-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Del Vecchio, Michael J Stein, Erez Dayan, Joseph Marte, Spero Theodorou, Nanotechnology and Artificial Intelligence: An Emerging Paradigm for Postoperative Patient Care, Aesthetic Surgery Journal, Volume 43, Issue 7, July 2023, Pages 748–757, https://doi.org/10.1093/asj/sjad071
Close - Share Icon Share
Abstract
An increasing number of aesthetic surgery procedures are being performed in an ambulatory fashion in office-based settings. Postoperative monitoring of these patients has historically required paid private-duty nurses measuring vital signs, encouraging ambulation, and monitoring overall comfort level. Recently, advancements in nanotechnology have permitted high-acuity data acquisition of multiple clinical parameters that can be transmitted to the surgeon's mobile device in a continuous fashion.
The aim of this study was to describe the authors’ early experience with this emerging artificial intelligence technology in the postoperative setting.
Twenty-three consecutive patients underwent radiofrequency-assisted liposuction and Brazilian butt lift surgery, and were placed in a monitoring garment, SimpleSense (Nanowear Technologies, Brooklyn, NY) postoperatively. The primary outcome was device usability, reflected by compliance with wearing the device and completeness of data collection.
During the first 48 hours, 91% of patients wore the device for more than 12 hours per day. Only 39% were compliant with postoperative positioning. No postoperative events were detected.
The quality of data collected enables detection of clinical derangements and can alert the surgeon in real time, prompting interventions such as drug administration, position changes, or presentation to the emergency room.

See the Commentary on this article here.
Patient monitoring following elective outpatient cosmetic surgery has traditionally been limited to transient vital sign evaluation. This leaves aesthetic plastic surgeons with a limited window of opportunity to monitor postoperative health status and treat physiologic disturbances. Similarly, reconstructive plastic surgeons find that evolving reimbursement models, expansion of accountable-care organizations, and increased bundled payments require them to predict and improve their surgical outcomes.
Outpatient aesthetic surgery varies broadly with respect to the degree of invasiveness and physiologic insult to the patient. Notwithstanding, few would disagree that the “triad” of liposuction, abdominoplasty, and Brazilian butt lift (BBL) tops the list. Each of these procedures can lead to life-threatening complications. Despite such mortality, recent 5-year BBL growth rates have surpassed all other cosmetic procedures, doubling over the past 5 years. Besides the aforementioned mortality arising from BBL pulmonary fat embolism, liposuction is a traumatic procedure in its own right, causing marked changes in tissue trauma physiology, fluid shifts, and frank blood loss.
Recently, nanosensor technology woven into fabric has resulted in a wearable vest that can monitor, record, and transmit detailed physiologic data. For surgeries associated with physiologic shifts and the potential for major adverse events, this technology serves to provide the surgeon with continuous physiologic information postoperatively. This provides an opportunity for surgeons to track, and potentially act upon, physiologic derangements that may reflect (or preclude) a complication. The purpose of the present study was to examine the feasibility of remote monitoring in postoperative cosmetic surgery patients.
METHODS
This prospective IRB-approved study (IRB#8244 Sterling) evaluated the utility of an FDA-cleared cloth nanotechnology wearable multisensor vest, SimpleSense (Nanowear Technologies, Brooklyn, NY) in patients who underwent radiofrequency-assisted BBL (RFABBL). Principles of the Declaration of Helsinki were followed, including respect for individuals, the right to make informed decisions, and recognition of vulnerable groups. From February 2022 to June 2022, 23 patients undergoing RFABBL by the senior author (D.D.V.) were monitored with the Nanowear vest for a period of 2 weeks postoperatively. All patients provided informed written consent for participation in the study and were instructed to wear the vest continuously under their clothes for 2 weeks after surgery. Inclusion criteria included healthy individuals over the age of 18 years undergoing RFABBL. Patients were excluded if they had pre-existing comorbidities (ie, BMI over 31 kg/m2, cardiopulmonary disease, connective tissue disease, infection, etc), had an implantable device (ie, pacemaker), or who indicated they would not be able to wear the Nanowear vest in a predictable fashion.
The primary outcome of the study was device usability. Device usability was reflected by patient compliance with the device and completeness of the clinical parameter data collection.
Nanowear Device
The Nanowear cloth nanotechnology wearable multisensor vest is a noninvasive, wearable, and portable device. Clinical data are obtained by utilizing physiologic and biometric sensors to monitor and evaluate patients. The specific physiologic parameters measured include 2 electrocardiogram (ECG) vectors, 2 impedance cardiography vectors, thoracic impedance (Z0), respiration, heart sounds, actigraphy, and posture. The clinical significance of each physiologic parameter is shown in Table 1.
| SimpleSense (Nanowear Technologies, Brooklyn, NY) measured parameter . | Derived biomarker . | Clinical significance . |
|---|---|---|
| ECG vectors | Heart rate and heart rhythm (including occurrences of ectopic beats and frequency of occurrence) | Pain Anxiety Pulmonary embolism Fat embolism |
| Impedance cardiograph | Used to estimate changes in cardiac output over time (this is a trending metric that can be used to observe changes over time) | Anemia Pulmonary embolism Fat embolism |
| Thoracic impedance | Respiration rate and respiration relative tidal volume (this is a metric used to trend the changes in respiratory effort over each breath and over time) | Pain Pulmonary embolism Fat embolism Lidocaine toxicity |
| Activity and posture | Absolute orientation of the chest is measured continuously. Activity as effective movement along x, y, and z axes: in other words, up-down, forward-backward, and side-to-side of the chest is measured continuouslya | Ambulatory level Adherence to post-operative positioning instructions |
| Heart sounds | The presence of distinct S1 and S2 heart sounds and potential presence of S3 or S4 sounds, The loudness of the characteristic heart sounds have been shown to be relevant to estimating blood pressure in SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) | Vasovagal episode Pain Hypertension leading to hematoma |
| Blood pressure | A SimpleSense (Nanowear Technologies, Brooklyn, NY) platform algorithm combines the above vital signs to derive a systolic and diastolic blood pressure measurementb | Vasovagal episode Pain Hypertension leading to hematoma |
| SimpleSense (Nanowear Technologies, Brooklyn, NY) measured parameter . | Derived biomarker . | Clinical significance . |
|---|---|---|
| ECG vectors | Heart rate and heart rhythm (including occurrences of ectopic beats and frequency of occurrence) | Pain Anxiety Pulmonary embolism Fat embolism |
| Impedance cardiograph | Used to estimate changes in cardiac output over time (this is a trending metric that can be used to observe changes over time) | Anemia Pulmonary embolism Fat embolism |
| Thoracic impedance | Respiration rate and respiration relative tidal volume (this is a metric used to trend the changes in respiratory effort over each breath and over time) | Pain Pulmonary embolism Fat embolism Lidocaine toxicity |
| Activity and posture | Absolute orientation of the chest is measured continuously. Activity as effective movement along x, y, and z axes: in other words, up-down, forward-backward, and side-to-side of the chest is measured continuouslya | Ambulatory level Adherence to post-operative positioning instructions |
| Heart sounds | The presence of distinct S1 and S2 heart sounds and potential presence of S3 or S4 sounds, The loudness of the characteristic heart sounds have been shown to be relevant to estimating blood pressure in SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) | Vasovagal episode Pain Hypertension leading to hematoma |
| Blood pressure | A SimpleSense (Nanowear Technologies, Brooklyn, NY) platform algorithm combines the above vital signs to derive a systolic and diastolic blood pressure measurementb | Vasovagal episode Pain Hypertension leading to hematoma |
ECG, electrocardiogram. aThe differentiation of postures between sitting upright and standing upright based only on the data acquired by SimpleSense (Nanowear Technologies, Brooklyn, NY) during that time interval is not currently possible, given that the posture is sensed on the chest. However, the device measures activity and posture, and activity reflects the transition between postures. bIn an observational multisite study by Nanowear, 120 subjects (female (N = 61, 52%) between 18 and 83 years of age were recruited with the following stratification: normal, 20%; prehypertensive, 37%; Stage 1, 26%; and Stage 2, 18%. From these subjects, 1686 measurements of blood pressure from a sphygmomanometer were associated with simultaneously acquired vital signs from the SimpleSense device (Nanowear Technologies, Brooklyn, NY). A proprietary machine-learning–based algorithm called SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) was developed with inputs as metrics derived from the multiparametric data, such as intensity and duration of S1 and S2 heart sounds, the time elapsed between ECG waveforms such as R peaks and these characteristic heart sounds, and patient demographic data, to calculate systolic and diastolic blood pressure.1
| SimpleSense (Nanowear Technologies, Brooklyn, NY) measured parameter . | Derived biomarker . | Clinical significance . |
|---|---|---|
| ECG vectors | Heart rate and heart rhythm (including occurrences of ectopic beats and frequency of occurrence) | Pain Anxiety Pulmonary embolism Fat embolism |
| Impedance cardiograph | Used to estimate changes in cardiac output over time (this is a trending metric that can be used to observe changes over time) | Anemia Pulmonary embolism Fat embolism |
| Thoracic impedance | Respiration rate and respiration relative tidal volume (this is a metric used to trend the changes in respiratory effort over each breath and over time) | Pain Pulmonary embolism Fat embolism Lidocaine toxicity |
| Activity and posture | Absolute orientation of the chest is measured continuously. Activity as effective movement along x, y, and z axes: in other words, up-down, forward-backward, and side-to-side of the chest is measured continuouslya | Ambulatory level Adherence to post-operative positioning instructions |
| Heart sounds | The presence of distinct S1 and S2 heart sounds and potential presence of S3 or S4 sounds, The loudness of the characteristic heart sounds have been shown to be relevant to estimating blood pressure in SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) | Vasovagal episode Pain Hypertension leading to hematoma |
| Blood pressure | A SimpleSense (Nanowear Technologies, Brooklyn, NY) platform algorithm combines the above vital signs to derive a systolic and diastolic blood pressure measurementb | Vasovagal episode Pain Hypertension leading to hematoma |
| SimpleSense (Nanowear Technologies, Brooklyn, NY) measured parameter . | Derived biomarker . | Clinical significance . |
|---|---|---|
| ECG vectors | Heart rate and heart rhythm (including occurrences of ectopic beats and frequency of occurrence) | Pain Anxiety Pulmonary embolism Fat embolism |
| Impedance cardiograph | Used to estimate changes in cardiac output over time (this is a trending metric that can be used to observe changes over time) | Anemia Pulmonary embolism Fat embolism |
| Thoracic impedance | Respiration rate and respiration relative tidal volume (this is a metric used to trend the changes in respiratory effort over each breath and over time) | Pain Pulmonary embolism Fat embolism Lidocaine toxicity |
| Activity and posture | Absolute orientation of the chest is measured continuously. Activity as effective movement along x, y, and z axes: in other words, up-down, forward-backward, and side-to-side of the chest is measured continuouslya | Ambulatory level Adherence to post-operative positioning instructions |
| Heart sounds | The presence of distinct S1 and S2 heart sounds and potential presence of S3 or S4 sounds, The loudness of the characteristic heart sounds have been shown to be relevant to estimating blood pressure in SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) | Vasovagal episode Pain Hypertension leading to hematoma |
| Blood pressure | A SimpleSense (Nanowear Technologies, Brooklyn, NY) platform algorithm combines the above vital signs to derive a systolic and diastolic blood pressure measurementb | Vasovagal episode Pain Hypertension leading to hematoma |
ECG, electrocardiogram. aThe differentiation of postures between sitting upright and standing upright based only on the data acquired by SimpleSense (Nanowear Technologies, Brooklyn, NY) during that time interval is not currently possible, given that the posture is sensed on the chest. However, the device measures activity and posture, and activity reflects the transition between postures. bIn an observational multisite study by Nanowear, 120 subjects (female (N = 61, 52%) between 18 and 83 years of age were recruited with the following stratification: normal, 20%; prehypertensive, 37%; Stage 1, 26%; and Stage 2, 18%. From these subjects, 1686 measurements of blood pressure from a sphygmomanometer were associated with simultaneously acquired vital signs from the SimpleSense device (Nanowear Technologies, Brooklyn, NY). A proprietary machine-learning–based algorithm called SimpleSense-BP (Nanowear Technologies, Brooklyn, NY) was developed with inputs as metrics derived from the multiparametric data, such as intensity and duration of S1 and S2 heart sounds, the time elapsed between ECG waveforms such as R peaks and these characteristic heart sounds, and patient demographic data, to calculate systolic and diastolic blood pressure.1
The wearable device (Figure 1) consists of a harness carrying active and passive cloth-based nanosensor technology, a 3-axis accelerometer, a microphone, a processing unit, a data storage unit, a battery-based power supply, and a wireless module.2 A software system with a user interface on an iPhone (Apple Inc., Cupertino, CA) application supports front-end functionality. A clinician can start and stop recording, schedule prompts, and set reminders to perform recordings at any time of day. Other features include logging nonemergency symptoms or notes and performing automated data-quality assessments to ensure proper use of the wearable device. In addition it is possible to set ranges on biomarker values beyond which the surgeons may wish to receive email alerts. For example: the heart rate for a particular patient may be between 60 and 90 beats per minute given a nominal range of activities performed, such as casual walking. By setting an alert range of 60 to 90 beats per minute for this patient, the surgeon can receive an alert email whenever the heart rate measured exceeds 90 beats per minute or drops below 60 beats per minute. Alternatively, a more complex rule for alerts can be set such as if the blood pressure dropped by more than 30 mm Hg with a coupled increase in heart rate.3 Similarly, with respect to patient positioning, a surgeon may receive the feedback that the patient is supine when they were instructed to be prone, or they are stationary when they were told to ambulate regularly. These alerts can prompt the surgeon to contact the patient and remind him/her to remain compliant with the postoperative instructions.
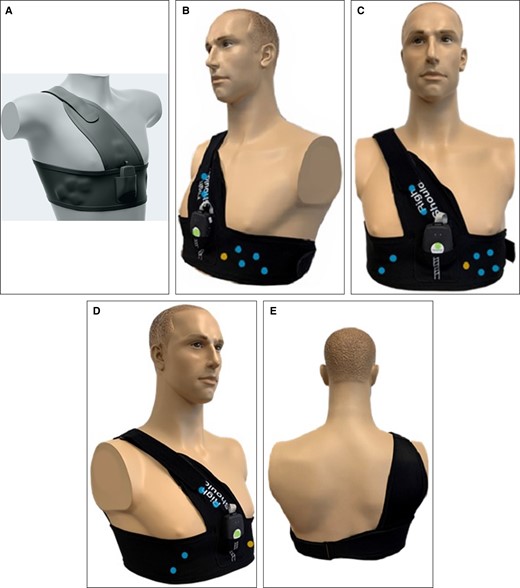
SimpleSense vest (Nanowear Technologies, Brooklyn, NY): (A) a 3-dimensional perspective drawing of the vest; (B-E) locations of the nanosensors and MEMS microphone and accelerometer in right (B), ventral (C), left (D), and dorsal (E) perspectives. Blue dot, cloth-based nanosensors; green dot, 3-axis MEMs accelerator in the SAU; yellow dot, MEMS microphone. MEMS, microelectromechanical systems.
The data are transmitted to an iPhone (Apple Inc., Cupertino, CA) over Bluetooth (Bluetooth SIG, Inc., Kirkland, WA) as seen in Figure 2. This later transmits the data to a secure website (meeting Health Insurance Portability and Accountability Act standards) through wi-fi or a mobile network. The device uses removable media for storage, and the storage capacity is not limited by the amount of data. The battery capacity allows continuous recording of all signals for up to 12 hours.
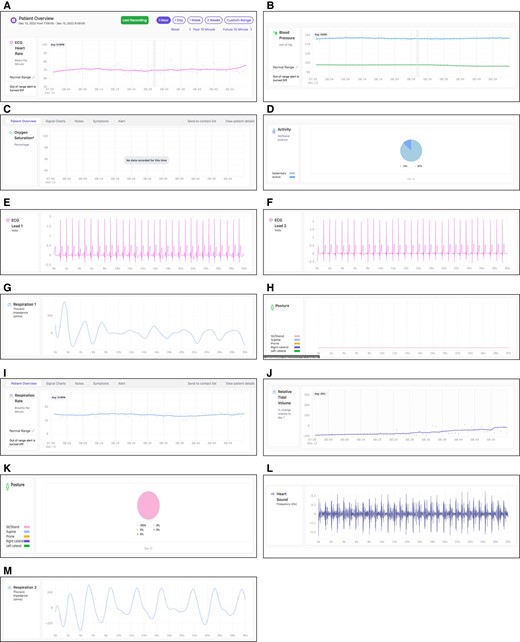
Screenshot of parameters captured on surgeon's iPhone application (Apple Inc., Cupertino, CA): (A) ECG-derived heart rate, (B) blood pressure, (C) oxygen saturation, (D) activity as a pie chart showing percentage of time active or sedentary, (E) vector 1 ECG, (F) vector 2 ECG, (G) vector 1 thoracic impedance, (H) posture over time as a line chart, (I) respiration rate, (J) relative tidal volume, (K) posture in each of 5 categories (sit/stand, supine, prone, right lateral, or left lateral), (L) heart sounds, and (M) vector 2 thoracic impedance. ECG, electrocardiogram.
Surgical Technique and Postoperative Protocol
All surgeries were performed by the senior author (D.D.V.), and involved simultaneous separation and tumescence,4 followed by manual donor site liposuction (Wells Johnson Inc., Tucson, AZ) of the back, abdomen, and flanks, followed by radiofrequency-assisted skin tightening with a bipolar radiofrequency device (BodyTite, Inmode, Lake Forrest, CA). The bipolar radiofrequency device was used at target temperatures of 68°C internally and 38°C externally in all cases. Fat transfer to the buttocks was performed by expansion vibration lipofilling5 and was performed under ultrasound guidance.
Following 2 hours of postoperative monitoring, the Nanowear vest was placed prior to discharge. Subjects were prompted to start recording prior to discharge and were further prompted by the SimpleSense application (Nanowear Technologies, Brooklyn, NY) to perform an automated data-quality check with 10 to 15 seconds of data prior to starting the 12-hour recording. Subjects had the ability to manually enter symptoms they were experiencing at any time during the recording. These symptoms were not used for the management of the patient's condition and were not reviewed by clinicians in real time.
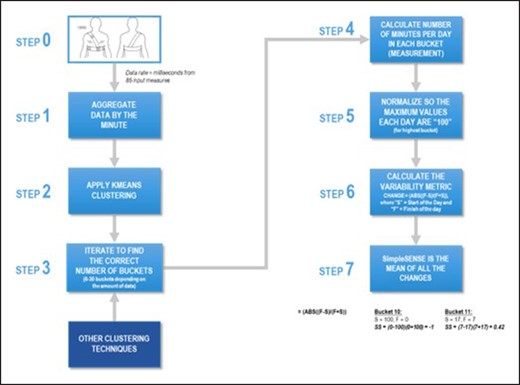
Patient data were extracted on a per-minute basis. Individual time-synchronous measurements were collected with millisecond precision from the 5 categories of Nanowear sensors. The minute-aggregated data were then submitted to the SimpleSense algorithm (Nanowear Technologies, Brooklyn, NY) which applied unsupervised learning to classify the patient readings, and then applied analytic models to derive a rate of change of the patient behavior following the procedure. The data model architecture used by the monitoring device in this study can be seen graphically in Figure 3. Deviations from baseline were hardwired to prompt and alert the surgeon.
RESULTS
Patient Cohort
Twenty-three (1 male and 22 female) consecutive patients were included in this study. All patients were treated by a single surgeon (D.D.V.) to limit variability in operative technique, postoperative care, and outcome measurement. The patients had a mean [standard deviation] age of 39 [8.83] years (range, 25-68 years) and a mean BMI of 29.90 [4.12] kg/m2 (range, 21.9-39.4 kg/m2). The mean surgical time was 109 [26.18] minutes (range, 49-155 minutes, SD = ), and the mean fat transfer volume was 2983 [1343] mL (range, 200-5000 mL). All patients were discharged home after an average of 2 hours spent in postprocedure recovery. There were no intraoperative complications noted or postoperative adverse events in any of the cases included in this study during the monitoring period. All patients were followed for a minimum of 6 months postoperatively.
Patient Compliance
Overall Compliance
All patients in the study wore the device for the 2-week measuring period. Of these, 21 of 23 patients (91%) wore the device for more than 12 hours a day in the first 48 hours, 16 of 23 patients (70%) for the first week, and 12 of 23 (52%) for the full 2 weeks. Considering a greater than 50% wear-time benchmark compliance rate a success, 2 of the 3 rates were significantly higher than 50%. That is, 91% of patients who wore the device 12 hours per day in the first 48 hours was statistically higher than 50% (z = 3.93, 1-tailed P < .001), and 70% of patients who wore the device 12 hours per day in the first week was statistically higher than 50% (z = 1.92, 1-tailed P = .03). The final cohort, those who wore the device 12 hours per day for the full 2 weeks, did not statistically differ from 50%. In other words, through at least the first week, there is significant evidence to suggest patients were compliant with wearing the device above 50% for 12 hours per day. All patients endorsed the device’s comfort, and reported its usability with different clothing styles. Less-compliant patients were asked what made them take the device off; they indicated forgetfulness rather than discomfort.
Posture and Accelerometry Analysis
It is standard to advise BBL patients to sleep and lie prone postoperatively. Interestingly, despite strict instructions provided to the patients postoperatively, 9 of 23 patients (39%) were noncompliant, ie, were recorded to be lying in the supine position, and of these, 6 were lying supine greater than 50% of the time. In other words, 39% of patients were noncompliant with instructions to avoid the sitting or supine position, and these were not brief violations. Although this difference was not statistically lower than a benchmark 50% compliance rate (z = −1.10, 1-sided P = .15), this finding nevertheless has qualitative and medical implications. This unexpected but important finding puts into question the long-held premise that postoperative pressure on the recipient site has an adverse effect on the viability of transplanted fat and warrants further study.
From recent reports of nuanced anatomy of the deep and superficial subcutaneous spaces overlying the gluteus maximus muscle, the “SIME” (static insertion, migration and equalization) technique6 has led to several observations. First, there appears to be migration of fat in the deep subcutaneous space up to a demarcation limit, suggesting deep subcutaneous layer compartments. Second, fat in the deep subcutaneous space survives by oxygen diffusion and not by inosculation per se and may not be as dependent on immobilization as previously thought. This would refute the long-held premise that off-loading is essential for gluteal fat transplantation survival.
Ambulation mitigates the risk of deep vein thrombosis and pulmonary embolism. Of the 23 patients in this study, 60% ambulated 2 or more hours per day. This was also an interesting finding considering all patients received strict instructions to ambulate more than 2 hours a day starting on postoperative day 1.
Completeness of Clinical Parameter Data Collection
A review of the SimpleSense website data indicated that all 5 clinical parameters had been collected for all 23 patients. Other than periods when the vest was not worn, data collection was continuously recorded with no disruptions, representing a 100% success rate of the device registering measurements at the appropriate cadence, a significant difference above a base threshold of 50% (z = 4.80, 1-sided P < .001, 2-sided P < .001). Clinical information was available graphically as seen in Figure 4 and collated data were reviewed for each patient. Analysis of vital signs with patient remarks also reflected symptom correlation. For instance, a patient entering “headache and lightheadedness” at 16:00 on postoperative day 2 could be correlated to chronologically matched clinical parameters showing a brief hypotensive episode. Aggregate data of all 23 patients facilitated minute-to-minute correlation between device data capture and patient symptomatology reporting.

Clinical parameters acquired with the SimpleSense device (Nanowear Technologies, Brooklyn, NY).
Patient Survey Responses
Patients were asked 5 questions related to their comfort wearing the device. The 5 questions asked were:
How do you perceive the overall size of the device (0 = largest and 5 = smallest)?
How secretive is the device (0 = unable to hide, 5 = discrete)?
How adaptable is the device size (0 = not adjustable, 5 = can fit all sizes)?
How comfortable is the device material (0 = uncomfortable, 5 = comfortable)?
How wearable is the device during exercise (0 = can’t be worn during exercise, 5 = can exercise without interference)?
Unfortunately, of the 23 patients who made it through the duration of the study, only 7 completed the survey. Regardless, the survey data were directionally consistent with a positive outcome, with the mean responses all being higher than the scale midpoint value of 2.5 (which indicates neutral comfort across the 5 semantic differential scales employed). Finally, the 5 items (Q1-Q5) were aggregated to create a composite comfortability score. Figure 5 displays the mean values and standard deviations of the 5 questions and the composite item.
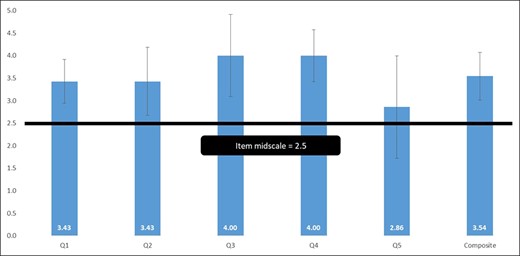
From a statistical perspective, some of those mean values are significantly higher than the 2.5 neutral point of the scale. A set of 1-sample t tests compared to a hypothesized mean of 2.5 (again, the middle of the scale, representing “neutral” comfort) were conducted for each item, with a P value of <.10 utilized as the cutoff due to the small sample size (n = 7). Q1, Q3, Q4, and the composite item were statistically higher than 2.5, indicating that respondents agreed that for those constructs, the device was significantly more comfortable than neutral (Table 2).
| One-sample test, test value = 2.5 . | ||||
|---|---|---|---|---|
| Question | t | df | Significance (2-tailed) | Mean difference |
| Q1 | 2.52 | 6 | 0.05 | 0.93 |
| Q2 | 1.63 | 6 | 0.16 | 0.93 |
| Q3 | 2.17 | 6 | 0.07 | 1.5 |
| Q4 | 3.44 | 6 | 0.01 | 1.5 |
| Q5 | 0.42 | 6 | 0.69 | 0.36 |
| Aggregate item | 2.61 | 6 | 0.04 | 1.04 |
| One-sample test, test value = 2.5 . | ||||
|---|---|---|---|---|
| Question | t | df | Significance (2-tailed) | Mean difference |
| Q1 | 2.52 | 6 | 0.05 | 0.93 |
| Q2 | 1.63 | 6 | 0.16 | 0.93 |
| Q3 | 2.17 | 6 | 0.07 | 1.5 |
| Q4 | 3.44 | 6 | 0.01 | 1.5 |
| Q5 | 0.42 | 6 | 0.69 | 0.36 |
| Aggregate item | 2.61 | 6 | 0.04 | 1.04 |
df, degrees of freedom; t, 1-sample t test.
| One-sample test, test value = 2.5 . | ||||
|---|---|---|---|---|
| Question | t | df | Significance (2-tailed) | Mean difference |
| Q1 | 2.52 | 6 | 0.05 | 0.93 |
| Q2 | 1.63 | 6 | 0.16 | 0.93 |
| Q3 | 2.17 | 6 | 0.07 | 1.5 |
| Q4 | 3.44 | 6 | 0.01 | 1.5 |
| Q5 | 0.42 | 6 | 0.69 | 0.36 |
| Aggregate item | 2.61 | 6 | 0.04 | 1.04 |
| One-sample test, test value = 2.5 . | ||||
|---|---|---|---|---|
| Question | t | df | Significance (2-tailed) | Mean difference |
| Q1 | 2.52 | 6 | 0.05 | 0.93 |
| Q2 | 1.63 | 6 | 0.16 | 0.93 |
| Q3 | 2.17 | 6 | 0.07 | 1.5 |
| Q4 | 3.44 | 6 | 0.01 | 1.5 |
| Q5 | 0.42 | 6 | 0.69 | 0.36 |
| Aggregate item | 2.61 | 6 | 0.04 | 1.04 |
df, degrees of freedom; t, 1-sample t test.
DISCUSSION
The Need for Enhanced Postoperative Monitoring Following Liposuction/BBL
Liposuction is a traumatic procedure, resulting in surface area trauma and fluid resuscitation dynamics, with separate considerations given to frank blood loss. Aspirate volume is a complex conglomerate of unabsorbed tumescent solution, blood, and fat lobules. Although clinical limitations of liposuction are guided by aspirate volumes, not all donor fat connective tissue is the same and not all aspirates are of equal quality. The fibrous nature of some fat vs others varies in several respects, and the term “dense fat” has been coined; we will discuss these variations and their clinical significance in a separate communication. In a first-time liposuction case in a non–dense fat patient, 5000 mL of relatively bloodless aspirate might be comprised of 1000 mL of relatively pinkish tumescent fluid and 4000 mL could be fat. This above example of blood loss contrasts sharply with a redo-liposuction case where 3000 mL of lipoaspirate may be comprised of 1500 mL of fat and 1500 mL of very bloody fluid. Although the former is a higher volume of aspirate, the latter represents a much more dangerous situation. The experienced and astute surgeon must look beyond aspirate volumes and be more aware of every aspect of their surgery—this gives the surgeon the option to make midcourse adjustments to the execution of the surgical plan. Checking the hematocrit of bloody aspirate fluid can be helpful to estimate blood loss and the curtailment of surgery as necessary. Additionally, checking the source of the epinephrine (mixed with lidocaine or in pure ampoules) for light exposure can avoid or correct bloody aspirate sessions. With all the nuanced feedback during liposuction, it becomes clear how a primary surgeon, going from room to room performing fat grafting while designated assistants perform the liposuction, could be completely oblivious to the safety issues of their patients, emphasizing the call for a “single surgeon” standard in body contouring and recommending against designating assistants to perform critical components of these procedures.1 Total aspirate, although the current benchmark, represents an oversimplification of tissue trauma and blood loss and should be replaced with more specific metrics. For the surgeon, a complete understanding of aspirate components, the fibrous nature of their patient's subcutaneous fat, and surgical judgment is vital to their patients’ safety and successful aesthetic outcomes.
Since the classic liposuction guidelines paper by Iverson and Lynch in 2002, patients have been discharged home after having liposuction involving up to 5000 mL of aspirate (although many surgeons use the limit of 5000 mL of fat). Sending patients home after liposuction surgery, now considered commonplace, invites the potential for occult periods of hypotension, dehydration, and other physiologic insults, unbeknownst to the surgeon. Add to this the uncertainty of proper positioning for the BBL recipient, and the argument for more information on the patient in the early postoperative period intensifies.
The concept of wearable computers can be traced back to the work of Thorp and Shannon in the early 1960s. The use of wearable healthcare sensors makes it possible to collect physiologic data over prolonged periods of time, which is not currently feasible in traditional clinical settings. This time-efficient and cost-effective method of monitoring has wide applicability, from routine postoperative monitoring of healthy individuals to home monitoring of patients with chronic diseases, to applications in rural and specialized (prison health) populations, infants and adults with sleep apnea, and specialized cohort groups (military operations).
Although the Holter Monitor has been the mainstay for the identification of occult cardiac arrythmias for over 40 years, the advent of cloud-based technologies and miniaturization of both microchip and battery power technology now affords real-time transmission of clinical patient data for a prolonged period. Numerous studies have demonstrated the value of home monitoring in postsurgical recovery. By “bringing the PACU (Post Anesthesia Care Unit) home,” remote postoperative monitoring has demonstrated powerful predictive value for discharge readiness, early adverse event detection (deep vein thrombosis/pulmonary embolism, pneumonia, infection, skin breakdown), reduction of hospital stays, and ultimately reduction of healthcare costs.
The demand for wearable medical devices is evidenced by unprecedented market growth, projected to increase from US$8.9 billion (2018) to US$29.9 billion (2023). Advancements in microfabrication, microelectronics, flexible electronics, nanomaterials, wireless capabilities, and improved data analysis are contributing to the evolution of textile-based and skin-like/epidermal technologies.
How Remote Monitoring With Artificial Intelligence Can Improve Postoperative Care
The ability to collect a large amount of continuous physiologic data has been facilitated by the development of cost-effective, light, and customizable multifunctional sensors. However, it is the ability to interpret and act on these large data sets that ultimately makes this data-gathering clinically relevant. Deep machine-learning pathways using neural networks are necessary to unveil hidden patterns in collected data, a task that is not achievable with standard analytical and statistical methods. Artificial intelligence methods have been successfully implemented to correlate various electrophysiologic signals (electroencephalogram, electrocardiogram, electromyography) and various activities (rest, walk, exercise), as well as data from wearable sensors to detect textures, objects, and vocal signals.
This study demonstrates the first use of nanotechnology for postoperative plastic surgery monitoring. Patients selected in this study were limited to radiofrequency-assisted liposuction with gluteal fat transfer performed by a single surgeon to minimize confounding variables attributed to surgical technique. Also, as previously mentioned, the cited morbidity/mortality rates of the gluteal fat transfer procedure made it of particular interest to study. The parameters obtained during this study included, atrial electrical activity, ventricular electrical activity, electrocardiogram rhythm analysis, PR interval, atrioventricular conduction interval, patient activity score, posture, cardiac output, stroke volume, patient geographic location and altitude, respiratory rate, relative tidal volume, relative minute ventilation, exercise tolerance, heart rate, transthoracic impedance, heart sounds, and blood pressure.
Most surgeons would strongly prefer to monitor cosmetic surgery patients overnight if it were more feasible from a cost-efficiency standpoint. However, due to rising healthcare costs, the average fee for overnight nursing care alone is between US$400 and US$1,000 per night not including additional facility fees. This makes it challenging to routinely provide overnight monitoring postprocedure. Although the capability of acquiring physiologic data remotely has been available, the ability to assess and synthesize these data by means of neural networks in real-time has not. The nanotechnology used in this study coupled with machine-learning neural networks ushers in a new age in patient monitoring. The concept of “big data” refers to the analysis and integration of large amounts of fast-moving data to create significant value by revealing insights not otherwise possible. According to McKinsey, if the US healthcare system could use “big data creatively and effectively to drive efficiency and quality,” the potential value could be over US$300 billion every year, two-thirds of which would be in the form of reducing national healthcare expenditures by approximately 8%.7
The ability to monitor and analyze patients with wearables through the use of big data allows for improvement of quality while decreasing costs. For example, through continuous monitoring and artificial intelligence, potential problems can be identified earlier, enabling preventative intervention, all while reducing or negating the need for office and hospital visits.
The results of this study were limited by the power of the study and fact that plastic surgery procedures generally have uneventful postoperative outcomes, especially in young, healthy patients. The data collection was limited to the postprocedure period, and did not include a baseline recording for patients preoperatively. It would have been more effective to understand recovery if samples had been taken preoperatively. This before-and-after analysis could then be used to measure trends back to normal. Lastly, there may have been confounding data based on medication usage and its effect on patients. For example, narcotic pain medications are known to impact blood pressure and respiratory rate, and the resumption of preoperative routine medications (ie, beta blockers) will have influenced heart-rate and blood-pressure recordings. Although motion artifact was a concern, the nanotechnology vest appeared to produce high-quality recordings and motion did not significantly confound these data.
CONCLUSIONS
This is the first report of the use of wearable cloth nanotechnology to continuously monitor patients postoperatively following aesthetic surgery, taking BBL as the flagship procedure. A small cohort of respondents generally agreed the device was quite comfortable compared to neutral. Although the ability to continuously monitor patients’ physiologic status and position did not significantly alter patient care or outcomes in the present study, increased use of this cloth-based nanotechnology in larger-cohort and perhaps higher-acuity patient studies will help determine if it can improve safety and outcomes. Future advances in this technology will likely permit contextual risk-stratifying information to be personalized for surgical patients.
Disclosures
Drs Del Vecchio and Theodorou are shareholders with Nanowear Technologies (Brooklyn, NY). Drs Dayan and Theodorou are consultants with Inmode (Lake Forest, CA). The remaining author declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
SimpleSense. Nanowear Inc. January 2, 2023. SimpleSense User Journey. Worldwide Web Accessed on 5/14/23. https://www.youtube.com/watch?v=6fpOY0SR814

Author notes
Dr Del Vecchio is a plastic surgeon, Department of Plastic Surgery, Massachusetts General Hospital, Boston, MA, USA.
Dr Stein is a plastic surgeon, Department of Plastic Surgery, Manhattan Eye, Ear and Throat Hospital, New York, NY, USA.
Dr Theodorou is a plastic surgeon, Department of Plastic Surgery, Manhattan Eye, Ear and Throat Hospital, New York, NY, USA.
Dr Dayan is a plastic surgeon in private practice in Reno, NV, USA.
Dr Marte is a plastic surgeon in private practice in New York, NY, USA.



