing 1 point (Table 5). The score would include these 5 variables resulting in a sum score ranging from 0 to 6. Area under the ROC curve resulted in 0.678 with a standard error of 0.013 (95% CI, 0.62-0.67) (Figure 3). Sensitivity analysis from this model showed at the cutoff value of ≥3, and there was a sensitivity of 57.6% and a specificity of 65.5%, correctly classifying 65% with a positive likelihood ratio (LR) of 1.67 and negative LR of 0.65 (Table 6).
| Variable . | Score . |
|---|---|
| Over 3 concomitant surgeries | 2 |
| Overweight | 1 |
| ASA class ≥2 | 1 |
| Current or former smoker | 1 |
| Age ≥45 | 1 |
| Variable . | Score . |
|---|---|
| Over 3 concomitant surgeries | 2 |
| Overweight | 1 |
| ASA class ≥2 | 1 |
| Current or former smoker | 1 |
| Age ≥45 | 1 |
| Variable . | Score . |
|---|---|
| Over 3 concomitant surgeries | 2 |
| Overweight | 1 |
| ASA class ≥2 | 1 |
| Current or former smoker | 1 |
| Age ≥45 | 1 |
| Variable . | Score . |
|---|---|
| Over 3 concomitant surgeries | 2 |
| Overweight | 1 |
| ASA class ≥2 | 1 |
| Current or former smoker | 1 |
| Age ≥45 | 1 |
| Cutoff point . | Sensitivity . | Specificity . | Correctly classified . | LR+ . | LR− . |
|---|---|---|---|---|---|
| (≥0) | 100.0% | 0.0% | 1.2% | 1 | |
| (≥1) | 89.1% | 23.9% | 24.7% | 1.17 | 0.46 |
| (≥2) | 86.1% | 28.0% | 28.7% | 1.19 | 0.50 |
| (≥3) | 57.6% | 65.5% | 65.4% | 1.67 | 0.65 |
| (≥4) | 23.5% | 89.9% | 89.1% | 2.32 | 0.85 |
| (≥5) | 9.1% | 97.6% | 96.6% | 3.87 | 0.93 |
| (≥6) | 0.9% | 99.7% | 98.5% | 3.07 | 0.99 |
| (>6) | 0.0% | 100.0% | 98.8% | 1 |
| Cutoff point . | Sensitivity . | Specificity . | Correctly classified . | LR+ . | LR− . |
|---|---|---|---|---|---|
| (≥0) | 100.0% | 0.0% | 1.2% | 1 | |
| (≥1) | 89.1% | 23.9% | 24.7% | 1.17 | 0.46 |
| (≥2) | 86.1% | 28.0% | 28.7% | 1.19 | 0.50 |
| (≥3) | 57.6% | 65.5% | 65.4% | 1.67 | 0.65 |
| (≥4) | 23.5% | 89.9% | 89.1% | 2.32 | 0.85 |
| (≥5) | 9.1% | 97.6% | 96.6% | 3.87 | 0.93 |
| (≥6) | 0.9% | 99.7% | 98.5% | 3.07 | 0.99 |
| (>6) | 0.0% | 100.0% | 98.8% | 1 |
LR, likelihood ratio.
| Cutoff point . | Sensitivity . | Specificity . | Correctly classified . | LR+ . | LR− . |
|---|---|---|---|---|---|
| (≥0) | 100.0% | 0.0% | 1.2% | 1 | |
| (≥1) | 89.1% | 23.9% | 24.7% | 1.17 | 0.46 |
| (≥2) | 86.1% | 28.0% | 28.7% | 1.19 | 0.50 |
| (≥3) | 57.6% | 65.5% | 65.4% | 1.67 | 0.65 |
| (≥4) | 23.5% | 89.9% | 89.1% | 2.32 | 0.85 |
| (≥5) | 9.1% | 97.6% | 96.6% | 3.87 | 0.93 |
| (≥6) | 0.9% | 99.7% | 98.5% | 3.07 | 0.99 |
| (>6) | 0.0% | 100.0% | 98.8% | 1 |
| Cutoff point . | Sensitivity . | Specificity . | Correctly classified . | LR+ . | LR− . |
|---|---|---|---|---|---|
| (≥0) | 100.0% | 0.0% | 1.2% | 1 | |
| (≥1) | 89.1% | 23.9% | 24.7% | 1.17 | 0.46 |
| (≥2) | 86.1% | 28.0% | 28.7% | 1.19 | 0.50 |
| (≥3) | 57.6% | 65.5% | 65.4% | 1.67 | 0.65 |
| (≥4) | 23.5% | 89.9% | 89.1% | 2.32 | 0.85 |
| (≥5) | 9.1% | 97.6% | 96.6% | 3.87 | 0.93 |
| (≥6) | 0.9% | 99.7% | 98.5% | 3.07 | 0.99 |
| (>6) | 0.0% | 100.0% | 98.8% | 1 |
LR, likelihood ratio.
DISCUSSION
The results from our study showed an overall morbidity rate of 1.2% for adults undergoing facial aesthetic surgery. The most common procedures performed were rhytidectomy, blepharoplasty, and rhinoplasty. Those with the highest morbidity rate were neck lift, canthoplasty, and face lift. The logistic regression model showed overweight, current or former smoking status, age ≥45, ASA score ≥2, and 3 or more concomitant surgeries to be independent risk factors for a major complication. This model is close to acceptable with an area under the ROC curve of 0.68. The Aesthetic Postoperative Complication Score (APeCS) ranges from 0 to 6, with each risk factor counting for 1 point except “3 or more concomitant surgeries” accounting for 2. Sensitivity analysis showed that a cutoff value of ≥3 was associated with correctly classifying 66% of those at risk for major morbidity. The highest morbidity rate for face and neck rejuvenation procedures has not been previously reported in the aesthetic surgical outcomes literature.
Fortunately, complications in facial aesthetic surgery are low and are specific to each individual procedure.10,18 However, as reported by Chopan et al, patients who undergo rhytidectomy undergo an average of 2.3 procedures at the same time and a total 76% of patients underwent combined procedures.10 This may increase overall major morbidity; however, this has not been deeply studied. In contrast to a previous TOPS analysis on rhytidectomy, in our study we found a lower morbidity of 1.8%, compared to 5.1%.10 This difference could be explained by the major morbidity definition in our study and exclusion of breast and body procedures. Breast and abdominal procedures alone have reported complication rates ranging from 5.3% to 70%.22-25 We believe this was an important exclusion criterion because aesthetic procedures of the chest and/or abdomen can overestimate complication rates of facial procedures when procedures are combined.26-28
Developing a risk assessment tool for adult patients choosing to undergo facial aesthetic procedures is an important and necessary addition to the plastic surgery literature. Managing expectations and communication with patients is an essential part of the preoperative process. The plastic surgeon and team's ability to communicate effectively with patients about risk profiles and complications is important to achieving better outcomes; a risk assessment tool can help with patient education and an understanding of the patient’s individual risk factors. An additional important point to consider is that malpractice litigations have increased in recent decades; blepharoplasties and rhinoplasties are the most litigated facial aesthetic procedures.29 This risk stratification tool can help plastic surgeons determine the risk for specific patients choosing to undergo single or multiple procedures at the same time; a patient with a higher APeCS score would be at higher risk for the surgery.
Risk factors as predictors for adverse surgical outcomes are ubiquitous in the literature, particularly those linking obesity and high ASA scores as predictors for poor outcomes.30-34 Patients with obesity have been found 1.62 times more likely to have complications, with the highest risk seen when undergoing cosmetic surgeries.34 A systematic review also found higher ASA scores as 1 of several risk factors associated with postoperative complications in head and neck free flaps.35 However, in facial and neck aesthetic surgery, this is the first study to identify these risk factors in addition to procedures that increase the likelihood of a major complication. With the development of the APeCS score, we intend to provide a useful clinical tool for plastic surgeons to risk stratify patients for single or multiple procedures.
This study was not exempt from limitations. These were mainly related to the retrospective design and lack of granularity in established variables by the database. Despite this study being a national representation, plastic surgeons who do not report their outcomes to TOPS can increase the risk of selection bias and may skew the results for a true national representation. Nevertheless, this is the largest cohort of isolated facial aesthetic surgeries to date that allows for adequate generalizability from our results. The statistical power from a national cohort has an impact on the internal validity due to lack of specific variables that are able to be retrieved from smaller cohort studies. However, we believe we accounted for many of the most important and reported risk factors for poor surgical outcomes. We believe we were able to identify the vast majority of these complications by assessing meticulously the “other complication” variable. Future directions should be focused on validating this risk score on a bigger cohort and in a prospective manner.
CONCLUSIONS
This national cohort study identified a major complication rate of 1.2% for patients undergoing a facial and neck aesthetic procedure. Despite the low morbidity rate, we developed an acceptable risk prediction score comprised of 5 variables. The cutoff value of ≥2 in the APeCS score was associated with correctly classifying approximately 65% of those at risk for major morbidity.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Drs Cataneo and Bartelt are general surgery residents, Advocate Illinois Masonic Medical Center, Department of Surgery, Chicago, IL, USA.
Ms Mathis is a medical student, University of Illinois at Chicago, College of Medicine, Rockford, IL, USA.
Dr Gelfond is a general surgery resident, Carle Health, Carle Illinois College of Medicine, Urbana, IL, USA.
Dr Arias-Serrato is an orthopedic and trauma surgery resident, Dresden International University, Dresden, Germany.
Dr Patel is a plastic surgeon, The University of Chicago Medicine and Biological Sciences, Division of Plastic and Reconstructive Surgery, Chicago, IL, USA.
Presented at: Midwestern Association of Plastic Surgeons meeting, June 2-5, 2021, Chicago, IL; and Plastic Surgery The Meeting, October 29-November 1, 2021, Boston, MA.



