-
PDF
- Split View
-
Views
-
Cite
Cite
Nicolas S Dhooghe, Sebastiaan Maes, Bernard Depypere, Karel E Y Claes, Renaat Coopman, Bela Kubat, Michel H Piette, Stan Monstrey, Fat Embolism After Autologous Facial Fat Grafting, Aesthetic Surgery Journal, Volume 42, Issue 3, March 2022, Pages 231–238, https://doi.org/10.1093/asj/sjab252
Close - Share Icon Share
Abstract
Autologous facial fat grafting has gained popularity in recent years and is considered to be safe. This paper presents the case of a patient who died due to massive cerebral microfat embolism after facial fat grafting.
The aim of this study was to raise awareness and provide more evidence on the prevention and treatment of this potentially lethal complication of facial fat grafting.
A detailed report was made of the case. Two online databases were searched for similar cases of facial fat embolism resulting in neurologic and/or visual symptoms. Thereafter a literature search was conducted to verify the etiology, current treatment options, and preventive measures.
Forty-nine cases with similar events were found in the literature. The most common injected area was the glabella (36.1%), and an average of 16.7 mL fat was injected. The main complications were visual impairment, with 88.5% of cases resulting in permanent monocular blindness, and neurologic symptoms, some of which never fully recovered. Including the present patient, 7 cases were fatal. Fat embolism can occur in the veins and arteries of the face. Two possible pathways for fat embolism exist: the macroscopic, mechanical pathway with immediate signs, and the microscopic, biochemical pathway with delayed symptoms. Mechanical embolectomy and corticosteroids are suggested treatment options but evidence for their efficacy is lacking. Several different preventive measures are described.
Although facial fat grafting is considered a safe procedure, one should be aware of the risk of fat embolism. Underreporting of this adverse event is likely. With no effective treatment and often detrimental outcomes, preventive measures are of utmost importance to improve patient safety.
Autologous facial fat grafting has gained much interest in recent years and has become a standard procedure for soft tissue reconstruction and augmentation. Correcting deflation of facial fat compartments through volumetric augmentation is essential in facial rejuvenation.1 Autologous fat is seen as the ideal filler because of its favorable characteristics; it is often abundantly available, has a low complication rate, is permanent, is host-compatible, and can be harvested in a minimally invasive way and under local anesthesia.2-4 Fat grafting is considered to be a safe procedure. However, in the literature more severe complications due to fat embolism have been reported, including unilateral vision loss, cerebral infarction, and even death. Complications can occur immediately or can be delayed.5-7
The aim of this paper was to give a detailed report of an adverse event together with an overview of similar cases to raise awareness of this potentially lethal complication of facial fat grafting. In addition, we undertook a literature review to provide an overview of the evidence about prevention and treatment.
We present the case of a 57-year-old transwoman who died 24 hours after facial gender confirmation surgery elsewhere. She underwent, under general anesthesia, a lowering of the hairline, correction of frontal bossing, a brow lift, reduction of the chin and lower mandible, a face-lift, and lipofilling of the upper lip and glabellar area. Postoperatively, the patient was monitored overnight in the clinic and discharged in a good general condition the following morning. However, later that day she was found dead in her hotel room. Postmortem examination in cooperation with our university showed extensive multifocal cerebral softening, due to multiple microfat embolisms in the cerebral circulation, localized subarachnoid hemorrhages, and an intraventricular bleeding in the fourth ventricle. No cerebral imaging was performed. Examination of the circle of Willis, bilateral middle cerebral arteries, and internal carotids showed no signs of obstruction. No signs of fat embolism were found in the lungs. Blood analysis showed no coagulation disorders and thromboprophylaxis with low-molecular-weight heparin had been given in the perioperative period. This patient was operated elsewhere and this case report is based on the information available during the criminal investigation of her death. No detailed operative report was provided, just a summation of the different procedures performed. Therefore, no data are available on the quantity of fat transplanted, or on the technique and cannulas used for harvest and injection of the fat. Permission to publish this case anonymously was given by the justice department.
METHODS
In January 2020, 2 online databases, PubMed (United States National Library of Medicine [NLM], Bethesda, MD) and Embase (Elsevier, Amsterdam, the Netherlands), were searched for the following MeSH terms: “adipose tissue” AND “transplantation, autologous” AND “face” AND “embolism, fat” for PubMed, and “autologous fat transfer” AND “fat embolism” AND “face” for Embase.
Inclusion Criteria
As the caseload on this topic is very limited, the threshold for inclusion was very low. Every human case that could be found from letters, case reports, and reviews, written in English or French, was included. Time was not a limiting factor.
Exclusion Criteria
All papers featuring animals or with other fillers, such as hyaluronic acid, were excluded; as were articles with fat transfer in regions other than the face. References of the included articles were analyzed, and articles retrieved this way were processed with the same method until no further articles could be found.
For all the search results the title and abstract were scanned by the 2 leading authors (N.D. and S.M.). The outcomes were compared, and differences were discussed and evaluated for inclusion or exclusion. If no consensus was found, an independent person (K.C.) would decide after hearing the arguments of both sides.
The following parameters were extracted from the included articles: sex, age, injection site, amount of fat injected, first symptoms, time to first symptoms, treatment, and outcome.
A further literature review on the pathogenesis, treatment, and prevention of fat embolism in facial fat grafting was performed.
RESULTS
Nine publications on fat embolism after facial fat grafting were found. All 9 met our inclusion criteria. Further analysis of references resulted in inclusion of 30 extra articles, resulting in a total of 49 cases, plus the case reported in this article. The extracted data of these 50 cases are summarized in Supplemental Table 1, available online at www.aestheticsurgeryjournal.com.
Of the 49 cases, 29 were female (59.2%), 6 male (12.2%), and in 14 cases (28.6%) the gender was not reported. The average age of the patients was 35.2 years (range, 19-66 years). The most common grafted locations were the glabellar (35%), the nasolabial (20%), and temporal area (13.3%). In only 24% of the cases was the volume of fat grafting reported, with the average volume injected being 16.7 mL. In 18% of the cases, timing of the onset of symptoms of fat embolism was not clearly reported; where it was reported, 9.7% mention the onset as occurring during injection, 48.8% immediately after, and 41.5% ranging between 1 hour and 4 days after. The most common reported symptoms were neurologic symptoms (paralysis, aphasia, and loss of consciousness) (34%), vision loss (32%), or both (24%). In 88.5% of the cases where vision loss occurred, permanent monocular blindness ensued; 11.5% did not report the final outcome. Signs of skin ischemia were described in 2 cases. Other reported symptoms were gastrointestinal, high blood pressure, and fever. Monocular blindness is the most common complication, occurring in 26 cases (53.1%). This was accompanied by neurologic complications in 7 cases with mild neurologic recovery in 6 cases and no neurologic recovery in 1 case. Cerebral fat embolism occurred with nonvisual neurologic complications in 11 cases (18.6%). There was some degree of neurologic recovery in 6 of these cases, no neurologic recovery in 3 cases and significant neurologic recovery in 2 cases. Six patients died (12.2%) and in 6 cases (12.2%) no complications were reported.
DISCUSSION
Vascular Anatomy of the Face
Taylor and Palmer introduced the angiosome concept by which the body is considered to be composed anatomically of multiple 3-dimensional composite blocks of tissue supplied by particular source arteries. The main angiosomes of the face are supplied by the ophthalmic artery coming from the internal carotid artery, and by the facial, superficial temporal, postauricular, and internal maxillary arteries, all branches of the external carotid artery (Figure 1). Multiple connections exist between these angiosomes and across the midline, mainly by small-caliber choke anastomoses, especially in the scalp and superficial muscular aponeurotic system layer of the face.8-10
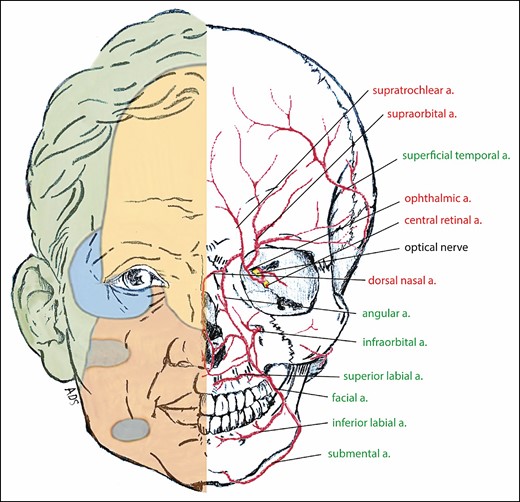
The right half of the face, illustrating the facial angiosomes and showing the internal carotid and ophthalmic arteries (yellow), the internal maxillary artery (blue), the facial artery (red), and the superficial temporal artery (green). The main branches of the ophthalmic artery (branch of the internal carotid artery) (red) and the external carotid artery (green) are shown on the left half of the face.
Experience with facial allograft transplantation has shown that the angiosome of the ophthalmic artery at the central forehead and nasal dorsum can be supplied by reverse flow from the adjacent superficial temporal and facial artery territories.8-10
Skin perforators of the main facial source vessels pierce the deep fascia at areas of skin attachment to the deeper layers, with a high density at the orbits, zygomatic arches, and root of the nose.10 These locations are common injection sites for fillers and fat grafting. Anatomic studies of the ophthalmic artery show that its terminal branches mainly emerge at the superior part of the medial orbital rim (Figure 1).11
Considering this vascular anatomy, arterial intravasation of fat in the face can reach the internal carotid artery through the terminal branches of the ophthalmic artery and through adjacent angiosomes, supplied by branches of the external carotid artery. Injection of fat under pressure can overcome the arterial pressure and generate a retrograde flow, similar to intravasation of fillers, which has been more frequently reported in the literature.12
The volume required to generate this reversed flow does not need to be high. As little as 3 mL of saline, containing an isotope, injected rapidly into the radial artery was enough to be detected at the carotid-subclavian junction.13 Khan et al even showed that injecting <0.1 mL of saline was enough to overcome the volume of the supratrochlear artery from the glabella to the bifurcation at the orbital apex.14 Retrograde flow to the ophthalmic artery and internal carotid artery can allow the fat particles to reach the retinal artery and the cerebral circulation.
The face also has a vast venous network, the course of which is often at a distance from the associated arteries.10 Venous intravasation in a facial vein will drain into the external jugular vein. It would then continue into the superior vena cava, the right heart, and the pulmonary circulation.13 Venous intravasation of fat particles has attracted more interest since 13 deaths following gluteal fat grafting were described by Cárdenas-Camarena et al.15 The right heart is then reached by the vena cava inferior and pulmonary embolism can occur.
Pathogenesis of Fat Embolism
Fat embolism can only occur after intravasation of fat. In facial fat grafting, fat can inadvertently be injected in an artery or vein of the face. As it enters the circulation it can cause problems through 2 different pathways; it can immediately cause a mechanical obstruction of the vessel, or it can cause an inflammatory cascade, eventually leading to delayed endothelial injury resulting in blood vessel and local tissue damage. These pathways are referred to as, respectively, the mechanical or macroscopic fat embolism pathway and the biochemical or microscopic fat embolism pathway (Figure 2).16,17
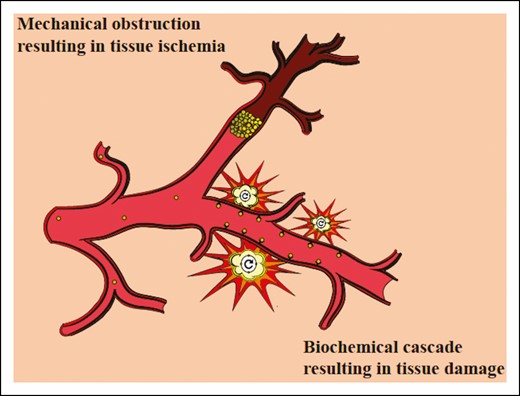
In the macroscopic pathway mechanical obstruction by fat causes tissue ischemia and immediate symptoms. In the microscopic pathway there is no obstruction, but a biochemical cascade is initiated by fat particles and leads to surrounding tissue damage and delayed symptoms.
If the fat particles enter a facial vein, they will eventually be trapped in the capillaries of the lungs. Macroscopic pulmonary fat embolism can cause mechanical obstruction of these capillaries, which can result in right heart failure and associated cardiopulmonary decompensation. Microscopic pulmonary fat embolism does not cause an immediate obstruction, but the lungs will react with the release of lipase. This enzyme will hydrolyze the fat particles, releasing free fatty acids and glycerol in the circulation, causing a huge increase in the permeability of the capillaries. This destroys the architecture of the alveoli and can cause edema and hemorrhaging. Subsequently, a release of inflammatory mediators can trigger a systemic reaction which can result in respiratory insufficiency and death. As this inflammatory cascade takes some time to develop, a delay of symptoms of between 24 hours and 3 days can be observed.16,17
Few articles describe what happens if fat particles enter an artery. A macroscopic fat embolism, blocking an artery in the eye or the brain, will cause immediate ischemia. The pathophysiology of a microscopic embolism is not so clear. We already know the impact of free fatty acids on the pulmonary tissue, but the effect on neural or optical tissue remains to be clarified. Based on the known pathway in the pulmonary circulation and delay in symptoms, we believe it might cause a similar inflammatory cascade, damaging the tissue surrounding the arteries. There is no clear cut-off point between immediate and delayed symptoms. Macroscopic and microscopic fat embolism might occur simultaneously, causing both early and delayed symptoms.18
Treatment
Only 2 of the 50 cases from this review report venous intravasation and pulmonary fat embolism.19,20 Both resulted in death. Venous fat embolism, both micro- and macroscopic, can lead to cardiopulmonary decompensation. This condition, with a poor prognosis, is seen more often in gluteal fat grafting.21 Treatment consists of supportive care and cardiopulmonary resuscitation. Extracorporeal membrane oxygenation could be associated with a better prognosis. Successful use of extracorporeal membrane oxygenation in the event of fat embolisms following orthopedic fixation and trauma has been reported. There is no evidence for its use in pulmonary fat embolism after fat grafting.22
Many different treatment options have been reported for arterial fat embolism after facial fat grafting. Reperfusion of the vessels is of utmost importance. In strokes caused by large vessel occlusions, stents are used as a recanalization method to reduce mortality and morbidity.6 Intra-arterial thrombolysis, used in 9 cases, involves the mechanical and/or pharmacologic clearance of the embolism. Zhou et al performed a mechanical lipectomy, by placement of a stent and aspiration of the fat, and were the only group to demonstrate a significantly improved neurologic status.23 The low degree of success of these techniques can be explained by the technical difficulty of removing the fat embolism.6
The usefulness of corticosteroids for fat embolism syndrome after long-bone fracture was published by Lindeque et al as long ago as 1987.24 Safran et al stated that a single prophylactic dose of methylprednisolone is effective in the prevention of fat embolism syndrome after gluteal augmentation in high-risk patients, without any clinical effect on wound-healing.16 However, the sample size in this study was low and there is no clear definition of a high-risk patient in facial fat grafting. Six cases mention the use of corticosteroids and only 1 case reported an improvement in neurologic status.7,20,25-27 Prophylactic use of corticosteroids was not reported. It is our belief that it could be useful to block the inflammatory cascade in microscopic fat embolism.
Occlusion caused by autologous fat does not respond to thrombolytic agents.6 However, if the blood flow is slowed down or disturbed by the presence of some filler material, formation of thrombi can occur.28 Animal studies showed the beneficial effects of thrombolytic agents (recombinant tissue plasmogen activator) intravenously in embolisms caused by hyaluronic acid.28 Direct intra-arterial delivery of urokinase is reportedly effective at recanalizing major symptomatic cerebral arterial occlusions after embolism caused by hyaluronic acid. No cases have been reported where thrombolytic agents were used for fat embolism.29 Three cases reported the use of antiplatelet agents, with little evidence to support its use.20,25,26 The administration of an anticoagulant, such as heparin, in fat embolism after gluteal fat grafting does not improve the outcome.16 Some cases mention the use of mannitol and even craniectomy to reduce intracranial pressure. 6,26 This pressure might rise due to brain edema after cerebral fat embolism.
During local anesthesia, acute neurologic or visual symptoms can be noticed. The procedure should then immediately be stopped. For an arterial embolism, acute stroke interventions should be initiated. If venous embolism is suspected, ICU admission combined with mechanical ventilation and hemodynamic support should be considered.17 Instructions should be given to patients that vision loss and respiratory and cerebral dysfunction can occur in the first 4 days after the procedure and, if present, medical help is urgent. Therefore, patients should not be left alone in the first days after the procedure.
Risk Reduction in Facial Fat Grafting
Neurologic deficit, monocular blindness, and death are extremely severe complications, even more so for cosmetic procedures. The prognosis of fat embolism in facial fat grafting is poor and there are no effective, evidence-based treatment options. Therefore, prevention is of utmost importance.1,12,15 Several preventive measures have been suggested in the literature, with a low level of evidence, many similar to prevention of complications of hyaluronic acid fillers. 30 All possible preventive measures are summarized in Table 1. Knowledge of the facial anatomy is paramount to avoid major blood vessels.31 Additionally, imaging and augmented reality could assist in vascular mapping before or during the procedure.32 Kadouch et al demonstrated this with duplex-ultrasound to improve safety of fat grafting in the temporal area.32 Although better survival of adipose tissue is assumed when injecting in a highly vascularized bed such as muscle, this also involves a higher risk of fat entering the bloodstream due to the larger vessels in the muscle.15 Avoiding fat grafting in traumatized areas should reduce the risk of intravasation.31 This would, for example, mean performing fat grafting before the face-lift. Local use of epinephrin causes vasoconstriction, reducing the risk of entering a blood vessel with the injection cannula or needle.31
| Knowledge and visualization of anatomy . |
|---|
| Avoid muscle |
| Avoid traumatized tissue |
| Epinephrine |
| Blunt cannulas |
| (Injection cannula diameter ≥ harvesting cannula diameter) |
| Small syringes |
| Pre-tunneling and wait |
| Multiple tunnels |
| Slow injection, pulling back |
| Low pressure |
| Small aliquots |
| Digital pressure proximal to injection |
| Knowledge and visualization of anatomy . |
|---|
| Avoid muscle |
| Avoid traumatized tissue |
| Epinephrine |
| Blunt cannulas |
| (Injection cannula diameter ≥ harvesting cannula diameter) |
| Small syringes |
| Pre-tunneling and wait |
| Multiple tunnels |
| Slow injection, pulling back |
| Low pressure |
| Small aliquots |
| Digital pressure proximal to injection |
| Knowledge and visualization of anatomy . |
|---|
| Avoid muscle |
| Avoid traumatized tissue |
| Epinephrine |
| Blunt cannulas |
| (Injection cannula diameter ≥ harvesting cannula diameter) |
| Small syringes |
| Pre-tunneling and wait |
| Multiple tunnels |
| Slow injection, pulling back |
| Low pressure |
| Small aliquots |
| Digital pressure proximal to injection |
| Knowledge and visualization of anatomy . |
|---|
| Avoid muscle |
| Avoid traumatized tissue |
| Epinephrine |
| Blunt cannulas |
| (Injection cannula diameter ≥ harvesting cannula diameter) |
| Small syringes |
| Pre-tunneling and wait |
| Multiple tunnels |
| Slow injection, pulling back |
| Low pressure |
| Small aliquots |
| Digital pressure proximal to injection |
To limit the likelihood of injecting into a vessel, blunt cannulas are recommended.13 The use of injection cannulas with a bore size equal to or larger than the harvesting cannula could prevent a build-up of pressure in the syringe due to obstruction with fat particles larger than the diameter of the injection cannula. The use of injection devices that only deliver small aliquots could help avoid a sudden increase of injected volume when a lower resistance is met, for example when a canula enters a blood vessel.13 We believe that, based on the research of Khan et al, if the aliquot injected is smaller than the volume needed to reach the internal carotid artery or retinal artery, severe complications might be avoided.14 The use of smaller syringes, preferably 0.5 to 1 mL, is recommended to lower the pressure required on the plunger.25
Multiple subcutaneous tunnels should be made to spread the volume of fat grafting. Waiting after making these tunnels allows hemostasis of injured blood vessels. The fat particles should be injected slowly and with low pressure whilst pulling the cannula or the needle back.13 When injecting in high-risk areas, digital pressure on the proximal part of blood vessels could obstruct the retrograde flow of intravasated fat. Tansatit et al have suggested trochlear compression for injections in the glabellar area.11 Despite all these measures, inadvertent intravascular injection may still occur.
Case Discussion
In all probability, the patient in the case we present suffered from microscopic fat embolism: there was a longer time interval between the procedure and onset of the symptoms and postmortem examination showed no obstruction of the cerebral circulation. There are multiple possible causes for intravasation of fat: fat grafting of the glabella and upper lip, bony resection of the frontal and mental bone, and liposuction from the abdomen. Both liposuction and bony surgery have been reported to cause fat embolism.17,33,34 Furthermore, the tissues that were fat grafted were probably already traumatized by the facial gender-confirmation surgery. We believe that, due to the absence of fat in the lungs, retrograde fat injection in the internal carotid artery is the most likely cause of the cerebral fat embolism and the ensuing death. According to our literature research, this is only the seventh case reported worldwide of fatal fat embolism after facial fat grafting.
Limitations
In the literature, over the course of 3 decades we found 49 cases with severe complications after autologous facial fat grafting. If we could compare this to the total number of these procedures, we would most likely conclude that these events are extremely rare. In plastic surgery there is an underreporting of adverse events.35-47 Evidence on these rare events can only be found in case reports and small case series. We assume that surgeons might not report cases of severe adverse advents, out of fear for their reputation and financial and time constraints. Most respected plastic surgery journals refer case reports to open access journals, which often require payment for publication, adding an extra financial barrier.
We therefore suspect that there is an underreporting of severe adverse advents during and after autologous facial fat grafting, giving surgeons a false belief of safety. No detailed operative report was made available. No imaging of cerebral perfusion was performed. Ascribing the cause of death to massive, microscopic fat embolism, as seen on the postmortem cerebral examination, is made by exclusion—no other possible causes of death were found.
CONCLUSIONS
Facial fat grafting is considered to be a safe procedure. However, we report a case resulting in death. Review of the literature indicates that severe complications of fat embolism after facial fat grafting are rare, but prognosis is poor and there are no effective treatment options. The increase in popularity of facial fat grafting means there is now an urgent need for awareness and prevention of adverse effects to improve safety. Suspected underreporting of these severe adverse events might give the surgeon a false belief of safety.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Presented at the European Association of Plastic Surgeons (EURAPS) 2017 in Pisa, Italy.



