-
PDF
- Split View
-
Views
-
Cite
Cite
Lennert Minelli, Cameron P Brown, Richard J Warren, Berend van der Lei, Bryan C Mendelson, J William Little, Lifting the Anterior Midcheek and Nasolabial Fold: Introduction to the Melo Fat Pad Anatomy and Its Role in Longevity and Recurrence, Aesthetic Surgery Journal, Volume 43, Issue 9, September 2023, Pages 941–954, https://doi.org/10.1093/asj/sjad126
Close - Share Icon Share
Abstract
A limitation of current facelift techniques is the early postoperative reappearance of anterior midcheek laxity associated with recurrence of the nasolabial fold (NLF).
This study was undertaken to examine the regional anatomy of the anterior midcheek and NLF with a focus on explaining the early recurrence phenomenon and to explore the possibility of alternative surgical methods that prolong NLF correction.
Fifty cadaver heads were studied (16 embalmed, 34 fresh; mean age, 75 years). Following preliminary dissections and macrosectioning, a series of standardized layered dissections were performed, complemented by histology, sheet plastination, and microcomputed tomography. Mechanical testing of the melo fat pad (MFP) and skin was performed to gain insight on which structure is responsible for transmission of the lifting tension in a composite facelift procedure.
Anatomic dissections, sheet plastination, and microcomputed tomography demonstrated the 3-dimensional architecture and borders of the MFP. Histology of a lifted midcheek demonstrated that a composite MFP lift causes a change in connective tissue organization from a hanging-down pattern into a pulled-upward pattern, suggesting traction on the skin. Mechanical testing confirmed that, in a composite lift, despite the sutures being placed directly into the deep aspect of the MFP, the lifting tension distal to the suture is transmitted through the skin and not through the MFP.
The usual method of performing a composite midcheek lift results in the skin, and not the MFP itself, bearing the load of the nondissected tissues distal to the lifting suture. For this reason, early recurrence of the NLF occurs following skin relaxation in the postoperative period. Accordingly, specific surgical procedures for remodeling the MFP should be explored, possibly in combination with volume restoration of the fat and bone, for more lasting improvement of the NLF.
Résumé
L’une des limites des techniques actuelles de lifting est la réapparition postopératoire précoce de la laxité du milieu antérieur de la joue, associée à la récurrence du sillon naso-génien.
Cette étude a été menée avec pour objectif l’examen de l’anatomie régionale du milieu antérieur de la joue et du sillon naso-génien afin d’expliquer le phénomène de récurrence précoce et de réfléchir à d’autres méthodes chirurgicales permettant de prolonger la correction du sillon naso-génien.
Cinquante têtes de cadavres ont été étudiées (16 embaumées, 34 fraîches; âge moyen, 75 ans). Suite aux dissections préliminaires et à la macrosection, une série de dissections par couches standardisées a été pratiquée, complétée par l’histologie, la plastination par tranche et la tomographie par microordinateur. Des tests mécaniques du coussinet adipeux de Melo et de la peau ont été réalisés pour comprendre quelle structure est responsable de la transmission de la tension de levage lors d’un lifting composite.
Les dissections anatomiques, la plastination par tranche et la tomographie par microordinateur ont démontré l’architecture tridimensionnelle et les limites du coussinet adipeux de Melo. L’histologie d’un lifting réalisé dans la zone médiane de la joue a montré qu’un lifting composite du coussinet adipeux de Melo entraîne un changement de l’organisation du tissu conjonctif, dont l’aspect change et semble tiré vers le haut au lieu d’être suspendu vers le bas, ce qui suggère une traction de la peau. Les tests mécaniques ont confirmé que, dans un lifting composite, bien que les sutures soient placées directement dans la partie profonde du coussinet adipeux de Melo, la tension de lifting distale à la suture est transmise à travers la peau et non à travers le coussinet adipeux de Melo.
La méthode habituelle de réalisation d’un lifting composite de la zone médiane de la joue fait que c’est la peau, et non le coussinet adipeux de Melo lui-même, qui supporte la charge des tissus non disséqués distaux par rapport à la suture de lifting. C’est pour cette raison qu’une récidive précoce du sillon naso-génien se produit après le relâchement de la peau au cours de la période postopératoire. Par conséquent, il convient d’étudier des procédures chirurgicales spécifiques pour remodeler le coussinet adipeux de Melo, si possible en association avec une restauration du volume de la graisse et de l’os, afin d’obtenir une amélioration plus durable du sillon naso-génien.
“With this procedure, the surgeon has become more a sculptor of tissues: the surgeon artist.”—Bryan C. Mendelson, invited commentary on “Three-dimensional Rejuvenation of the Midface: Volumetric Resculpture by Malar Imbrication” by J. William Little, Plastic & Reconstructive Surgery (2000)1
The cheek, “melo,” is a key area in facial aging, often displaying such early signs as fullness of the nasolabial fold (NLF) and downturned corners of the mouth (Figure 1).2 These features contribute to an unaesthetic facial appearance and convey negative feelings, such as sadness, which may not correspond to the patient's true condition. Facelifts attempt to improve these visible aging changes. However, a limitation of most facelift techniques is the early postoperative reappearance of anterior midcheek laxity associated with recurrence of the NLF (Figure 2). Despite its clinical importance, the reason for early recurrence of the NLF after facelift surgery has not been adequately explained. This study was undertaken to examine the anatomy of the anterior midcheek, melo fat pad (MFP), and NLF with a focus on explaining the early NLF recurrence phenomenon, and to explore the possibility of alternative surgical methods prolonging the benefit of NLF correction.
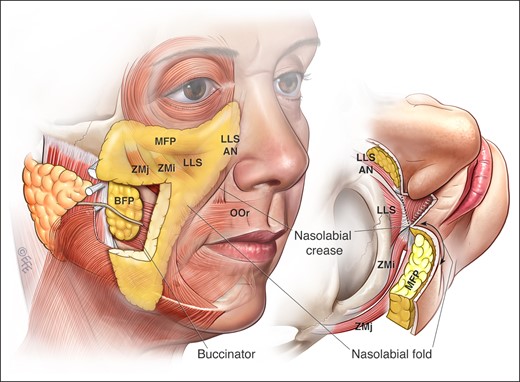
The MFP, shown from (left) a right oblique view and (right) a superior view, is a localized triangular-shaped area of increased thickness of the subcutaneous panniculus adiposus in the midcheek. Its medial extent is marked by the nasofacial groove, nasolabial crease, and labiomandibular crease; its lateral extent largely relates to the anterior border of the masseter, although this border is less distinct. The MFP overlies the upper lip levator muscles above the oral commissure, the buccinator muscle and modiolus at the level of the oral commissure, and the risorius, platysma, and depressor anguli oris muscles below the oral commissure. The jowl is formed by the lowest part of the MFP. The nasolabial fold and labiomandibular fold are the parts of the MFP that border and partially overhang the perioral adhesion zone. There is a difference between the nasolabial fold (hanging fullness), and the nasolabial crease (sharp depression). In youth the MFP extends well over the orbital rim into the lower lid up infratarsal crease. However, in the middle-aged and elderly, the MFP over the orbicularis oculi muscle deflates, with its upper edge becoming the tear-trough and palpebromalar groove. LLSAN, levator labii superioris alaeque nasi; BFP, buccal fat pad; OOr, orbicularis oris muscle; ZMi, zygomaticus minor muscle; ZMa, zygomaticus major muscle. Created by and published with permission from Dr Levent Efe, CMI.

A 62-year-old female patient (A) before and (B) 6 months after a traditional deep-plane facelift and lip lift without anterior melo fat pad sutures or addition of volume (no lipofilling or hydroxyapatite). Note the improved lid cheek junction with improved malar highlight, as well as the jawline, jowl, and neck improvement, whereas the nasolabial fold remains essentially uncorrected. Courtesy of Dr Anh Nguyen of Perth, Australia.
METHODS
Ethical approval for the project was granted by the Human Ethics Advisory Groups of the University of Melbourne for the feasibility study, the Queensland University of Technology for the conclusive study including histology and plastination, and the Yonsei University College of Medicine for the microcomputed tomography (micro-CT) study (project numbers 14243, LR2021-4306-4761, and YSAEC22-004). The authors state that every effort was made to follow all local and international ethics guidelines and laws that pertain to the use of human cadaveric donors in anatomic research. The study was conducted between June 2020 and May 2022.
A feasibility study was performed on a group of 15 embalmed and 6 fresh frozen cadavers (male, 10; female, 11; mean age, 76 years [range, 45-96 years]) to learn how to effectively study this area of complex anatomy. This involved layered dissections, facelift dissections, and macrosectioning in various planes. Based on this preliminary study, a definitive study was conducted on 27 cadavers. Standardized dissections were performed on 16 cadavers, 1 embalmed and 15 fresh (nonfrozen) (male, 9; female, 7; mean age, 78 years [range, 45-97 years]; BMI, 26 kg/m2 [range, 17-33 kg/m2]). On the first side of the face, the effect of a deep-plane facelift through the prezygomatic space performed by a recognized technique was investigated, focusing on the presence of skin tension.3 On 3 cadavers, a subdermal dissection and MFP plication, as described by Little, was performed.1
On the contralateral side, a dissection immediately deep to the subcutaneous layer was performed (ie, directly on the surface of the flat mimetic muscles and lip levators) to harvest a composite flap (skin and MFP) for subsequent mechanical testing. These fresh (nonfrozen) samples were then frozen by submersion into liquid nitrogen and stored in a −80°C freezer. Mechanical testing of the MFP sample, first with the skin attached and then repeated with the skin removed, was performed on all fresh samples after thawing. To this end, each sample was suspended in a mechanical testing device (Micro Tester 5848 with 100-N load cell; Instron, Norwood, MA) between 2 points: from the deep aspect of the MFP at the level of where a deep-plane MFP lift would be performed, and from the inferomedial-most NLF. At each side, the force was distributed equally by means of a running suture fixing the ends of the tissue to the testing device. Samples were extended at a constant strain rate of 2.50 mm/s to a maximum load of 12 N, recording tension and extension data at 100 Hz. A 12-N load was used because this had previously been demonstrated to be the maximum load at which the superficial musculoaponeurotic system (SMAS) can be sutured,4,5 as well as being the load at which the anterior SMAS tends to burst.6 The stiffness of the samples was calculated for the load range of 8 to 12 N.
Finally, objective technical investigations were used to complement the dissection findings:
Sheet plastination of the head and neck of 10 fresh cadavers processed by von Hagens Plastination in the axial, sagittal, and coronal planes according to their latest technique (male, 4; female, 6; mean age, 67 years).7
Histology of full-thickness macrosections of the malar region were studied in 6 hemifaces of 3 cadavers (mean age, 84 years).8 In 2 of these, the effects of surgical lifting of the MFP through a deep-plane prezygomatic approach was studied on the one side while comparing it to the normal anatomy on the contralateral side.
High-resolution micro-CT of the malar area was performed on 1 cadaver (male, 67 years) to confirm the anatomy in a 3-dimensional way.9
RESULTS
Surgical Anatomy of the Midcheek
A key entity in the midcheek is a locally thicker subcutaneous fat layer in the mobile area of the face, overlying the mimetic muscles, the MFP. Unlike in Owsley's original description of the malar fat pad, which did not extend further laterally or inferiorly than the zygomaticus major muscle (ZMa), we have observed that this locally increased thickness of the fat has an inferior extension, which continues over the anterior buccinator, modiolus, depressor anguli oris (DAO), and upper platysma into the jowl (Figure 1).10 The fat pad effectively spans the entire cheek, hence the logical name change to “melo” fat pad, as distinct from the original “malar” fat pad, which specifically refers to the layer only in relation to the malar bone (zygoma). A dense network of retinacula cutis (RC) superficialis, which Owsley called “fibroelastic septa,” provides the structural framework of the MFP, which contains the fat lobules in a honeycomb-like arrangement through which the skin is retained to the deeper structures, as demonstrated with histology, sheet plastination, and micro-CT (Figure 3). These septa run from the mimetic muscles (upper lip levators, buccinator, DAO, platysma), or from the fascia in between these muscles, to the skin. This organization perpendicular to the skin distinguishes the MFP (as a subcutaneous structure) from the deep fat, in which the connective tissue is oriented essentially parallel to the skin surface. In a standing position, these RC are largely arranged in an obliquely hanging-down direction. Distinct superficial fat compartments, as described by Rohrich and Pessa, were not identified macroscopically or microscopically.11
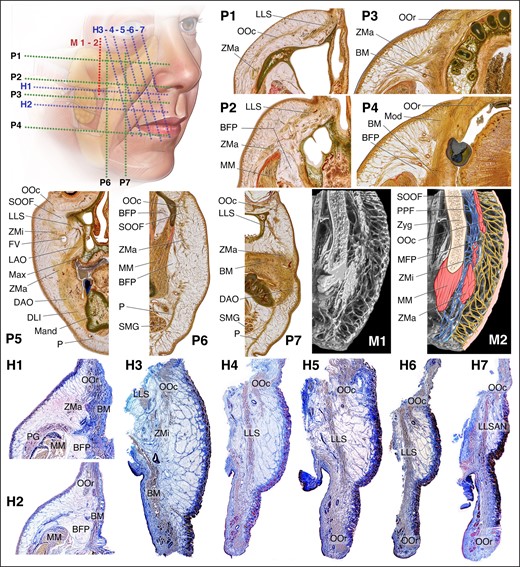
Microscopic studies of the face. Sheet plastination cross sections of the midcheek in the axial plane (P1-P4), the coronal plane (P5), and the sagittal plane (P6-P7). Microcomputed tomography in a vertical plane perpendicular to the skin (M1-M2). Histology in the axial plane (H1-H2) and in the plane parallel to the ZMa and perpendicular to the skin (H3-H7). The MFP marks the localized increased volume of the subcutaneous fat. The retinacula cutis provide structural architecture to this subcutaneous entity in a consistent arrangement, essentially perpendicular to the skin. LLS, levator labii superioris; OOc, orbicularis oculi muscle; ZMa, zygomaticus major muscle; OOr, orbicularis oris muscle; BM, buccinator muscle; BFP, buccal fat pad; MM, masseter muscle; Mod, modiolus; SOOF, sub-orbicularis oculi fat; ZMi, zygomaticus minor; FV, facial vein; LAO, levator anguli oris; Max, maxilla; DAO, depressor anguli oris; DLI, depressor labii inferioris; M and, mandible; P, platysma; SMG, submandibular gland; PPF, pre-periosteal fat; Zyg, zygoma; MFP, melo fat pad; PG, parotid gland; LLSAN, levator labii superioris alaeque nasi.
Surgical Manipulation of the Nasolabial Fold
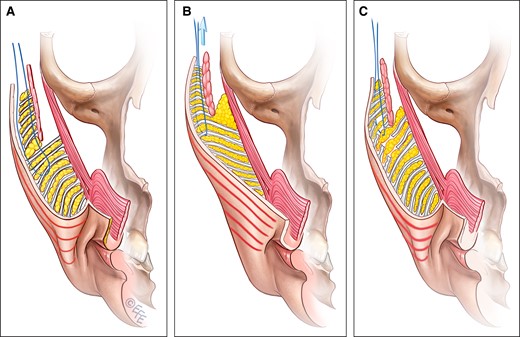
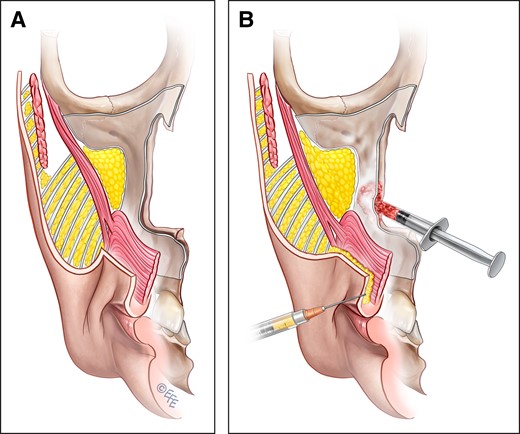
The NLF can be targeted through a subdermal dissection, with plication of the MFP or alternatively by a deep-plane/composite dissection with en-bloc lifting of the MFP. A true deep-plane approach to the midcheek is performed deep to the orbicularis oculi muscle (OOc) through the prezygomatic space. Some surgeons prefer a dissection in this area on the superficial surface of orbicularis, ie, deep to the subcutaneous layer. Either way, beyond the boundaries of the OOc and dissecting medially from the lateral border of the ZMa, the dissection is always performed in the deep subcutaneous plane, not a sub-SMAS plane, to avoid damaging the zygomatic and buccal branches of the facial nerve which run on the deep aspect of the ZMa. The upper portion of the MFP is raised as a composite flap, and the zygomatic cutaneous ligaments (ZCLs) are released. The midcheek lift is maintained by sutures placed within the deep portion of the MFP in a vector parallel to the ZMa (Video 1).3 Microscopy investigations demonstrated that despite the sutures being placed deep, the lift of the lower portion of the MFP, including the NLF, is achieved through skin tension rather than tension mediated through the MFP itself (Figure 4). This is demonstrated by the change of the direction of the RC in the lower portion of the MFP from a downward orientation in which these fibers support the skin, to an upward-pulled direction in which the skin supports, or rather pulls, the RC (Figure 4C).
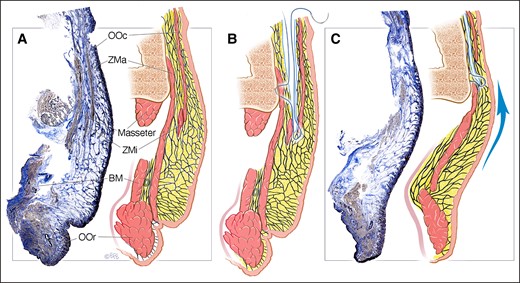
Histology, with accompanying illustration, demonstrating the mechanical effect of lifting the MFP and NLF through a deep-plane approach. (A) Preoperative situation of an aged midcheek showing the ptotic MFP and NLF. (B) Illustration of the procedure performed through the prezygomatic space, deep to the OOc but over the ZMa and ZMi with the suture bite deep within the MFP. (C) Immediate result after the MFP lift, demonstrating not only an adequate effacing of the NLF, but also a change in the orientation of the retinacula cutis from a hanging-down pattern into an upward-pulled pattern. This can only be explained by traction by the suture being transmitted to the skin, not through the MFP itself. BM, buccinator muscle; MFP, melo fat pad; NLF, nasolabial fold; OOc, orbicularis oculi muscle; OOr, orbicularis oris muscle; ZMa, zygomaticus major muscle; ZMi, zygomaticus minor muscle. Created by and published with permission from Dr Levent Efe, CMI.
An alternative is to target the NLF through a subdermal approach with MFP plication, ie, dissecting over the MFP, which is technically easier, although vascularity of this thin flap is a risk. Separating the skin from the MFP allows the full length of the MFP to be used (see below). Simple plication sutures of the MFP lift the lower part onto the upper part, which reduces the surface area, while the projection is increased (Video 2). In theory, this plication reverses the teardrop-shaped MFP, restoring fullness to the middle portion while reducing the fullness of the NLF without putting tension on the skin, as it is redraped over the fat plication without taking any of the tension.
Mechanical Testing of the Melo Fat Pad
The stiffness, given by the steepness of the slope of the load-displacement curves in Figure 5, of the skin-MFP composite is a nearly double that of the isolated MFP (mean [standard deviation], 197% [37%]) in the “linear” high-load region. This difference in stiffness, however, is dwarfed by the large difference in the “low-resistance region” between the skin-MFP composite vs the isolated MFP, as indicated by the region of extension for which little resistive force is measured, prior to stiffness increasing up to a linear region above 8 N. Based on a low load threshold of 0.1 N defining a large portion of this low-resistance region, an isolated MFP allows a mean of 5 [1.8] times (range, 2.8-8.1 times) more extension than the same MFP with the skin still attached. At a maximal facelift load of 12 N, an isolated MFP extends a mean of 2 [0.2] times (range, 1.8-2.4 times) more than the same MFP with the skin still attached, an effect dominated by this low-resistance region, and not the difference in stiffness.
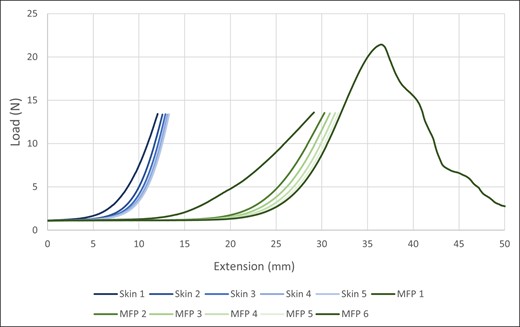
Plot demonstrating the resistance to extension of a typical midcheek sample suspended between the superolateral MFP at the inferior border of the prezygomatic space, and the nasolabial crease. The y axis shows the load and the x axis shows the extension in millimeters. First, 5 repeated loads were performed on the MFP with the skin attached (Skin 1-5), and then on the MFP with the skin removed (MFP 1-5). A final maximal loading was always performed to study the breaking force of the MFP (MFP 6). This test demonstrated how the skin is less deformable, at least in the short term, than the MFP. The first five loads (Skin 1-5) show mostly skin tension with a minor contribution of the retinacula cutis from the suture to the skin. The result of this test demonstrates that a lift through sutures placed into the MFP is transferred through the skin, and not through the MFP itself. With the skin attached, a 10-mm lift of the suture results in approximately a 10-mm lift at the end of the nasolabial fold by a near-linear transmission through the skin, whereas after removal of the skin from the equation, the suture needs to be lifted by approximately 30 mm to gain the same 10-mm lift at the nasolabial fold due to the stretching of the MFP. MFP, melo fat pad.
In absolute distances, this translates to an average of 5.8 [1.3] mm (range, 4.6-7.8 mm) extra extension of an isolated MFP over a skin-MFP composite at a minimal 0.1-N load, increasing to an average of 12.5 [4.4] mm (range, 6.7-18.7 mm) extra extension at a maximum 12-N load. This “extra” length of the MFP is used in plication-type surgical procedures (see above).
In more clinically relevant terms, a 10-mm extension (lift) puts almost no load on the MFP while the load on the skin is already approaching maximum capacity. The conclusion is that when lifting the upper part of the MFP with 10 mm with notable lifting on the NLF, the rest of the MFP is still stretching passively while the overlying skin is already approaching maximal stress and hence taking all the load responsible for this lift of the NLF.
DISCUSSION
The dissections, sheet plastination, histology, micro-CT, and mechanical testing of this study demonstrated the true nature of the NLF and its early recurrence after facelift surgery: distal to the placed suture within the MFP, it is the skin, and not the MFP, that transfers the tension to the NLF, and for that reason early recurrence of the NLF occurs.
Aging of the Midcheek
The midcheek ages in a very particular manner with transformation of the round, plump fullness of a youthful MFP into a teardrop-shaped, ptotic entity creating the NLF (Figure 6). Based on the presented anatomic findings and previously published literature, several anatomic changes must occur simultaneously to produce the stigmata of the aged midcheek:
The position of the nasolabial crease (NLC) remains essentially fixed throughout the lifetime, and is maintained by the resting tone of the upper lip levator muscles which firmly attach the skin at the location of the NLC and modiolus. An early MRI study concluded that the NLF develops without appreciable change in the muscle plane.12 Only in the case of facial palsy, and in contrast to normal aging, do the NLC and muscular modiolus truly descend. The depth of the NLC becomes exaggerated with aging by 2 primary pathways: (1) bone resorption of the maxilla causing a posterior displacement of the overlying soft tissues; and (2) fat deflation and muscle atrophy in the perioral region causing up to 40% decrease in soft tissue thickness.13 This principle of NLC deepening was eloquently demonstrated recently by Lambros.14
The aging MFP hangs over this fixed NLC, creating the bulge of the NLF and affecting the skin and subcutis of the modiolus, similar to what is seen in temporal hooding. Owsley proposed that the MFP slides down and forward superficial to the levator muscles to produce the palpebromalar groove superiorly and the NLF inferiorly.10,15 However, based on the presence of RC on histology and micro-CT, it is clear that the MFP cannot simply glide down. Instead, the 2 components making up the MFP, subcutaneous fat and RC, undergo specific aging changes and it is the combination of both that causes the resulting fold:
The RC fibers, which support the overlying skin and create a matrix for the fat, lose elasticity and elongate with aging. It is unclear which comes first: skin redundancy or RC redundancy. It is, however, clear that the 2 are always interrelated as the skin is entirely supported by the RC.
The subcutaneous fat acts as a filler, keeping the structural matrix of the MFP distended. Hence, it only has the capacity to increase or decrease (ie, inflate or deflate). In aging, the subcutaneous fat volume generally decreases in a process called fat deflation.16 Especially superiorly, around the lower lid, the subcutaneous fat between the OOc and the skin undergoes significant deflation, probably related to the repetitive closure of the eyes. Near-total deflation of the MFP over the orbital portion of the OOc causes the lid-cheek junction to disappear, which marks the upper extent of the MFP in youth, and the tear-trough and palpebromalar groove to appear, which marks the upper extent of the MFP in the elderly.17 The net result of MFP deflation for the midcheek is that the structural matrix of skin and RC will be relatively oversized. In young and healthy individuals, the skin and RC have some ability to contract after volume decrease (ie, weight loss). With aging, however, diminished elasticity of the connective tissue will result in redundant length of the RC and ptosis of the MFP-skin complex because the amount of fat required to keep the entity inflated is lacking. Effectively, the MFP of youth with fullness over the zygoma becomes a teardrop-shaped fat pad, thinned at the superior border and thicker at the inferior border along the NLF. This explains how weight loss in adulthood often results in an aged appearance of the face, whereas gaining weight in the face often has a rejuvenating effect in the short term. It also explains the apparent lifting effect of lipofilling or fillers.
The malar fat pad, of course, remains an important component within the more extensive MFP, but not as important in aging as the submalar, central facial, and lower facial components.18
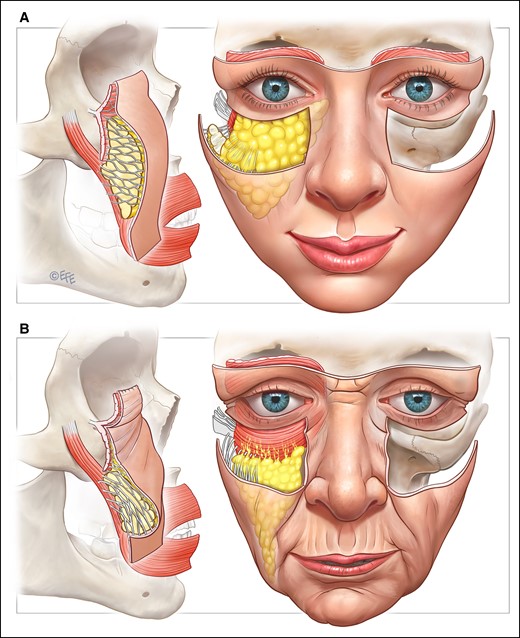
The typical aging pattern of the midcheek. In general, deflation of the MFP with elongation of the retinacula cutis adds to the redundancy of soft tissues causing the nasolabial fold. Near-total deflation of the MFP over the orbicularis oculi muscle causes the infratarsal crease to disappear, marking the upper extent of the MFP in youth, and the tear-trough and palpebromalar groove to form, marking the upper extent of the MFP with aging. The MFP becomes teardrop-shaped, with fat accumulation above the nasolabial crease. Resorption of the anterior maxilla and deep fat deflation contributes to the flattening of the midcheek. There is no evidence for zygomaticus major muscle elongation/stretch, with the zygomaticus major muscle maintaining the position of the nasolabial crease. MFP, melo fat pad. Created by and published with permission from Dr Levent Efe, CMI.
Mechanism of Action and Limitations of Traditional Techniques for NLF Correction
Skin-only facelifts, with or without plication of the subcutaneous tissues, which some authors later called the “SMAS,” were demonstrated early on to be ineffective for treating the NLF.19 Even deep-plane techniques, originally described by Skoog in 1974 and further refined by Hamra in 1986, were demonstrated to be largely ineffective in treating the NLF.20,21 In 1987, Millard et al noted that lifting the SMAS does not alter the NLF significantly, and observed that the lip levator muscles insert at the NLC with the NLF sitting just lateral/superior to it.22 Tensioning the muscle layer (SMAS) simply lifts the NLC and NLF upward without effacing it, an effect that was observed in the short term but not in the long term due to relaxation and stretching of the mimetic muscles postoperatively.23,24 The recently demonstrated absence of a musculoaponeurotic layer in the midcheek should additionally persuade surgeons away from the notion that the flap can rely on the strength of the “SMAS” to hold up the anterior tissues.25
The MFP was first described and introduced as the “malar fat pad” by Owsley in 1993 and proposed to function as a protective layer over the underlying thin-walled maxillary sinus.10 The hypothesis was that the MFP “slides down” with aging, and hence could be lifted en bloc over the lip levators without having to extensively release it (Figure 7A). In 1995, Mendelson published a technique for more anteriorly placed sutures to suspend the MFP en bloc with the same conviction that the MFP could glide over the lip levators (Figure 7B).26 In more mechanical terms, this idea implied that lifting sutures in the MFP layer would result in tension being transmitted through the MFP, passively carrying the overlying skin along (Figure 7C). However, the different investigations done in this study have conclusively demonstrated that the exact opposite occurs: a lift obtained by traction on the MFP, even through a deep-plane approach, is achieved by tension transmitted through the skin, not through the MFP as was previously assumed (Figure 7D). The realization that corrections of the NLF by conventional lifting techniques are depending on skin tension, which is known to stretch, explains why this lifting technique is not long lasting. In a deep-plane facelift, the dissected (undermined) part of the flap will therefore retain long-lasting results because postoperative healing causes a reattachment of the released composite flap to the deeper tissues, after which the sutures will become redundant.27 The nonreleased anterior tissues, however, rely on skin tension and will relapse (Figure 7E). This understanding explains the typical stigmata of composite midcheek lifting marked by a high and lateral cheek volume with good periorbital rejuvenation, but with a stretched MFP, flat anterior cheek, and recurrent NLFs, especially in absence of fat grafting, skeletal augmentation, or after a secondary facelift. To minimize this reliance on skin, an option would be to do a more extensive dissection over the lip levator muscles up to the NLC and place the sutures closer to the NLF. It is important in this extensive type of release to conduct the dissection from superiorly over the zygomatic body, not from laterally over the masseter, to prevent injury to the buccal branches that will be exposed superficially until they pass below the lip levator muscles.28
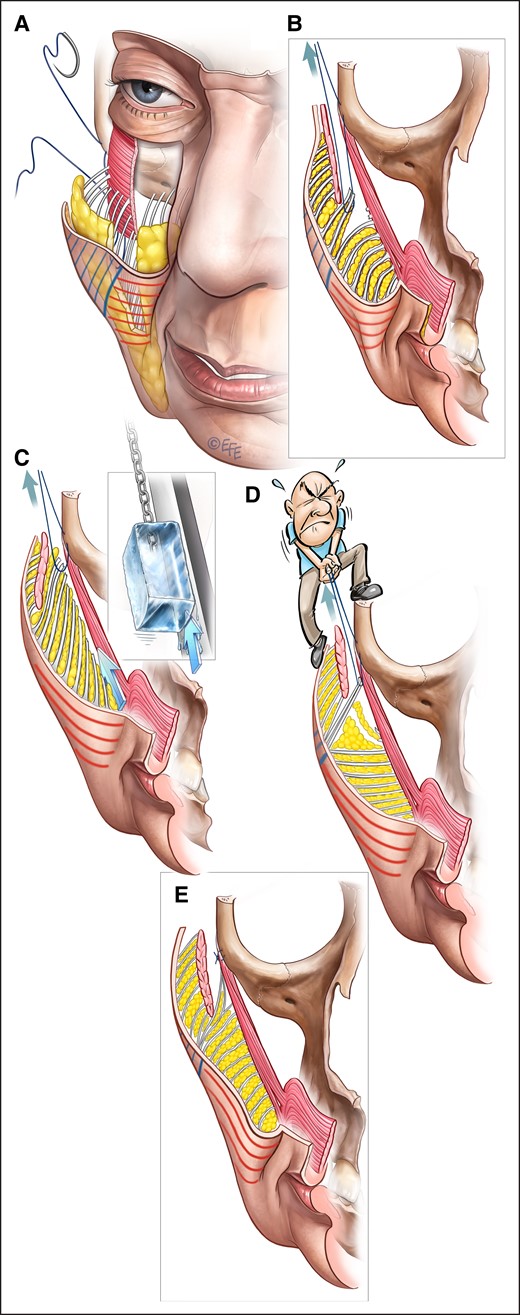
Mechanism of action of a deep-plane facelift with composite flap of the cheek, with the skin and MFP, in this case through a prezygomatic space dissection extending over the origin of the zygomaticus major and minor muscles. The undermined part is indicated by blue lines on the skin, while the part not undermined is indicated by red lines. (A, B) Sutures are placed in the deep aspect of the MFP at the most anterior-inferior extent of the dissection, to suspend the fat pad to the periosteum of the zygoma. (C) It is often assumed that the MFP slides en bloc over the underlying mimetic muscles with aging and can hence be lifted using the same sliding principle.1 (D) However, the mechanical testing and histology demonstrated that the nonreleased part of the MFP (ie, the part distal to the suture) is held up by the skin tension rather than tension conducted through the MFP. This distal skin–mediated lift results in a change of the architectural organization of the nonreleased part of the MFP from a gravity-opposing “hanging-down” organization to a “pulled-up” organization which does not oppose gravitational pull (Figure 4C). As a result, the entire flap distal to the placed suture, including the MFP and upper lip, are effectively suspended by the skin tension. (E) Following the surgery, the released and suspended superolateral cheek volume remains high and lateral, contributing to the periorbital fullness for the long term, whereas over the nonreleased part of the cheek the skin relaxation process will continue without the gravity-opposing retinacula cutis until relapse occurs, effectively undoing the initial result and causing recurrence of the NLF. The end result is a retained high and lateral position of the dissected MFP, which was brought onto the zygoma, and a flattening of the midcheek due to stretching of the skin and MFP with the volume being distributed over a larger area than preoperatively. MFP, melo fat pad. Created by and published with permission from Dr Levent Efe, CMI.
Many of the facelift procedures involve no release of the MFP off the underlying muscles, such as lateral SMAS-plication, SMASectomy, S-lift, minimal access cranial suspension technique (MACS)-lift, and thread lifts.19,29-32 Lifting the MFP through a subdermal dissection over the MFP was proposed by Vasconez and co-workers in 1996 and by Barton and Kenkel in 1997.33,34 In these techniques, no form of postoperative healing will result in a stable lifted situation: the sutures and the skin tension remain the only reason why the lift is maintained. Once the sutures cheesewire or the skin stretches, the effect is largely lost (Figure 8).
No-release facelifts, in which the anterior midcheek is being lifted without being first undermined (eg, SMAS-plication, SMASectomy, S-lift, MACS lift, PRS-lift, thread lift), do not result in a stable healed situation. (A) In this illustration, the third MACS-lift suture placed through a superficial subcutaneous dissection is demonstrated. (B) The normal gravity-opposing hanging-down pattern of the retinacula cutis is changed to a pulled-up pattern in which the entire weight of the flap is supported by the sutures and the skin tension. (C) Skin relaxation and weakening of the fixation (a process sometimes referred to as “cheesewiring’) contributes to recurrence of the nasolabial fold. MACS, minimal access cranial suspension technique; SMAS, superficial musculoaponeurotic system. Created by and published with permission from Dr Levent Efe, CMI.
As an alternative to lifting the MFP en-bloc, superficial plication of the MFP was proposed by Little to reshape the cheek fat with a wide surface area to a more compact/plump fat pad with a smaller surface area (Figure 9).1 In contrast to the en-bloc lifting, localized plication of the MFP with nontension sutures causes the fat pad to become reshaped without the requirement for sutures being responsible for holding up a heavy flap (Video 3). This technique may therefore have longer-lasting results on the NLF (Supplemental Figure 1). However, the lack of lifting the superior part of the MFP usually requires lipofilling to address infraorbital hollowing. Other authors have since described similar techniques utilizing anterior MFP plication sutures.35-37
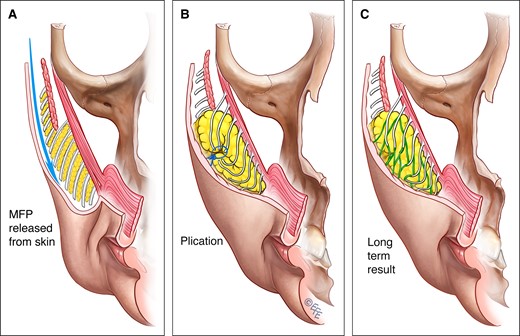
MFP plication, as introduced by Little, involves (A) releasing the MFP from the skin then (B) a no-tension plication to reduce the surface area and increase the projection of the MFP. In the process, the lowest part of the MFP and jowl is lifted to a higher position without tension being placed on the skin and underlying muscles. (C) Healing, with fat remodeling, is proposed to explain the long-term increased plumpness of the MFP. Note how this technique does not by itself improve periorbital hollowness as does the deep-plane composite lift of the released MFP en bloc onto the zygoma. MFP, melo fat pad. Created by and published with permission from Dr Levent Efe, CMI.
Alongside lifting and plication procedures, effacing the NLF has been attempted by NLF volume reduction and NLC volumizing procedures. Early on, Millard et al recommended direct lipectomy by resecting the NLF fat from superficially through a subdermal dissection, whereas Ellenbogen et al used curettage of the NLF fat from deep through a deep subcutaneous dissection.22,38 Direct liposuction of the NLF fat was described by McKinney and Cook in 1989.39 On the other side of the spectrum, augmentation of the NLC was utilized by volumizing the soft tissues or the bone (Figure 10). Ranging from local de-epithelialized skin rolled up onto itself,40 to autogenous tissue grafts (dermal, subcutaneous, aponeurotic/galeal, SMAS, etc),41,42 GoreTex (W. L. Gore & Associates, Newark, DE),43,44 and finally autologous fat grafting45 were described. Today, soft tissue fillers (hyaluronic acid, calcium hydroxyapatite, etc) and lipofilling are commonly used to add volume to creased soft tissues. Bony augmentation of the maxilla with implants,46 and more recently with the use of subperiosteal hydroxyapatite granule implantation,47 have been used to correct congenital hypoplasia and age-related bone shrinkage with good, long-lasting effects on the NLC (Supplemental Figure 2).
(A) Volume deflation, due to remodeling of the anterior face of the maxilla and fat deflation, adds to the depth of the nasolabial crease, accentuating the nasolabial fold. (B) Volume augmentation can be used to improve the nasolabial crease, using either hydroxyapatite to restore the bone projection of the underlying maxilla or increasing the soft-tissue volume of the nasolabial crease and the upper lip area by lipofilling or commercial fillers. Created by and published with permission from Dr Levent Efe, CMI.
Limitations
In vitro studies can only provide information on the natural architecture of the tissues and immediate implications of surgical manipulation, not the long-term effects required to empirically prove longevity in regenerating and moving living tissues. All deductions on longevity were limited to the change of the soft tissue architecture visualized, which are not consistent with their normal antigravitational function. Microscopic studies comparing a younger cohort with an older cohort could provide more conclusive evidence on aging of the midcheek and rejuvenation options.
CONCLUSIONS
Our study clearly demonstrated the true nature of the NLF as a deflated and ptotic MFP hanging over a receded NLC. In a composite midcheek lift, it is the skin and not the MFP that bears the load of the lifted tissues distal to the placed sutures. For this reason, early recurrence of the NLF occurs. Accordingly, in a composite midcheek lift, the suture in the MFP should be placed close to the NLF to minimize the length of tension-transmitting skin. Alternatively, specific surgical procedures for remodeling the MFP can be used, such as anterior MFP plication. In all cases, volume restoration of the deflated soft tissues and receded maxilla should be considered for more lasting improvement of the NLF.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Acknowledgments
The authors acknowledge the donors and families of the Body Donor Programs of the University of Melbourne and the Queensland University of Technology who have made this study possible. Specific thanks to Associate Professor Quentin Fogg from the University of Melbourne and Mr Matt Wissemann and Mr Ian Mellor of the Medical Engineering Research Facility for their assistance in the laboratory. The authors thank Dr Tae-Hyeon Cho and Professor Hun-Mu Yang of the Department of Anatomy of the Yonsei University College of Medicine for providing high-resolution micro-CT scans. Also, Ms Erica Mu and Dr Darryl Whitehead from the School of Biomedical Sciences of The University of Queensland, Ms Tania Henderson and Ms Felicity Lawrence from the CARF Histology Laboratory at the Queensland University of Technology and Mr Rory Bown for providing the pristine histology outcomes. The authors are grateful for the help of Dr Vladimir Chereminskiy and Mrs Daniela Albinus from von Hagens Plastination for providing high-quality sheet plastination slices. Special thanks to the international authorities Dr T. Gerald O’Daniel, Dr Mario Pelle-Ceravolo, and Dr James C. Grotting, as well as our local Mendelson Advanced Facial Anatomy Course faculty members Dr Chin-Ho Wong, Dr Andres Freschi, Dr Peter Callan, and Dr Darryl Hodgkinson for their thorough review of the manuscript.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
Author notes
Dr Minelli is the Tagliacozzi research fellow, Mendelson Advanced Facial Anatomy Course, Australasian Society of Aesthetic Plastic Surgeons, Toorak, Australia.
Dr Mendelson is a plastic surgeon, Mendelson Advanced Facial Anatomy Course, Australasian Society of Aesthetic Plastic Surgeons, Toorak, Australia.
Dr Brown is a professor, Medical Engineering Research Facility, Queensland University of Technology, Brisbane, Australia.
Dr Warren is a plastic surgeon, University of British Columbia and Vancouver Plastic Surgery Center, Vancouver, British Columbia, Canada.
Dr van der Lei is a professor, Department of Plastic Surgery, University Medical Centre Groningen, University of Groningen, Groningen, the Netherlands and is an international editor for Aesthetic Surgery Journal.
Dr Little is a plastic surgeon, Department of Plastic Surgery, Georgetown University School of Medicine, Washington, DC, USA.



