-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Velthuis, Leonie Schelke, Sebastian Cotofana, Filler Anatomy, Aesthetic Surgery Journal, Volume 42, Issue 1, January 2022, Pages NP89–NP90, https://doi.org/10.1093/asj/sjab348
Close - Share Icon Share
Although human anatomy is universal, medical specialties have their own ways of approaching anatomy based on particular scientific and educational needs, hence terms such as cadaver anatomy, clinical anatomy, and surgical anatomy. Having delivered many training sessions of ultrasound imaging of the face, the authors gradually have reached the conclusion that “filler anatomy” differs from surgical anatomy or any other form of anatomical instruction.
Recently we published two articles on doppler ultrasound analysis of the face in cosmetic medicine in the Aesthetic Surgery Journal.1,2 Utilizing the standard positions given in part 1, clinicians may visualize clear reference structures from which the anatomy of that area of the face can be explored. In part 2, the courses of the major vascular structures in the face are described. This work focuses on translating cadaver anatomy to ultrasound images. This manner of employing ultrasound imaging may be helpful, for instance, in avoiding intra-arterial filler injections. Also knowing the exact location of the infraorbital foramen can help injectors avoid damage to the nerve. However, to optimize filler treatment strategies, other anatomical information should prevail, hence the term filler anatomy.
Understanding the layering of the tissues beneath the epidermis/dermis is of the utmost importance. The superficial musculo-aponeurotic system (SMAS) divides this space into superficial and deep compartments. Superficial to it are fat pads and smaller vascular structures. Deep to the SMAS are deep fat pads and various other structures such as muscles, the parotid gland, lymph nodes, and large arteries. Although filler injections into the superficial fat compartments are relatively routine, the thickness of this space may be limited. For instance, over the parotid gland it can be as small as 1 to 2 mm. The authors have seen numerous cases of hyaluronic acid deposits inside the parotid gland leading to clinical nodules with or without inflammation (Figure 1). Also, we have seen patients injected into the proper plane, the subcutis overlying to the parotid, but with a high G-prime hyaluronic acid substance, giving rise to unsightly nodules.
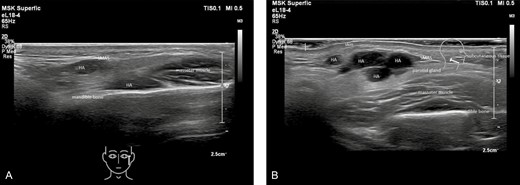
(A, B) Ultrasound images showing nodules in the parotid gland. HA, hyaluronic acid filler; SMAS, superficial musculo-aponeurotic system.
As for the structures deep to the SMAS, it is important to ensure the exact placement of the filler, whether in contact with bone or clearly above the bone. Furthermore, avoiding injecting inside a muscle may be important. We have observed that it is virtually impossible to avoid the masseter muscle when injecting deep on the lateral mandible. Subsequent muscle action can spread the material to unwanted sites. In contrast, injecting right under a muscle may render a positive myomodulation effect. We have shown that movement of the deep medial cheek fat pad during muscle activity is almost absent, whereas the superficial fat compartments regularly move back and forth.3 Filler injected deeply probably lasts longer and upon smiling and gives a much more natural effect. Because of the small size of the deep fat pad, injections should be performed under ultrasound guidance or after ultrasound verification. These examples highlight that the benefits of ultrasound imaging are a mix of improved safety and improved aesthetic outcome.
Ultrasound imaging has been utilized in cosmetic medicine only a few years; thus, there is more to learn about its potential of improving outcomes of soft tissue filler injections. To the authors, it is clear that ultrasound filler anatomy is not about the exact terminology of anatomical structures, but rather about recognition of the different echogenicities of fat, muscles, fibrous sheet, etc, and their subcutaneous orientation.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this letter.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES



