-
PDF
- Split View
-
Views
-
Cite
Cite
Elisa Bolletta, Ciara McGoldrick, Elizabeth J Hall-Findlay, Aesthetic Breast Surgery: What Do the Measurements Reveal? A Practical Visual Application of the Results, Aesthetic Surgery Journal, Volume 43, Issue 11, November 2023, Pages NP866–NP877, https://doi.org/10.1093/asj/sjad243
Close - Share Icon Share
Abstract
The results of preoperative and 1-year postoperative measurements in aesthetic breast surgery were outlined in chart form in the Aesthetic Surgery Journal in 2020. Measurements were performed preoperatively and postoperatively, but the authors concentrated on 1-year follow-up because it was generally accepted as the minimum time to define a stable surgical result. Extensive statistical analysis was outlined in the previous paper.
This paper translates those results into a visual form so that the surgeon can see the changes that occur in breast reduction, breast augmentation, mastopexy, mastopexy-augmentation, and implant removal with mastopexy.
There were 548 patients in the breast augmentation group, 388 patients in the breast reduction group, 244 patients for mastopexy-augmentation, and 90 patients for mastopexy. Only primary surgeries that had a full year follow-up comparing preoperative and postoperative measurements were reviewed. Measurements were performed by E.H.F. preoperatively and at each postoperative visit. The measurements that were included in this study were clavicle to upper breast border, upper breast border to nipple, suprasternal notch to nipple, suprasternal notch to inframammary fold, and midline to nipple.
The preoperative and postoperative measurement changes in aesthetic breast surgery were consistent, with minimal variation for each of the aesthetic breast surgery procedures.
The visual interpretation of these results allows the surgeon to accurately plan preoperatively to achieve good, predictable results.
How measurements change after surgery should guide our choices as plastic surgeons in both aesthetic and reconstructive breast surgery. It is important to read Part 1, our original article on what the measurements revealed in aesthetic breast surgery, to understand the statistical analysis that was performed on a large number of cases.1 The database included 4-year postoperative data and outcomes for all procedures analyzed.2 Measurements were performed preoperatively and at 1, 3, and 6 months and 1, 2, 3, and 4 years, but we concentrated on 1-year follow-up because it was generally accepted as the minimum time to define a stable surgical result. Extensive statistical analysis was outlined in the previous paper.
E.H.F. has been measuring breast parameters both before and after surgery for years. In our previous paper in the Aesthetic Surgery Journal, we put together the data resulting from 1 year of follow-up documenting breast measurements and their changes in 4 of the most common aesthetic breast surgery procedures: breast augmentation, breast reduction, mastopexy, and mastopexy-augmentation.1 The tables in the previous paper showed that the results were surprisingly consistent from 1 patient to another. This paper, Part 2, has translated those results into a visual form so that plastic surgeons have a practical method for achieving consistent results with the procedures outlined in both papers.
METHODS
The purpose of this paper was to support our results, previously documented through graphs and tables, with the addition of photographic documentation. We decided to consider only the 4 most frequent types of procedures (breast augmentation, breast reduction, mastopexy-augmentation, and mastopexy). For Part 2, we added visual evidence of the changes that occurred with implant removal and mastopexy.
The measurements in this study were recruited from female patients who had surgery performed by E.H.F. between January 1, 2010, and the end of December 2017. There were fewer mastopexy-only patients, so the measurements were recruited from female patients who had a mastopexy between January 1, 2005, and the end of December 2017. Of course, full 1-year measurements were not available for all patients and those patients were not included. The only other patients who were excluded were those for whom the inframammary fold was purposefully lowered in primary breast augmentations. All procedures were primary and no secondary or revisional patients were included.
There were 548 patients in the breast augmentation group (80% subglandular), 388 patients in the breast reduction group, 244 patients for mastopexy-augmentation, and 90 patients for mastopexy. For the analysis in these 2 papers, only primary surgeries that had a full year follow-up comparing preoperative and postoperative measurements were reviewed. Measurements were performed by E.H.F. preoperatively and at each postoperative visit. The measurements that were included in this analysis were clavicle to upper breast border, upper breast border to nipple, suprasternal notch to nipple, suprasternal notch to inframammary fold, and midline to nipple (Figure 1).
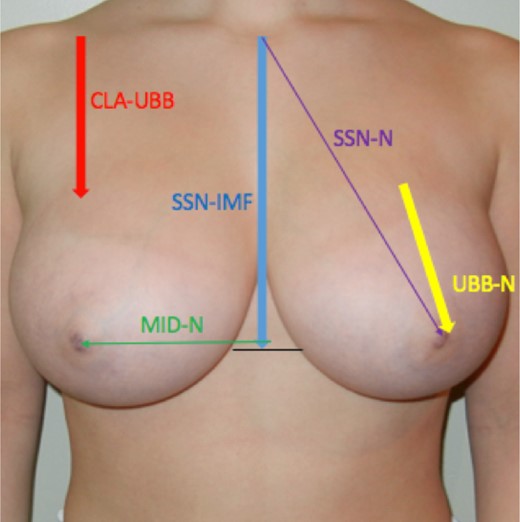
The measurements that were performed both preoperatively and postoperatively by E.H.F. are marked on the photograph of this 17-year-old female breast reduction candidate. Only patients with measurements that were obtained at 1-year follow-up were included in this study. CLA-UBB, clavicle to upper breast border; MID-N, chest midline to nipple; SSN-IMF, suprasternal notch to inframammary fold; SSN-N, suprasternal notch to nipple; UBB-N, upper breast border to nipple. Some of the examples shown in the figures were chosen for illustration purposes and not because they were necessarily all at 1 year follow-up. The changes that they show are consistent with the statistical analysis results.
To avoid bias, for each of the procedures we only considered 1 technique, except for the breast augmentation group, for which we evaluated both the subglandular and the subpectoral planes as well as larger (>500 cc) and smaller (<500 cc) breast implants for the division of the results into subgroups. We also divided the mastopexy group, for which we considered both the Ribeiro (inferior flap) and Graf (inferior flap under a pectoralis strip) methods.3,4
No secondary cases were included. For each group, all charts were reviewed for demographic data, incision location, preoperative morbidity, and postoperative complications.
For the breast augmentation group, all charts were also reviewed for implant profiles (the majority of patients had moderate profile implants), and only patients in whom the inframammary incisions were not intentionally altered were included. Subglandular and subpectoral augmentations along with larger (>500 cc) and smaller (<500 cc) implants were analyzed both together and separately.
For the mastopexy-augmentation group, similar data were analyzed. Superior or superomedial pedicles and a “minus-plus” or “reduction-augmentation” approach, described originally by Paule Regnault, were employed.5 We also investigated, through a regression analysis, whether the amount of the removed breast tissue affected the parameter changes.
For the breast reduction group, all charts were also reviewed for the amount of breast parenchyma removed along with the amount of additional liposuction performed. For the mastopexy group, all charts were similarly reviewed and separated into procedures that had an inferior flap alone performed, vs an inferior flap held up under a pectoralis muscle strip. We correlated different changes in the parameters through a bar graph showing the delta values of each subgroup for each parameter.
In the cases shown for illustration in this paper, we did the measurements before and after surgery shown in Figure 1. We only presented data that were available for a full 1-year follow-up. Some of the examples shown in the figures were chosen for illustration purposes and not because they were necessarily all at 1 year follow-up. The changes that they show are consistent with the statistical analysis results.
We present 5 patients who underwent different aesthetic breast surgery procedures:
Breast reduction—vertical pattern with a superomedial pedicle
Mastopexy—vertical pattern with an inferior flap initially described by Liacyr Ribeiro3
Breast augmentation—both subglandular and dual-plane subpectoral
Mastopexy-augmentation—vertical minus-plus (reduction of the glandular ptosis and augmentation of the upper pole) with a superiorly based pedicle
Mastopexy with implant removal
All procedures were performed by a single surgeon and all measurements were performed by the same surgeon. With a standard measuring tape, data were collected immediately preoperatively and at each follow-up visit.
Drawings were performed at the preoperative visit and arrows pointing to the principal landmarks were added to the preoperative and postoperative photographs to visually enhance the results of our studies. For example, the yellow arrow shows the upper breast border to nipple (UBB-N) distance. The upper breast border is less well defined than the inframammary fold, but it has a more predictable effect on postoperative results. The upper breast border is curved up from the indentation of the preaxillary fold and the breast. Scott Spear and E.H.F. often talked about how the upper breast border was the best landmark for assessing breast parameters (personal communication). The measurements were taken at the level of the breast meridian for both the upper breast border and the lower breast border (inframammary fold).
No secondary surgery cases were included in the data analysis. This study adhered to the guiding principles of the Declaration of Helsinki, and written informed consent was obtained from all patients.
RESULTS
In the previous paper, we analyzed the 5 breast parameter changes at 1-year follow-up.1 Through the statistical analysis of paired samples, we compared 10 pairs of values (every pair referred to a preoperative and 1-year postoperative follow-up value for each parameter and each side, for a total of 20 values), reporting the mean value, the standard deviation, and the number and the mean of the standard error. We performed a paired, 2-tailed t test, without correction for multiple testing, for all comparisons between measurements, separating the right side from the left side. In this way, we analyzed whether the difference between the 2 averaged values of each pair was significant. Pairs with significant difference between the preoperative value and the 1-year postoperative follow-up were reported in the tables in Part 1 (the original paper).1,2 A P value of <.05 was considered statistically significant.
Breast Reduction
E.H.F. performed breast reduction surgery with the superomedial pedicle vertical technique (Figure 2). The CLAV-UBB measurement did not change, which showed that the breast footprint could not be pushed up the chest wall. The SSN-N distance remained where it was marked. If the new nipple position was marked at 24 cm, for example, it remained at 24 cm. It was elevated vertically (compared to the floor) because of the increased projection that was achieved with the vertical approach.
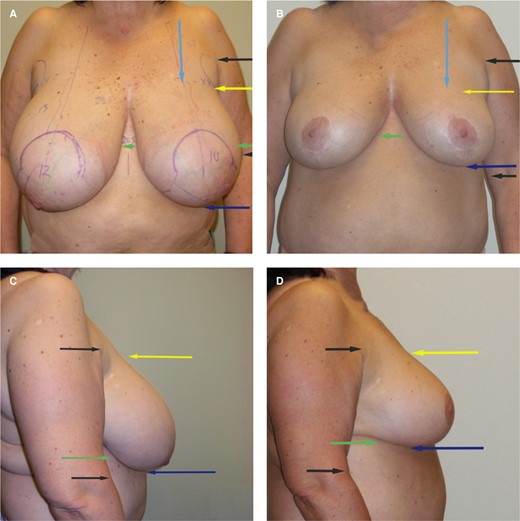
(A, C) Preoperative superomedial vertical breast reduction. (B, D) Postoperative result as seen at 2 years. This 54-year-old female underwent a breast reduction (superomedial pedicle, vertical reduction) with 640 gm removed from the right breast and 610 gm removed from the left breast. She had another 1050 mL of fat removed with liposuction in the lateral chest wall and preaxillary areas, and to shape the inframammary fold. She was 5 feet, 4 inches tall and weighed 174 lb. Note that the upper breast border (yellow arrows) did not change after surgery when compared to the preaxillary crease (upper black arrow). The inframammary fold (green arrow) was elevated when compared to the elbow crease (lower black arrow); our previous paper confirmed a raising of the inframammary fold of on average 1.5 cm. The suprasternal notch to nipple (SSN-N) distance remains where it is marked. The lower border of the breast (dark blue arrow) is where the main effect of the breast reduction is seen. The breast is not pushed up on the chest wall; the lower pole (and lateral) excess is removed.
The SSN-IMF measurement shortened because of elevation of the inframammary fold that resulted from the weight being removed. The surgeon might have purposely elevated the fold more than average in some cases by removing more of the parenchyma above the fold—this led to more variability in this measurement, but our previous data analysis revealed that there was a correlation between the SSN-IMF changes and the amount of removed tissue and liposuction.
Mastopexy
E.H.F. performed mastopexies with the inferior flap described by Liacyr Ribeiro and occasionally with a modification defined by Ruth Graf in which the flap was held under a strip of pectoralis muscle (Figure 3).3,4 The results were similar for both procedures. The UBB was elevated about 1 cm. The SSN-N distance was lengthened about 1 cm from where the nipple was marked preoperatively. This distance did not change with a breast reduction, but it was presumed that the elongation in a mastopexy occurred because the inferior flap added weight to the central portion of the breast (so-called autoaugmentation). The inframammary fold may have been only slightly elevated. The “lift” effect in a mastopexy was not really about the 1-cm elevation of the upper breast border; the lift effect occurred because the lower pole of the breast was moved so that it was centralized behind the new nipple position. The difference between a breast reduction and a mastopexy was that the lower glandular ptosis was “removed” in a breast reduction and “moved” in a mastopexy.
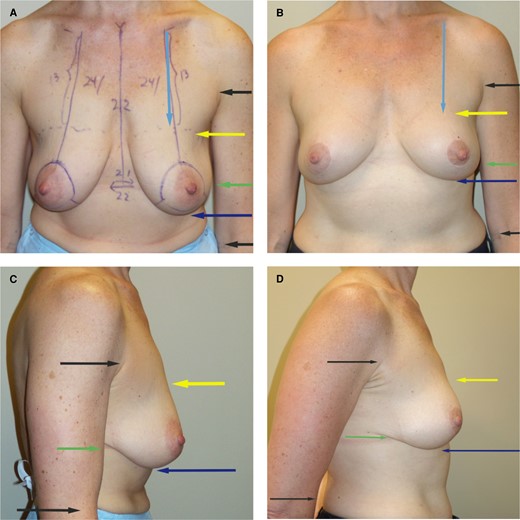
(A, C) Preoperative superior pedicle, inferior flap mastopexy. (B, D) Five-year postoperative result. This 45-year-old female underwent a mastopexy with a superior pedicle and an inferior flap. She was 5 feet, 5 inches tall and weighed 125 lb. Liposuction was not performed. No breast tissue was removed. Note that the upper breast border (yellow arrow) has risen slightly (on average 1 cm). There is more projection from the vertical approach with the inferior flap along with some increase in upper pole fullness. Note that the inframammary fold has not changed much. All of the improvement with a mastopexy is in moving the inferior pole (as opposed to a reduction in which the inferior pole is removed). This is a 5-year follow-up photograph, which shows the long-term stability of this type of mastopexy. The measurements did not change from the 1-year result to the 5-year result.
Breast Augmentation
The SSN-N distance with a breast augmentation lengthened about 2 cm from its original position (Figure 4). It might not appear to drop as long as the implant had been successful in increasing breast projection. Sometimes the nipple might end up higher (as compared to the floor) postoperatively, and sometimes it ended up lower, as in this case.
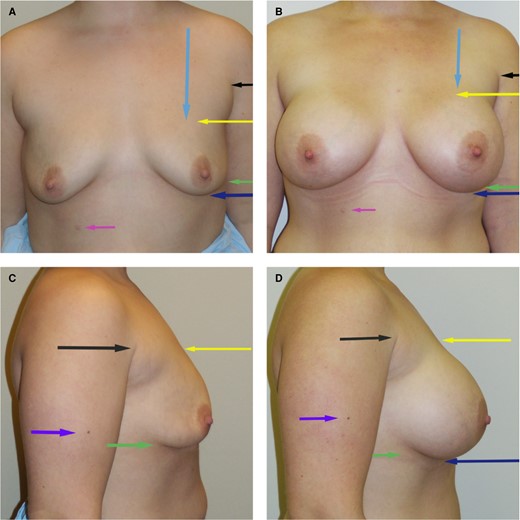
(A, C) Preoperative subglandular breast augmentation. (B, D) Postoperative result. This 27-year-old female underwent a breast augmentation with subglandular smooth-walled silicone gel implants measuring 540 gm each. She was 5 feet, 3 inches tall and weighed 167 lb. Note that the upper breast border (yellow arrow) has been elevated about 2 cm closer to the preaxillary crease (black arrow). The lower breast border (blue arrow) and the IMF (green arrow) have both descended when compared to the purple arrow on the arm and the pink arrow on the abdomen marking a mole for reference. The breast implant is centralized behind the existing nipple position and the upper breast border is elevated, whereas the lower pole (and IMF) descends. IMF, inframammary fold.
In patients in whom the implant was placed in a subpectoral pocket, the upper breast border (once the implant settled) rose about 0.5 cm more than a subglandular implant (2.0 cm for subglandular and 2.5 cm for subpectoral). The IMF, however, lowered more over time with the subpectoral implant, with which it dropped on average 2.4 cm, vs a subglandular implant that dropped on average 1.7 cm. All patients who had their IMF purposely lowered were excluded from this study.
The breast often appeared to be elevated after a breast augmentation procedure. The upper pole was filled, and the upper breast border rose about 2 to 2.5 cm. But surgeons often do not realize that both the lower pole of the breast and the inframammary fold descend. This occurred even when the IMF was not purposely lowered. This result should be taken into consideration when planning a breast augmentation, especially with large-volume implants.
Mastopexy-Augmentation
E.H.F. performed both subglandular and dual-plane subpectoral placement for mastopexy-augmentation patients (Figure 5). If the problem was just nipple ptosis, it was relatively simple to achieve good results. But when there was glandular ptosis, a reduction-augmentation procedure was performed as initially described by Paule Regnault.5 The skin brassiere would not be effective at supporting ptotic gland. The SSN-N distance with a mastopexy-augmentation was lengthened on average 2.5 cm from where it was originally marked. This was again presumed to be the effect of the increased weight of the implant dragging the breast downward.

(A, C) Mastopexy-augmentation preoperative photographs. (B, D) Three-year postoperative results. This 41-year-old female underwent a mastopexy-augmentation with a superomedial pedicle and subglandular smooth-walled silicone gel implants, 240 gm each. She had a “reduction-augmentation” or “plus-minus” procedure with removal of 64 gm from the inferior pole on the right breast and 62 gm from the left breast. Liposuction was not performed. Note that the upper breast border (yellow arrow) has been elevated about 2.5 cm (as opposed to only 2 cm with a subglandular augmentation alone). The IMF (green arrow) has stayed close to its original position (the mastopexy has counterbalanced the natural drop of the IMF with an implant alone). The lower pole of the breast (blue arrow) has been elevated by the reduction aspect of the procedure. The lower pole cannot just be pushed up with the expectation that the skin envelope will hold it. IMF, inframammary fold.
The inframammary fold only dropped minimally in a mastopexy-augmentation patient (0.7 cm) compared with an augmentation alone (1.9 cm). It was presumed that the effect of the mastopexy was able to counterbalance the weight of the implant.
Implant Removal and Mastopexy
When an implant was removed and a mastopexy performed, the measurements worked in reverse. It was important to understand that the upper breast border would drop about 2 cm (Figure 6). This drop was even more dramatic when there was capsular contracture and the upper breast border was abnormally high. It is tempting to design the new nipple position on the existing breast mound, but the surgeon needs to be able to visualize the new mound. The new nipple position should often be designed far lower than desired. Sometimes a subpectoral implant has remained in an abnormally high position, and the new nipple position should be designed even lower when an implant is sitting abnormally high. Occasionally, when an implant has bottomed out, the upper breast border may have already dropped, and this must be evaluated preoperatively. Note how low the nipples were marked on this patient.
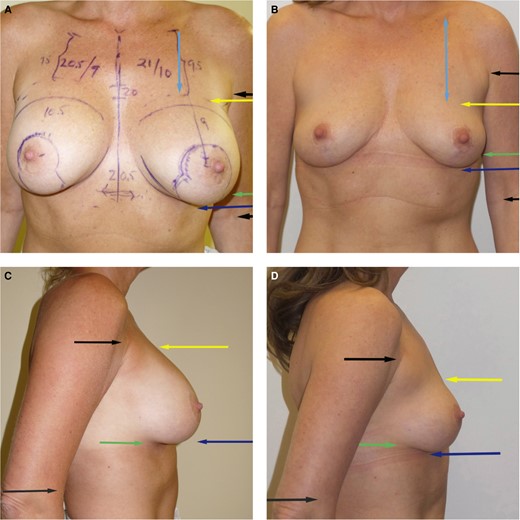
(A, C) Preoperative implant removal and mastopexy. (B, D) Postoperative photographs at 1 year. This 49-year-old female underwent removal of her smooth-walled subpectoral silicone gel implants that were 304 gm each. A mastopexy was performed with no breast tissue removed. She was 5 feet, 4 inches tall and weighed 113 lb. Note that the measurements are reversed when compared to the previous examples. The upper breast border (yellow arrow) has dropped about 2 cm (as compared to the arrow marking the preaxillary crease). The inframammary fold (green arrow) has risen with the weight of the implant removed. Note how little the nipples were elevated. It is essential that the surgeon recognizes that the upper breast border will drop (even more when capsular contracture is present), so it is important not to place the nipples too high.
Good results in a mastopexy-augmentation were achieved when the plus-minus approach was employed and some of the glandular ptosis was removed. The implant then added to the lower pole, so it was important for the surgeon to be aware that correction of the large inferior pole would be achieved with implant removal only. Only rarely will any gland need to be excised when implants are removed and a mastopexy performed. The pillars can be inverted, and the vertical skin closed.
DISCUSSION
Much has been written on what constitutes the ideal breast, but it has rarely been distilled into quantifiable parameters. In some studies there has been an attempt to create protocols to objectively evaluate breast measurements, but they have a difficult task and very little information exists regarding their reliability. This paper, as a completion of our retrospective study of changes in breast measurements, might help colleagues improve their surgical planning and optimize their outcomes.
Although much has been written about breast aesthetics, the literature lacks a simple, systematic, and comprehensive view on the preoperative breast assessment.6 We can find very few articles in the literature that report the changes in breast surgery based on objective parameters. Even fewer have relied on measurements for their conclusions.
To our knowledge, there are no scientific studies that have utilized the upper breast border as the main anthropometric benchmark or studies in which such a large follow-up of anthropometric measurements 1 year after surgery and beyond have been collected and analyzed. This lack of standards makes it difficult to compare results of different surgical techniques among surgeons.
It is critical to point out to patients whether they have a high or low breast footprint: the measurements confirmed by our cases show that the footprint cannot be pushed up the chest wall even though the borders of the footprint can be altered to some degree. According to our results, a low-breasted patient with a slightly low nipple position may be best managed with a mastopexy-augmentation, whereas a high-breasted patient with a similarly shaped breast may be best managed by an augmentation alone, with intentional lowering of the inframammary fold.
Our results show that the changes in breast measurements from preoperatively to postoperatively are quite consistent, with a reliable (at least 1 full year) period of follow-up, as reported in the previous paper.1 The changes in the upper breast border are predictable in each procedure, which confirms that the upper breast border can be considered a good landmark for deciding the new nipple position. The new nipple position is best determined in relation to the upper breast border and the lower pole of the breast rather than the inframammary fold (which can be more variable from patient to patient). The eye of the beholder sees the overall breast mound with the nipple position on the mound rather than where the IMF is located. The surgeon needs to know what the measurements show will happen with each type of procedure to end up with an ideal nipple position postoperatively.
In 1994, Freiberg et al showed that the suprasternal notch to nipple distance did not change from where it was marked after a breast reduction with an inverted-T inferior pedicle. The lower pole of the breast would bottom-out, but the nipple stayed in the same place over time.7
Swanson in his article in ASJ in 2010 showed that the IMF crease is a dynamic structure.8 The IMF descended on average 0.71 cm in all primary augmentations (n = 17). He also pointed out that the inframammary fold was elevated in a vertical breast reduction (n = 1) and a vertical mastopexy (n = 5). He showed that the IMF actually also was elevated with a mastopexy-augmentation (n = 15). Our measurements included significantly more patients but followed a similar trend in the breast reduction group.
Mallucci in his PRS article of 2016 on the ICE principle stated that when an implant exceeded the breast capacity (dimensions), abdominal skin was recruited onto the lower pole of the breast from the abdomen.9 Because his article emphasized the need to lower the incision below the existing IMF, it was clear that the implant was actually sitting lower on the abdominal wall rather than having skin recruited upward. This is shown by the mole on the lateral chest wall which was at the level of the IMF in his preoperative photographs, whereas in the postoperative photographs the IMF was lower than the mole. The mole did not move; the implant sat lower on the chest wall than the original breast footprint.
We agree with the discussion by Atiyeh and Chahine in PRS in February 2017, which emphasized that centralizing the implant behind the existing nipple position was more important than IMF considerations.10 Either the implant was centralized behind the existing nipple, or the nipple was moved up to the level on the footprint where it would result in a centralized position.
Some publications also investigated the long-term changes in nipple position and breast shape following Wise pattern/inferior pedicle breast reduction: Rheus and Mathes followed 22 patients and found that the length of the vertical scar increased over time, with a superior displacement of the nipple areola-complex, although the overall breast projection was well preserved and the midclavicle to nipple distance did not change.11
Only a few studies have been performed to examine changes following vertical scar reduction mammaplasty. Keck et al followed 72 patients for 1 year after vertical scar reduction mammaplasty and reported an increase in the suprasternal notch to nipple distance and scar length, on average 17% and 22%, respectively.12
In 2008, Lista described that, with vertical measurements (unlike in this study, in which the measurements were made along the breast skin), the breast reduction elevated the nipple above the marked position.13 With a straight ruler, he showed in 46 patients that the nipple was 1.3 cm higher on postoperative day 5 from where it was marked and 1.0 cm higher at 4 years.
The plastic surgical treatment of the opposite breast after reconstruction is still not well addressed in the literature, even though it is a key element in achieving symmetry and patient satisfaction. Persichetti et al reviewed 28 patients for unilateral breast reconstruction with implants and contralateral breast reduction with an inverted-T superior pedicle technique and an inferiorly based dermal adipose flap.14 They assessed the long-term stability and aesthetic result of the reduced breasts at 5 years postoperatively, and they found minor variations when analyzing the comparison of the preoperative and postoperative measurements (sternal-notch to nipple distance and inframammary fold to nipple distance).
Salgarello et al reviewed 19 consecutive patients undergoing unilateral NSM (nipple-sparing mastectomy) with immediate prosthetic reconstruction and contralateral simultaneous symmetrization with the tailored reduction/augmentation mammaplasty technique; they principally focused on the importance of adjusting the healthy breast tissue to the reconstructed one, choosing a proper size of implant together with a resection of the central breast base.15 The average follow-up time was 13 months.
Understanding how the measurements change in aesthetic breast surgery can also be applied to breast reconstruction patients, especially with respect to symmetrization procedures. If the upper breast border is higher on the reconstructed side, then it would be better to choose an implant for symmetrization and perform a minus-plus mastopexy-augmentation rather than just a reduction or mastopexy. Neither the reduction alone nor the mastopexy alone will result in symmetrical upper breast borders without the addition of an implant (or fat grafting if the difference is minimal).
The purpose of this study has been to help surgeons create better and more predictable outcomes, and to provide a framework by which results can be assessed in an objective manner. Measurements are not necessary to perform good surgery, but every surgeon should understand what the measurements show, and what happens to the breast over time with gravity and physiological changes. This is essential for visualizing what is possible to achieve, and as well for managing surgical results and making systematic advances in treatment. In that way, breast measurements become the pattern on which preoperative surgical decisions can be made.
These measurements allow us to plan surgery so that we can achieve consistent, predictable results. For example, we know that we cannot push the breast footprint up, but we can adjust the footprint borders by either adding or removing volume. The upper breast border does not change in a breast reduction, so we can use that landmark to accurately mark the new nipple position. The upper breast border will rise about 1 cm with the inferior flap (Ribeiro) type mastopexy and it will rise about 2.5 cm (subpectoral, 3 cm) when performing a mastopexy-augmentation.3 Because these measurements are quite consistent, with minimal variability across a wide range of patients, we can better visualize our results and make appropriate plans. E.H.F. consistently applies this knowledge to mark potential results on patient photographs at the time of initial consultation. The final results seen at 1 year postoperatively are very close to the results drawn, allowing her to better manage patient expectations.
The footprint forms the first two breast dimensions, and the breast mound forms the third dimension.16 These measurements also show consistency in what happens to the mound itself with various aesthetic procedures. The lift effect of a breast reduction results from removal of the inferior pole, whereas the lift effect of a mastopexy results from rearrangement of the inferior pole. This so-called lift effect is achieved with either no (breast reduction) or minimal (mastopexy) changes in the upper breast border.
The lower pole of the breast is lowered when an implant is added. This can be quite acceptable in a pure breast augmentation, but it can lead to an unacceptable result in a mastopexy-augmentation. If a mastopexy-augmentation is being performed solely to correct nipple ptosis, the lowering of the breast may be acceptable. On the other hand, when the problem is glandular ptosis, the weight of the implant will make this worse. Reduction of the lower pole is often necessary when an implant is added to prevent “recurrent glandular ptosis.”5 This effect of adding weight helps us understand why the lower pole of the breast often remains unchanged in a mastopexy-augmentation even when some of the glandular ptosis is removed. It also helps us assess whether the problem is nipple ptosis, glandular ptosis, or both.
Determining the new nipple position will depend on an understanding of what happens to the breast mound. Because an implant will lengthen the suprasternal notch to nipple distance about 2 cm at the same time as the weight of the implant lowers the lower pole, surgeons must understand what changes will occur in the upper breast border as well as the mound itself. The SSN-N distance will not change from where it is marked preoperatively unless weight is added. The inferior flap mastopexy does add some weight to the midportion of the breast mound, and this results in a SSN-N lengthening of about 1 cm. An implant adds weight to the whole breast mound and this results in lengthening of the SSN-N distance by 2 cm.
Preoperative marking and determining the new nipple position is much more difficult in a mastopexy-augmentation, in which the upper breast border rises about 2.5 cm and the new suprasternal notch to nipple position is lengthened. The limitation of this study was that the lengthening of the new nipple was assessed along the skin surface and not vertically. Skin lengthening does not take into account the effect of increasing breast projection. The authors are currently conducting a study of those vertical changes, because they will likely help surgeons with preoperative planning more than skin lengthening measurements alone.
Another limitation of this study was that the measurements were performed for specific procedures. For example, these results would not apply to an inferior pedicle breast reduction in which the weight is not removed from the lower pole of the breast. These measurements only apply to a superomedial vertical breast reduction, an inferior (Ribeiro type) mastopexy, or a mastopexy-augmentation that removes glandular ptosis.3,6,17
The inframammary fold, although better defined than the upper breast border, is much more variable and can mislead the surgeon when planning the new nipple position. When a superomedial pedicle vertical breast reduction is performed, the IMF is unweighted, and it will often rise. When an implant is added, the IMF drops on average 2 cm (when it is not purposely lowered). On the other hand, when a mastopexy-augmentation is performed the IMF remains closer to its original level because the mastopexy (with removal of glandular ptosis) will counteract the effect of the added implant weight.
All of these measurements come together for the surgeon when performing an implant removal and mastopexy. The reverse effects will happen to both the upper breast border and the lower pole of the breast. This means that it is important for the surgeon not to move the new nipple position too much. This will be especially important when a patient has elevation of the breast due to capsular contracture.
Because these measurements results are so consistent, surgeons can use them to better understand what happens and therefore better plan and perform accurate preoperative markings. When we, as surgeons, can manage our own expectations, we can better manage patient expectations.
All plastic surgeons should rigorously analyze their own practice to standardize decisions, based on objective measurements, and abandon arbitrary and subjective assessment methods. We think our study has presented an outcomes benchmark, for comparison of other surgical outcomes to a standard outcome, and to determine the current best tailored procedure for each patient.
CONCLUSIONS
In this paper we tried to give colleagues a more practical (visual) understanding of aesthetic breast surgery measurements to improve preoperative planning and optimize outcomes. Our statistical analysis of preoperative and postoperative measurements has shown that the results were consistent and predictable. We need to remember that we cannot accurately evaluate what we do not measure. Predicting changes in breast measurements, and then comparing our data with those of other surgeons, allows us to better master our own practice by minimizing the variability inherent in the surgical act and in differences between patients. The purpose of this study was to help surgeons create better and more predictable outcomes and provide a framework by which results can be assessed in an objective manner.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
Author notes
Dr Hall-Findlay is a plastic surgeon in private practice in Alberta, Canada.
Dr Hall-Findlay is a Aesthetic Breast Surgery section co-editor for Aesthetic Surgery Journal.
Dr Bolletta is a consultant plastic surgeon, Department of Plastic and Reconstructive Surgery, Policlinico S. Orsola-Malpighi IRCCS, Bologna, Italy.
Dr McGoldrick is a consultant plastic surgeon, Belfast City Hospital, Belfast, Northern Ireland.



