-
PDF
- Split View
-
Views
-
Cite
Cite
Joseph M Escandón, Krishna S Vyas, Oscar J Manrique, High-Definition Lipoplasty in Male Patients: A Systematic Review of Surgical Techniques and Outcomes, Aesthetic Surgery Journal, Volume 42, Issue 1, January 2022, Pages 68–85, https://doi.org/10.1093/asj/sjab300
Close - Share Icon Share
Abstract
Lipoplasty has undergone a series of refinements since its inception. It is now possible to apply superficial suction to enhance the outline of a muscle in order to improve the results of aesthetic lipoplasty.
The aim of this study was to summarize the available evidence on the techniques and surgical outcomes of high-definition lipoplasty (HDL) in male patients.
A systematic search across PubMed MEDLINE, Web of Science, Ovid MEDLINE In-Process & Other Non-Indexed Citations, and SCOPUS was performed in accordance with the PRISMA guidelines. Data regarding the surgical techniques, outcomes, and complications were extracted.
Thirteen studies comprising 1280 patients fulfilled the inclusion criteria. The age of patients ranged from 18 to 71 years. The average BMI was 26.5 kg/m2. The follow-up ranged from 2 weeks to 10 years. The liposculpting concepts reported were abdominal etching, high-definition, muscular sculpture, and dynamic definition. Four studies used conventional liposuction, 3 used VASER-assisted HDL, and 6 studies used power-assisted liposculpting. Eight studies reported the use of fat grafting. All studies reported the use of postoperative garments and a well-established wound treatment protocol. Overall satisfaction ranged from 84% to 100%. The most common complications reported were fluid collection, hyperpigmentation, contour irregularities, anemia, and port dehiscence.
A wide variety of techniques are available to perform HDL with a variable degree of definition. Careful patient selection is critical for successful results because HDL is not suitable for every patient. Finally, proper training and adequate knowledge of abdominal anatomy is necessary to avoid complications.

Since Schrudde et al in 1972 published preliminary reports in which subcutaneous fat was removed by means of sharp lipectomy assisted by uterine curettes, lipoplasty has undergone a series of refinements.1,2 Currently, we continue to adhere to the principles of blunt suction-assisted lipectomy (SAL) described by Arpad and Giorgio Fischer and further improved by Illouz and Fournier, who extended the application of liposuction to enable contouring of the whole body.1,3,4 Later, as pressure garments and infiltrating solutions with local anesthetic and epinephrine were employed, the problems of bleeding and prolonged recovery were overcome while expanding liposuction to several anatomic areas with more predictable results.5-7 In fact, it is now possible to apply superficial suction to improve the appearance of flaccid skin and to sculpt 3-dimensional shapes of muscular units by means of aesthetic lipoplasty.8-10
According to the Plastic Surgery Procedural Statistics of 2019 from the American Society of Plastic Surgeons (ASPS), liposuction is the second most common procedure performed in the United States and the third most common cosmetic surgery in male patients. In fact, cosmetic male liposuction has shown an increase of 3% in comparison to the previous year.11 Remarkably, since Mentz et al presented the technique of “abdominal etching” with the aim of enhancing the details of the anterior abdominal wall musculature through the use of differential liposuction, many techniques have being reported to provide liposuction with the aim of outlining the superficial abdominal anatomy with high definition.12-14 Therefore, the purpose of this study was to summarize the available literature on the methods used for aesthetic high-definition lipoplasty (HDL) in male patients in terms of surgical technique and outcomes.
METHODS
Systematic Literature Search
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.15,16 A review protocol was conceived and accepted by all authors a priori. A comprehensive search was conducted by J.M.E. across PubMed MEDLINE (United States National Library of Medicine, Bethesda, MD), Web of Science (Clarivate, Philadelphia, PA), SCOPUS (Elsevier, Amsterdam, the Netherlands), and Ovid MEDLINE In-Process & Other Non-Indexed Citations through February 2021 for the following Medical Subject Headings and keywords: “male,” “men,” “suction-assisted lipectomy,” “lipoabdominoplasty,” “body contouring,” “abdominal etching,” “high-definition liposuction,” “liposculpture,” and “abdominal body shaping” (Supplemental Table 1, available online at www.aestheticsurgeryjournal.com, displays the search strategy for the different databases).
Inclusion and Exclusion Criteria
Observational cohort studies, case-control studies, and case series reporting outcomes of HDL in cis-male patients for aesthetic indications written in English were included. Studies including transgender patients or solely reporting the management of gynecomastia, or chest or limb liposculpting were excluded. Preclinical studies, survey studies, conference presentations, abstracts, and case reports were also excluded.
Selection of Articles and Data Extraction
After removal of duplicates, a double-screening process was conducted by 2 reviewers (J.M.E. and O.J.M.). First, studies were reviewed based on title and abstract and then a full-text assessment was performed. The remaining studies fulfilling the inclusion criteria were incorporated into the following phase of data extraction. All discrepancies were resolved by consensus-forming discussions between the 2 investigators. The reference list of each study was inspected manually to identify relevant studies.
Data extraction was performed independently by 2 authors (J.M.E. and O.J.M.). Data regarding the author and year, number of patients, age, BMI, preoperative markings, tumescent solution, types of cannulas, liposuction technique, lipoaspirate volume, fat-grafting technique, closure of incisions, surgical outcomes and complications, postoperative wound treatment protocol, and follow-up were extracted. Cumulative estimates of the patients’ clinical and demographic characteristics were calculated as weighted means.
Quality Assessment
Two independent reviewers used the Oxford Centre for Evidence-Based Medicine (OCEBM) protocol to appraise the level of evidence of the included studies (Supplemental Table 2, available online at www.aestheticsurgeryjournal.com).17 The Newcastle-Ottawa Scale (NOS) was deemed suitable for evaluating the methodologic quality of cohort studies (Supplemental Table 3, available online at www.aestheticsurgeryjournal.com); and the tool for evaluating the methodological quality of case reports and case series (TMQCR/CS) developed by Murad et al was applied to assess the methodologic quality of case series (Supplemental Table 4, available online at www.aestheticsurgeryjournal.com).18,19 Disagreements were resolved through consultation with a third reviewer (K.S.V.).
RESULTS
Included Study Characteristics
The initial search provided 920 citations. After duplicates were removed, 744 articles were then screened for title and abstract. Subsequently, 77 articles were eligible for full-text review, from which 9 fulfilled the inclusion criteria and were prepared for qualitative analysis.1,9,10,12,20-24 Four additional studies were added manually after reviewing the reference lists and authors’ names of the included articles.25-28 A total of 13 studies were included in this systematic review (Figure 1).1,9,10,12,20-28 Four studies were case series, 6 were single-arm retrospective cohort studies, 2 were single-arm prospective cohort studies, and 1 was a 2-arm prospective cohort study. An overview of the characteristics of included studies is summarized in Table 1. Overall, 1284 male patients were included; only 1 study did not specify a sample size (7.6%). The mean age was not ubiquitously reported but ranged from 18 to 71 years. The average BMI was 26.5 kg/m2 (range, 18.8-38 kg/m2), reported in 5 studies (38.46%). The follow-up was reported in 11 studies (84.6%) and ranged from 2 weeks to 10 years.
| Author, year . | Location . | NOS . | OCEBM . | Patients (n) . | Age (years) . | BMI (gg/m2) . | Type of Study . | Observation period . |
|---|---|---|---|---|---|---|---|---|
| Mentz et al, 199312 | Houston, TX | 4∑ | 4 | 8 | 32 | NR | Case series | NR |
| Ersek and Salisbury, 19971 | Houston, TX | 3∑ | 4 | 2 | 29-30 | NR | Case series | NR |
| Hoyos and Millard, 20079 | Bogotá DC, Colombia | 5 | 4 | 33 | 18-65 | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Monarca and Rizzo, 201526 | Rome, Italy | 1 | 4 | NS | NR | NR | Single-center retrospective single-cohort | NR |
| Steinbrech and Sinno, 201628 | New York, NY | 3 | 4 | 43 | 22-58 | NR | Single-center retrospective single-cohort | 2013-2016 |
| Boeni, 202025 | Zurich, Switzerland | 4 | 4 | 48 | 43.8 (26-58) | NR | Single-center prospective single-cohort | 09/2018-08/2019 |
| Husain et al, 201921 | Miami, FL | 4 | 4 | 26 | 21-55 | 18.8-38 | Retrospective single-cohort | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Houston, TX | 5 | 4 | 512 | 39 (8-71) | NR | Single-center retrospective single-cohort | 01/2013-01/2017 |
| Niddam et al, 201922 | Créteil, France | 4∑ | 4 | 21 | 19-49 | 21 (19.1-25.8) | Single-center prospective case series | 01/2015-01/2017 |
| Saad et al, 202023 | San Diego, CA | 4∑ | 4 | 12 | 32.3 (27-38) | 26.4 (25.4-29) | Single-center prospective case series | 11/2017-11/2018 |
| Hoyos and Perez, 202037 | Bogotá DC, Colombia | 5 | 4 | 479 | 42.5 (23-69) | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Taha et al, 202024 | Cairo, Egypt | 5 | 4 | 50 | 36 (24-50) | 29 (28-33) | Prospective cohort | NR |
| Saad et al, 202127 | San Diego, CA | 5 | 4 | 50 | 37.34 (25-56) | 26.4 (24-30) | Single-center retrospective single-cohort | 01/2018-11/2019 |
| Author, year . | Location . | NOS . | OCEBM . | Patients (n) . | Age (years) . | BMI (gg/m2) . | Type of Study . | Observation period . |
|---|---|---|---|---|---|---|---|---|
| Mentz et al, 199312 | Houston, TX | 4∑ | 4 | 8 | 32 | NR | Case series | NR |
| Ersek and Salisbury, 19971 | Houston, TX | 3∑ | 4 | 2 | 29-30 | NR | Case series | NR |
| Hoyos and Millard, 20079 | Bogotá DC, Colombia | 5 | 4 | 33 | 18-65 | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Monarca and Rizzo, 201526 | Rome, Italy | 1 | 4 | NS | NR | NR | Single-center retrospective single-cohort | NR |
| Steinbrech and Sinno, 201628 | New York, NY | 3 | 4 | 43 | 22-58 | NR | Single-center retrospective single-cohort | 2013-2016 |
| Boeni, 202025 | Zurich, Switzerland | 4 | 4 | 48 | 43.8 (26-58) | NR | Single-center prospective single-cohort | 09/2018-08/2019 |
| Husain et al, 201921 | Miami, FL | 4 | 4 | 26 | 21-55 | 18.8-38 | Retrospective single-cohort | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Houston, TX | 5 | 4 | 512 | 39 (8-71) | NR | Single-center retrospective single-cohort | 01/2013-01/2017 |
| Niddam et al, 201922 | Créteil, France | 4∑ | 4 | 21 | 19-49 | 21 (19.1-25.8) | Single-center prospective case series | 01/2015-01/2017 |
| Saad et al, 202023 | San Diego, CA | 4∑ | 4 | 12 | 32.3 (27-38) | 26.4 (25.4-29) | Single-center prospective case series | 11/2017-11/2018 |
| Hoyos and Perez, 202037 | Bogotá DC, Colombia | 5 | 4 | 479 | 42.5 (23-69) | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Taha et al, 202024 | Cairo, Egypt | 5 | 4 | 50 | 36 (24-50) | 29 (28-33) | Prospective cohort | NR |
| Saad et al, 202127 | San Diego, CA | 5 | 4 | 50 | 37.34 (25-56) | 26.4 (24-30) | Single-center retrospective single-cohort | 01/2018-11/2019 |
NOS, Newcastle-Ottawa; NR, not reported; NS, not specified; OCEBM, Oxford Centre for Evidence-Based Medicine level of evidence. ∑, case series evaluated with the TMQCR/CS, a tool for evaluating the methodological quality of case reports and case series developed by Murad et al.19
| Author, year . | Location . | NOS . | OCEBM . | Patients (n) . | Age (years) . | BMI (gg/m2) . | Type of Study . | Observation period . |
|---|---|---|---|---|---|---|---|---|
| Mentz et al, 199312 | Houston, TX | 4∑ | 4 | 8 | 32 | NR | Case series | NR |
| Ersek and Salisbury, 19971 | Houston, TX | 3∑ | 4 | 2 | 29-30 | NR | Case series | NR |
| Hoyos and Millard, 20079 | Bogotá DC, Colombia | 5 | 4 | 33 | 18-65 | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Monarca and Rizzo, 201526 | Rome, Italy | 1 | 4 | NS | NR | NR | Single-center retrospective single-cohort | NR |
| Steinbrech and Sinno, 201628 | New York, NY | 3 | 4 | 43 | 22-58 | NR | Single-center retrospective single-cohort | 2013-2016 |
| Boeni, 202025 | Zurich, Switzerland | 4 | 4 | 48 | 43.8 (26-58) | NR | Single-center prospective single-cohort | 09/2018-08/2019 |
| Husain et al, 201921 | Miami, FL | 4 | 4 | 26 | 21-55 | 18.8-38 | Retrospective single-cohort | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Houston, TX | 5 | 4 | 512 | 39 (8-71) | NR | Single-center retrospective single-cohort | 01/2013-01/2017 |
| Niddam et al, 201922 | Créteil, France | 4∑ | 4 | 21 | 19-49 | 21 (19.1-25.8) | Single-center prospective case series | 01/2015-01/2017 |
| Saad et al, 202023 | San Diego, CA | 4∑ | 4 | 12 | 32.3 (27-38) | 26.4 (25.4-29) | Single-center prospective case series | 11/2017-11/2018 |
| Hoyos and Perez, 202037 | Bogotá DC, Colombia | 5 | 4 | 479 | 42.5 (23-69) | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Taha et al, 202024 | Cairo, Egypt | 5 | 4 | 50 | 36 (24-50) | 29 (28-33) | Prospective cohort | NR |
| Saad et al, 202127 | San Diego, CA | 5 | 4 | 50 | 37.34 (25-56) | 26.4 (24-30) | Single-center retrospective single-cohort | 01/2018-11/2019 |
| Author, year . | Location . | NOS . | OCEBM . | Patients (n) . | Age (years) . | BMI (gg/m2) . | Type of Study . | Observation period . |
|---|---|---|---|---|---|---|---|---|
| Mentz et al, 199312 | Houston, TX | 4∑ | 4 | 8 | 32 | NR | Case series | NR |
| Ersek and Salisbury, 19971 | Houston, TX | 3∑ | 4 | 2 | 29-30 | NR | Case series | NR |
| Hoyos and Millard, 20079 | Bogotá DC, Colombia | 5 | 4 | 33 | 18-65 | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Monarca and Rizzo, 201526 | Rome, Italy | 1 | 4 | NS | NR | NR | Single-center retrospective single-cohort | NR |
| Steinbrech and Sinno, 201628 | New York, NY | 3 | 4 | 43 | 22-58 | NR | Single-center retrospective single-cohort | 2013-2016 |
| Boeni, 202025 | Zurich, Switzerland | 4 | 4 | 48 | 43.8 (26-58) | NR | Single-center prospective single-cohort | 09/2018-08/2019 |
| Husain et al, 201921 | Miami, FL | 4 | 4 | 26 | 21-55 | 18.8-38 | Retrospective single-cohort | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Houston, TX | 5 | 4 | 512 | 39 (8-71) | NR | Single-center retrospective single-cohort | 01/2013-01/2017 |
| Niddam et al, 201922 | Créteil, France | 4∑ | 4 | 21 | 19-49 | 21 (19.1-25.8) | Single-center prospective case series | 01/2015-01/2017 |
| Saad et al, 202023 | San Diego, CA | 4∑ | 4 | 12 | 32.3 (27-38) | 26.4 (25.4-29) | Single-center prospective case series | 11/2017-11/2018 |
| Hoyos and Perez, 202037 | Bogotá DC, Colombia | 5 | 4 | 479 | 42.5 (23-69) | NR | Single-center retrospective single-cohort | 06/2013-09/2019 |
| Taha et al, 202024 | Cairo, Egypt | 5 | 4 | 50 | 36 (24-50) | 29 (28-33) | Prospective cohort | NR |
| Saad et al, 202127 | San Diego, CA | 5 | 4 | 50 | 37.34 (25-56) | 26.4 (24-30) | Single-center retrospective single-cohort | 01/2018-11/2019 |
NOS, Newcastle-Ottawa; NR, not reported; NS, not specified; OCEBM, Oxford Centre for Evidence-Based Medicine level of evidence. ∑, case series evaluated with the TMQCR/CS, a tool for evaluating the methodological quality of case reports and case series developed by Murad et al.19
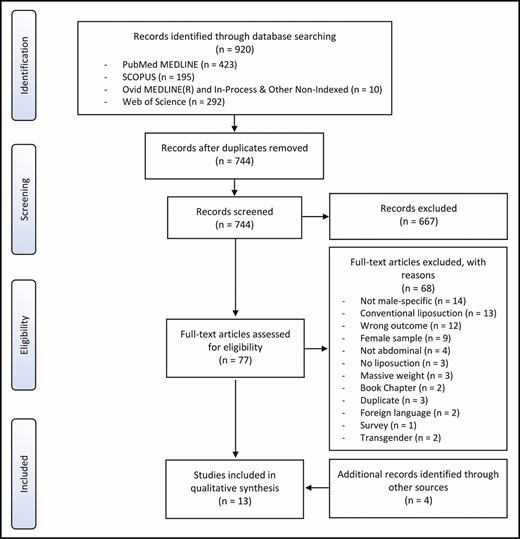
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Quality Assessment
The NOS and OCEBM scores are shown in Table 1. With the NOS instrument, 5 studies scored 5, 2 scored 4, 1 scored 3, and 1 scored 1 (Figure 2). Quality assessment with the TMQCR/CS resulted in 3 studies with a score of 4 and 1 scoring 3. All studies had a level of evidence of 4 according to the OCEBM protocol (100%) (Table 1).
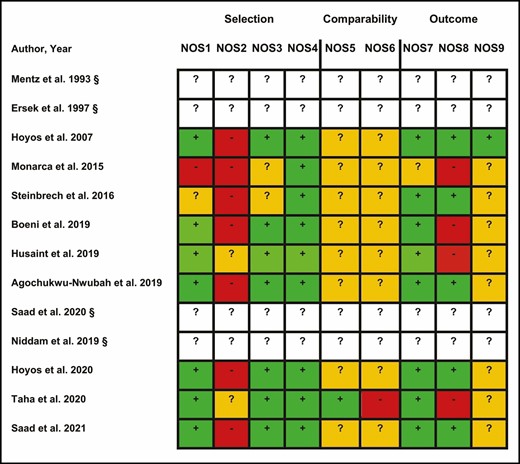
Quality assessment of observational studies with the Newcastle-Ottawa scale. §Case series evaluated with TMQCR/CS, a tool for evaluating the methodologic quality of case reports and case series developed by Murad et al.19
Surgical Planning
Preoperative markings were performed exclusively in the standing position in 10 studies, whereas 2 series reported preoperative markings performed in different positions.9,24 One study did not specify the patients’ position.26 Preoperative markings and surgical planning were limited to the linea alba, linea semilunaris, the flanks, and the transverse inscriptions of the rectus muscle in 6 studies (anterior abdominal wall).1,12,20-22,28 Preoperative markings beyond liposculpting of the anterior and lateral abdominal wall muscles were reported in 7 studies (Table 2). In these articles, liposculpting was performed over the abdomen, the chest (n = 5),9,10,23,24,27 upper and lower back (n = 6),9,10,23-25,27 gluteus and lower extremity (n = 4),10,23,26,27 and upper extremity (n = 6) (Table 2).9,10,23,25-27
Liposculpting Concept, Surgical Planning, and Preoperative Markings Described in Included Studies
| Author, year . | Concept . | Position . | Preoperative abdominal markings . | Additional locations . |
|---|---|---|---|---|
| Mentz et al, 199312 | Abdominal etching: differential liposuction | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle | NR/NS |
| Ersek and Salisbury, 19971 | Abdominal etching | StP | Two horizontal lines are chosen to create 2 nearly equal, distant planes, by bisecting the vertical line between the xiphoid and the umbilicus; etching is not applied beneath or at the level of the umbilicus | NR/NS |
| Hoyos et al, 20079 | VASER-assisted high-definition liposuction | SuP and StP | Serratus anterior, rectus abdominis, external oblique, iliac crest and inguinal ligaments and the relation between those structures | Pectoralis major and relation between other muscles; the V-shaped convexity over the inferior portion of the obliquus muscle in the back |
| Monarca and Rizzo, 201526 | Muscular sculpture | NR | Preoperative abdominal markings | Lines drawn over the deltoid and the arm muscles, and gluteal and lower extremity muscles |
| Steinbrech and Sinno, 201628 | Selective lipocontouring with PAL or standard SAL | StP | NR/NS | NR/NS |
| Boeni, 202025 | HDL | StP | As detailed by Hoyos and Millard, 20079 | Love handles and anterior border of the latissimus dorsi muscle up to the armpit; arms, the anterior and posterior definition lines between deltoid muscle and biceps, and the groove between the long head of the triceps and the triceps tendon |
| Husain et al, 201921 | PAL-assisted HDL | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle; iliac crest to create indentation lines, and any excessive flank lipodystrophy; serratus anterior lines for ultra-high definition. | Back, flanks, and thighs |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal etching: FAE, muscular “six-pack”; MAE, softer abdominal contour | StP | MAE: linea alba and linea semilunaris; FAE: transverse intersections or inscriptions of the rectus muscle + MAE | NR/NS |
| Niddam et al, 201922 | Abdominal etching | StP | Linea semilunaris and linea alba; transverse inscriptions of the rectus muscle; lateral oblique lines corresponding to the Apollo’s belt | NR/NS |
| Saad et al, 202023 | PAL-assisted HDL | StP | Delineate the underlying rectus abdominis anatomy; the iliac crests and ligaments were marked | Inferior horizontal and oblique lines of the pectoralis muscle; the groove between the deltoid and the biceps anteriorly and deltoid and triceps posteriorly; lateral border of the thoracolumbar fascia, the inferior border of the latissimus, and the superior border of the gluteus maximus |
| Hoyos and Perez, 202037 | Hoyos Dynamic Definition (HD2): Basic, Moderate, eXtreme | StP | Color code to mark the different zones and spaces that were to be treated with superficial and/or deep liposuction, and the smooth transition zones (standing position, allowing gravity and muscles to start in resting anatomic position); then, the patient contracted different muscles to mark specific “dynamic zones” and also negative spaces | |
| Taha et al, 202024 | HDL | DP | Areas to be treated were the waist and abdomen | Areas to be treated were over the back, upper back and chest |
| Saad et al, 202127 | HDL with PAL: MiD, 3-5 mm of fat; MoD, 5-7 mm of fat; HD, 7-9 mm of fata | StP | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 |
| Author, year . | Concept . | Position . | Preoperative abdominal markings . | Additional locations . |
|---|---|---|---|---|
| Mentz et al, 199312 | Abdominal etching: differential liposuction | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle | NR/NS |
| Ersek and Salisbury, 19971 | Abdominal etching | StP | Two horizontal lines are chosen to create 2 nearly equal, distant planes, by bisecting the vertical line between the xiphoid and the umbilicus; etching is not applied beneath or at the level of the umbilicus | NR/NS |
| Hoyos et al, 20079 | VASER-assisted high-definition liposuction | SuP and StP | Serratus anterior, rectus abdominis, external oblique, iliac crest and inguinal ligaments and the relation between those structures | Pectoralis major and relation between other muscles; the V-shaped convexity over the inferior portion of the obliquus muscle in the back |
| Monarca and Rizzo, 201526 | Muscular sculpture | NR | Preoperative abdominal markings | Lines drawn over the deltoid and the arm muscles, and gluteal and lower extremity muscles |
| Steinbrech and Sinno, 201628 | Selective lipocontouring with PAL or standard SAL | StP | NR/NS | NR/NS |
| Boeni, 202025 | HDL | StP | As detailed by Hoyos and Millard, 20079 | Love handles and anterior border of the latissimus dorsi muscle up to the armpit; arms, the anterior and posterior definition lines between deltoid muscle and biceps, and the groove between the long head of the triceps and the triceps tendon |
| Husain et al, 201921 | PAL-assisted HDL | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle; iliac crest to create indentation lines, and any excessive flank lipodystrophy; serratus anterior lines for ultra-high definition. | Back, flanks, and thighs |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal etching: FAE, muscular “six-pack”; MAE, softer abdominal contour | StP | MAE: linea alba and linea semilunaris; FAE: transverse intersections or inscriptions of the rectus muscle + MAE | NR/NS |
| Niddam et al, 201922 | Abdominal etching | StP | Linea semilunaris and linea alba; transverse inscriptions of the rectus muscle; lateral oblique lines corresponding to the Apollo’s belt | NR/NS |
| Saad et al, 202023 | PAL-assisted HDL | StP | Delineate the underlying rectus abdominis anatomy; the iliac crests and ligaments were marked | Inferior horizontal and oblique lines of the pectoralis muscle; the groove between the deltoid and the biceps anteriorly and deltoid and triceps posteriorly; lateral border of the thoracolumbar fascia, the inferior border of the latissimus, and the superior border of the gluteus maximus |
| Hoyos and Perez, 202037 | Hoyos Dynamic Definition (HD2): Basic, Moderate, eXtreme | StP | Color code to mark the different zones and spaces that were to be treated with superficial and/or deep liposuction, and the smooth transition zones (standing position, allowing gravity and muscles to start in resting anatomic position); then, the patient contracted different muscles to mark specific “dynamic zones” and also negative spaces | |
| Taha et al, 202024 | HDL | DP | Areas to be treated were the waist and abdomen | Areas to be treated were over the back, upper back and chest |
| Saad et al, 202127 | HDL with PAL: MiD, 3-5 mm of fat; MoD, 5-7 mm of fat; HD, 7-9 mm of fata | StP | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 |
DP, different positions; FAE, full abdominal etching; HDL, high-definition liposuction; MAE, modified abdominal etching; MiD, mild definition; MoD, moderate definition; NR, not recorded; NS, not specified; PAL, power-assisted lipectomy; SAL, suction-assisted lipectomy; StP, standing position; SuP, supine position.
aDifference in skin height and projection between the treated and untreated areas of the superficial fat layer.
Liposculpting Concept, Surgical Planning, and Preoperative Markings Described in Included Studies
| Author, year . | Concept . | Position . | Preoperative abdominal markings . | Additional locations . |
|---|---|---|---|---|
| Mentz et al, 199312 | Abdominal etching: differential liposuction | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle | NR/NS |
| Ersek and Salisbury, 19971 | Abdominal etching | StP | Two horizontal lines are chosen to create 2 nearly equal, distant planes, by bisecting the vertical line between the xiphoid and the umbilicus; etching is not applied beneath or at the level of the umbilicus | NR/NS |
| Hoyos et al, 20079 | VASER-assisted high-definition liposuction | SuP and StP | Serratus anterior, rectus abdominis, external oblique, iliac crest and inguinal ligaments and the relation between those structures | Pectoralis major and relation between other muscles; the V-shaped convexity over the inferior portion of the obliquus muscle in the back |
| Monarca and Rizzo, 201526 | Muscular sculpture | NR | Preoperative abdominal markings | Lines drawn over the deltoid and the arm muscles, and gluteal and lower extremity muscles |
| Steinbrech and Sinno, 201628 | Selective lipocontouring with PAL or standard SAL | StP | NR/NS | NR/NS |
| Boeni, 202025 | HDL | StP | As detailed by Hoyos and Millard, 20079 | Love handles and anterior border of the latissimus dorsi muscle up to the armpit; arms, the anterior and posterior definition lines between deltoid muscle and biceps, and the groove between the long head of the triceps and the triceps tendon |
| Husain et al, 201921 | PAL-assisted HDL | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle; iliac crest to create indentation lines, and any excessive flank lipodystrophy; serratus anterior lines for ultra-high definition. | Back, flanks, and thighs |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal etching: FAE, muscular “six-pack”; MAE, softer abdominal contour | StP | MAE: linea alba and linea semilunaris; FAE: transverse intersections or inscriptions of the rectus muscle + MAE | NR/NS |
| Niddam et al, 201922 | Abdominal etching | StP | Linea semilunaris and linea alba; transverse inscriptions of the rectus muscle; lateral oblique lines corresponding to the Apollo’s belt | NR/NS |
| Saad et al, 202023 | PAL-assisted HDL | StP | Delineate the underlying rectus abdominis anatomy; the iliac crests and ligaments were marked | Inferior horizontal and oblique lines of the pectoralis muscle; the groove between the deltoid and the biceps anteriorly and deltoid and triceps posteriorly; lateral border of the thoracolumbar fascia, the inferior border of the latissimus, and the superior border of the gluteus maximus |
| Hoyos and Perez, 202037 | Hoyos Dynamic Definition (HD2): Basic, Moderate, eXtreme | StP | Color code to mark the different zones and spaces that were to be treated with superficial and/or deep liposuction, and the smooth transition zones (standing position, allowing gravity and muscles to start in resting anatomic position); then, the patient contracted different muscles to mark specific “dynamic zones” and also negative spaces | |
| Taha et al, 202024 | HDL | DP | Areas to be treated were the waist and abdomen | Areas to be treated were over the back, upper back and chest |
| Saad et al, 202127 | HDL with PAL: MiD, 3-5 mm of fat; MoD, 5-7 mm of fat; HD, 7-9 mm of fata | StP | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 |
| Author, year . | Concept . | Position . | Preoperative abdominal markings . | Additional locations . |
|---|---|---|---|---|
| Mentz et al, 199312 | Abdominal etching: differential liposuction | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle | NR/NS |
| Ersek and Salisbury, 19971 | Abdominal etching | StP | Two horizontal lines are chosen to create 2 nearly equal, distant planes, by bisecting the vertical line between the xiphoid and the umbilicus; etching is not applied beneath or at the level of the umbilicus | NR/NS |
| Hoyos et al, 20079 | VASER-assisted high-definition liposuction | SuP and StP | Serratus anterior, rectus abdominis, external oblique, iliac crest and inguinal ligaments and the relation between those structures | Pectoralis major and relation between other muscles; the V-shaped convexity over the inferior portion of the obliquus muscle in the back |
| Monarca and Rizzo, 201526 | Muscular sculpture | NR | Preoperative abdominal markings | Lines drawn over the deltoid and the arm muscles, and gluteal and lower extremity muscles |
| Steinbrech and Sinno, 201628 | Selective lipocontouring with PAL or standard SAL | StP | NR/NS | NR/NS |
| Boeni, 202025 | HDL | StP | As detailed by Hoyos and Millard, 20079 | Love handles and anterior border of the latissimus dorsi muscle up to the armpit; arms, the anterior and posterior definition lines between deltoid muscle and biceps, and the groove between the long head of the triceps and the triceps tendon |
| Husain et al, 201921 | PAL-assisted HDL | StP | Linea alba and linea semilunaris; transverse inscriptions of the rectus muscle; iliac crest to create indentation lines, and any excessive flank lipodystrophy; serratus anterior lines for ultra-high definition. | Back, flanks, and thighs |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal etching: FAE, muscular “six-pack”; MAE, softer abdominal contour | StP | MAE: linea alba and linea semilunaris; FAE: transverse intersections or inscriptions of the rectus muscle + MAE | NR/NS |
| Niddam et al, 201922 | Abdominal etching | StP | Linea semilunaris and linea alba; transverse inscriptions of the rectus muscle; lateral oblique lines corresponding to the Apollo’s belt | NR/NS |
| Saad et al, 202023 | PAL-assisted HDL | StP | Delineate the underlying rectus abdominis anatomy; the iliac crests and ligaments were marked | Inferior horizontal and oblique lines of the pectoralis muscle; the groove between the deltoid and the biceps anteriorly and deltoid and triceps posteriorly; lateral border of the thoracolumbar fascia, the inferior border of the latissimus, and the superior border of the gluteus maximus |
| Hoyos and Perez, 202037 | Hoyos Dynamic Definition (HD2): Basic, Moderate, eXtreme | StP | Color code to mark the different zones and spaces that were to be treated with superficial and/or deep liposuction, and the smooth transition zones (standing position, allowing gravity and muscles to start in resting anatomic position); then, the patient contracted different muscles to mark specific “dynamic zones” and also negative spaces | |
| Taha et al, 202024 | HDL | DP | Areas to be treated were the waist and abdomen | Areas to be treated were over the back, upper back and chest |
| Saad et al, 202127 | HDL with PAL: MiD, 3-5 mm of fat; MoD, 5-7 mm of fat; HD, 7-9 mm of fata | StP | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 |
DP, different positions; FAE, full abdominal etching; HDL, high-definition liposuction; MAE, modified abdominal etching; MiD, mild definition; MoD, moderate definition; NR, not recorded; NS, not specified; PAL, power-assisted lipectomy; SAL, suction-assisted lipectomy; StP, standing position; SuP, supine position.
aDifference in skin height and projection between the treated and untreated areas of the superficial fat layer.
Liposculpting Concept
Abdominal Etching
Mentz et al and Niddam et al used differential lipoplasty to detail the abdominal musculature, specifically the rectus abdominis muscles, between the linea alba and the linea semilunaris, while also addressing the horizontal tendinous inscriptions.12,22 This concept was limited to patients with a low total body fat percentage (≤15%).9 Ersek et al performed conventional liposuction to generate a smooth and even contour of the abdomen and flanks. Precision etching was then performed with a special semisharp beveled cannula over the tendinous inscriptions and linea alba above the umbilicus until a defatted groove was noted (Figure 3).1

Abdominal etching (blue, debulking; yellow, superficial fat liposculpting).
Agochukwu-Nwubah and Mentz described a “modified abdominal etching” and a “full abdominal etching” technique. Both techniques were performed to detail the abdominal musculature but the latter involved a more aggressive deep and superficial liposuction performed along the linea semilunaris and over the transverse rectus inscriptions in comparison to the former (Table 2).20
HDL
Initially presented by Hoyos, HDL elevated the concept of abdominal etching to a 3-dimensional approach encompassing the impact of other muscle groups and the effect of bony structures over the superficial anatomy to integrate the entire torso, the arms, legs, and back (Figure 4).9,23-25,27 In this approach, the concept of body contouring by sectors was abolished and liposuction was also extended to patients with a higher percentage of total body fat (>15%).9

High-definition liposculpting (blue, debulking; yellow, superficial fat liposculpting).
Saad et al proposed a classification of 3 levels of definition based on the extent of superficial fat liposculpting, and the difference in skin height and projection between treated and untreated areas of the superficial fat layer. These classifications were as follows: mild definition (MiD), 3 to 5 mm; moderate definition (MoD), 5 to 7 mm; and high definition (HD), 7 to 9 mm.27
Monarca and Rizzo reported a muscle sculpture technique that extrapolated concepts of HDL to overweight and previously obese patients. This technique also included excision of subcutaneous tissue and fat grafting selectively to muscles when increased volume was desired, giving a bodybuilder-like effect (Table 2).26
Dynamic Definition
The Hoyos Dynamic Definition (HD2) technique involves the aforementioned principles of HDL. However, the dynamic component incorporates a muscular definition that follows the pattern of particular muscle movements by creating “dynamic zones” at specific anatomic landmarks, predicting the form of the muscles in motion (Figure 5). Therefore, with HD2, multilayer liposuction and fat grafting were based on muscular motion and biomechanics.10 In addition, HD2 takes into consideration the natural succession of the body sculpting process of muscular units and the different anatomic groups (endomorph, ectomorph and mesomorph) to choose an adequate treatment plan according to the BMX (Basic, Moderate, eXtreme) algorithm (Table 2).10

Color-based anatomic-topographic concept of variable degrees of dynamic definition according to the BMX (Basic, Moderate, eXtreme) algorithm (blue, basic; yellow, moderate; red, extreme).
Incisions and Infiltration Solution
An overview of the incisions performed for liposculpting and the use of infiltrating solution is shown in Table 3. Four studies used tumescent solution with diluted epinephrine,9,10,22,26 whereas 9 studies used tumescent solution diluted with local anesthetic and epinephrine. The amount of tumescent fluid injected was reported in 4 studies and ranged from 300 to 14,400 mL.10,20,21,25 The infiltration-aspiration ratio ranged from 1:1 to 2:1, reported in 3 studies.9,10,20 Remarkably, Hoyos and Millard reported a detailed infiltration in areas with skin laxity and areas that were treated more superficially (Table 3).9
Equipment, Anatomic Location of Incision and Ports, and Details of the Infiltrating Solution
| Author, year . | Cannula and equipment . | Punctures . | Infiltration solution . |
|---|---|---|---|
| Mentz et al, 199312 | 2- or 3-mm flat Becker-style liposuction cannula; small Mercedes cannula (1.5-2.5 mm) | Pubic hair at the lateral edge of the rectus and at the midline (n = 3); umbilical (n = 1) and in the midline at the upper two rectus inscriptions (n = 2) | Pressure infusion technique: 1 L of normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; 15-min delay was allocated for vasoconstriction |
| Ersek and Salisbury, 19971 | Custom-designed suction cannula 3 mm in diameter, 35 cm in length, with a beveled (semi-sharp) tip; 4- or 5-mm diameter cannulas | Escutcheon incisions in the pubic area (n = 2); umbilicus superiorly (n = 1); 5 cm beyond the extremes of the planned horizontal lines (n = 2) | Solution of 0.18% lidocaine with epinephrine |
| Hoyos and Millard, 20079 | VASER lipoplasty; atraumatic VentX cannulas (Sound Surgical Technologies, Louisville, CO), 3.7- or 2.9-mm 3-groove probe or 3.7-mm 1-groove probe | NR | 1000 mL of normal saline and 1 ampule of epinephrine 1:1000; superficial and deep infiltration; infiltration-aspiration ratio 1.5-2:1; detailed infiltration in areas with skin laxity and that required more superficial work |
| Monarca and Rizzo, 201526 | Basket/accelerator cannulas | NR | Saline and adrenaline |
| Steinbrech and Sinno, 201628 | PAL (MicroAire Inc., Charlottesville, VA) | Underwear line (n = 3), “hidden” umbilical incisions (n = 4), under the nipples (n = 2), upper gluteal crease (n = 2), lateral incision (n = 2) | 0.9% saline with lidocaine 0.1% and epinephrine 1:1,100,000; the tumescent solution is given 10 minutes to take effect |
| Boeni, 202025 | Interconnected flow system with four 28-gauge needles (Vacuson 60 LP, Erlangen, Germany) for infiltration; PAL (MicroAire Inc., Charlottesville, VA) with Mercedes cannula | 3-mm incisions: mons pubis area at the lateral edge of the rectus (n = 2); umbilical puncture (n = 1); anterior armpit crease (n = 2) | Saline, adrenaline, lidocaine (300 mg/L), and prilocaine (250 mg/L); tumescent fluid: 9400 mL (range, 6800-12,000 mL) |
| Husain et al, 201921 | PAL with a blunt-tip cannula (no. 4 or 5); no. 5 Mercedes cannula for deep layers | Superior to umbilicus (n = 1); lower abdominal crease along the linea alba and semilunaris lines (n = 3); lateral incisions (n = 2); “hidden” umbilical incisions (n = 4); under the nipples (n = 2) | 30 mL of 1% lidocaine plus 1000 mL of normal saline plus 1 mL of 1:1000 epinephrine; the tumescent solution is given 10 minutes to take effect; tumescent fluid: range, 2700-11,000 mL |
| Agochukwu-Nwubah and Mentz, 201920 | Small Mercedes cannula; superficial and deep liposuction with 4- and/or 5-mm basket cannula; larger cannula can be used if the tissue is more fibrous. | Pubis (n = 3) (one central and two lateral); inferior border of the NAC (n = 2); patients undergoing pectoral etching, additional ports are positioned at each axilla | 1000 mL normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; supersweet technique is usually used (1:1 ratio of tumescent injected:aspirate); 15 minutes for epinephrine-induced vasoconstriction; tumescent fluid: 4681 mL (range, 300-5700 mL) |
| Saad et al, 202023 | PAL system (MicroAire Inc., Charlottesville, VA); fat harvest and superficial liposculpting were done by means of bent and straight 5-mm flared Mercedes cannulas (MicroAire) | 5-mm supragluteal region incisions (n = 2); 5-mm posterior axillary fold incisions (n = 2); medial inguinal in the suprapubic region (n = 2); umbilicus, NAC below the nipple (n = 2); axillary crease along the anterior axillary line (n = 2) | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Niddam et al, 201922 | 4-mm 3-hole cannula | Lateral pubic incisions (n = 2); xiphoidal incision (n = 1); lateral incisions (n = 2) | 2 mg of epinephrine in 1000 mL of saline |
| Hoyos and Perez, 202037 | VASER lipoplasty; 4.0 and 3.0 mm connected to PowerX (2018 Solta Medical - Bausch Health Companies, Inc., Raleigh, NC) or Microaire (2019 MicroAire Surgical Instruments, LLC, Charlottesville, VA) | NR | 1000 mL of saline and 1 mL of epinephrine 1:1000; ratio of infiltration/total lipoaspirate volume of approximately 2:1 to 1.5:1; ~20-30 minutes sufficient for vasoconstriction; infiltration: range, 1200-14,400 mL |
| Taha et al, 202024 | NR | NR | 20 mL of 2% xylocaine and 1 mg of 1 mL epinephrine for each 1 L of normal saline |
| Saad et al, 202127 | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Author, year . | Cannula and equipment . | Punctures . | Infiltration solution . |
|---|---|---|---|
| Mentz et al, 199312 | 2- or 3-mm flat Becker-style liposuction cannula; small Mercedes cannula (1.5-2.5 mm) | Pubic hair at the lateral edge of the rectus and at the midline (n = 3); umbilical (n = 1) and in the midline at the upper two rectus inscriptions (n = 2) | Pressure infusion technique: 1 L of normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; 15-min delay was allocated for vasoconstriction |
| Ersek and Salisbury, 19971 | Custom-designed suction cannula 3 mm in diameter, 35 cm in length, with a beveled (semi-sharp) tip; 4- or 5-mm diameter cannulas | Escutcheon incisions in the pubic area (n = 2); umbilicus superiorly (n = 1); 5 cm beyond the extremes of the planned horizontal lines (n = 2) | Solution of 0.18% lidocaine with epinephrine |
| Hoyos and Millard, 20079 | VASER lipoplasty; atraumatic VentX cannulas (Sound Surgical Technologies, Louisville, CO), 3.7- or 2.9-mm 3-groove probe or 3.7-mm 1-groove probe | NR | 1000 mL of normal saline and 1 ampule of epinephrine 1:1000; superficial and deep infiltration; infiltration-aspiration ratio 1.5-2:1; detailed infiltration in areas with skin laxity and that required more superficial work |
| Monarca and Rizzo, 201526 | Basket/accelerator cannulas | NR | Saline and adrenaline |
| Steinbrech and Sinno, 201628 | PAL (MicroAire Inc., Charlottesville, VA) | Underwear line (n = 3), “hidden” umbilical incisions (n = 4), under the nipples (n = 2), upper gluteal crease (n = 2), lateral incision (n = 2) | 0.9% saline with lidocaine 0.1% and epinephrine 1:1,100,000; the tumescent solution is given 10 minutes to take effect |
| Boeni, 202025 | Interconnected flow system with four 28-gauge needles (Vacuson 60 LP, Erlangen, Germany) for infiltration; PAL (MicroAire Inc., Charlottesville, VA) with Mercedes cannula | 3-mm incisions: mons pubis area at the lateral edge of the rectus (n = 2); umbilical puncture (n = 1); anterior armpit crease (n = 2) | Saline, adrenaline, lidocaine (300 mg/L), and prilocaine (250 mg/L); tumescent fluid: 9400 mL (range, 6800-12,000 mL) |
| Husain et al, 201921 | PAL with a blunt-tip cannula (no. 4 or 5); no. 5 Mercedes cannula for deep layers | Superior to umbilicus (n = 1); lower abdominal crease along the linea alba and semilunaris lines (n = 3); lateral incisions (n = 2); “hidden” umbilical incisions (n = 4); under the nipples (n = 2) | 30 mL of 1% lidocaine plus 1000 mL of normal saline plus 1 mL of 1:1000 epinephrine; the tumescent solution is given 10 minutes to take effect; tumescent fluid: range, 2700-11,000 mL |
| Agochukwu-Nwubah and Mentz, 201920 | Small Mercedes cannula; superficial and deep liposuction with 4- and/or 5-mm basket cannula; larger cannula can be used if the tissue is more fibrous. | Pubis (n = 3) (one central and two lateral); inferior border of the NAC (n = 2); patients undergoing pectoral etching, additional ports are positioned at each axilla | 1000 mL normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; supersweet technique is usually used (1:1 ratio of tumescent injected:aspirate); 15 minutes for epinephrine-induced vasoconstriction; tumescent fluid: 4681 mL (range, 300-5700 mL) |
| Saad et al, 202023 | PAL system (MicroAire Inc., Charlottesville, VA); fat harvest and superficial liposculpting were done by means of bent and straight 5-mm flared Mercedes cannulas (MicroAire) | 5-mm supragluteal region incisions (n = 2); 5-mm posterior axillary fold incisions (n = 2); medial inguinal in the suprapubic region (n = 2); umbilicus, NAC below the nipple (n = 2); axillary crease along the anterior axillary line (n = 2) | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Niddam et al, 201922 | 4-mm 3-hole cannula | Lateral pubic incisions (n = 2); xiphoidal incision (n = 1); lateral incisions (n = 2) | 2 mg of epinephrine in 1000 mL of saline |
| Hoyos and Perez, 202037 | VASER lipoplasty; 4.0 and 3.0 mm connected to PowerX (2018 Solta Medical - Bausch Health Companies, Inc., Raleigh, NC) or Microaire (2019 MicroAire Surgical Instruments, LLC, Charlottesville, VA) | NR | 1000 mL of saline and 1 mL of epinephrine 1:1000; ratio of infiltration/total lipoaspirate volume of approximately 2:1 to 1.5:1; ~20-30 minutes sufficient for vasoconstriction; infiltration: range, 1200-14,400 mL |
| Taha et al, 202024 | NR | NR | 20 mL of 2% xylocaine and 1 mg of 1 mL epinephrine for each 1 L of normal saline |
| Saad et al, 202127 | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
NAC, nipple-areola complex; NR, not reported; PAL, power-assisted lipectomy; VASER, vibration amplification of sound energy at resonance.
Equipment, Anatomic Location of Incision and Ports, and Details of the Infiltrating Solution
| Author, year . | Cannula and equipment . | Punctures . | Infiltration solution . |
|---|---|---|---|
| Mentz et al, 199312 | 2- or 3-mm flat Becker-style liposuction cannula; small Mercedes cannula (1.5-2.5 mm) | Pubic hair at the lateral edge of the rectus and at the midline (n = 3); umbilical (n = 1) and in the midline at the upper two rectus inscriptions (n = 2) | Pressure infusion technique: 1 L of normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; 15-min delay was allocated for vasoconstriction |
| Ersek and Salisbury, 19971 | Custom-designed suction cannula 3 mm in diameter, 35 cm in length, with a beveled (semi-sharp) tip; 4- or 5-mm diameter cannulas | Escutcheon incisions in the pubic area (n = 2); umbilicus superiorly (n = 1); 5 cm beyond the extremes of the planned horizontal lines (n = 2) | Solution of 0.18% lidocaine with epinephrine |
| Hoyos and Millard, 20079 | VASER lipoplasty; atraumatic VentX cannulas (Sound Surgical Technologies, Louisville, CO), 3.7- or 2.9-mm 3-groove probe or 3.7-mm 1-groove probe | NR | 1000 mL of normal saline and 1 ampule of epinephrine 1:1000; superficial and deep infiltration; infiltration-aspiration ratio 1.5-2:1; detailed infiltration in areas with skin laxity and that required more superficial work |
| Monarca and Rizzo, 201526 | Basket/accelerator cannulas | NR | Saline and adrenaline |
| Steinbrech and Sinno, 201628 | PAL (MicroAire Inc., Charlottesville, VA) | Underwear line (n = 3), “hidden” umbilical incisions (n = 4), under the nipples (n = 2), upper gluteal crease (n = 2), lateral incision (n = 2) | 0.9% saline with lidocaine 0.1% and epinephrine 1:1,100,000; the tumescent solution is given 10 minutes to take effect |
| Boeni, 202025 | Interconnected flow system with four 28-gauge needles (Vacuson 60 LP, Erlangen, Germany) for infiltration; PAL (MicroAire Inc., Charlottesville, VA) with Mercedes cannula | 3-mm incisions: mons pubis area at the lateral edge of the rectus (n = 2); umbilical puncture (n = 1); anterior armpit crease (n = 2) | Saline, adrenaline, lidocaine (300 mg/L), and prilocaine (250 mg/L); tumescent fluid: 9400 mL (range, 6800-12,000 mL) |
| Husain et al, 201921 | PAL with a blunt-tip cannula (no. 4 or 5); no. 5 Mercedes cannula for deep layers | Superior to umbilicus (n = 1); lower abdominal crease along the linea alba and semilunaris lines (n = 3); lateral incisions (n = 2); “hidden” umbilical incisions (n = 4); under the nipples (n = 2) | 30 mL of 1% lidocaine plus 1000 mL of normal saline plus 1 mL of 1:1000 epinephrine; the tumescent solution is given 10 minutes to take effect; tumescent fluid: range, 2700-11,000 mL |
| Agochukwu-Nwubah and Mentz, 201920 | Small Mercedes cannula; superficial and deep liposuction with 4- and/or 5-mm basket cannula; larger cannula can be used if the tissue is more fibrous. | Pubis (n = 3) (one central and two lateral); inferior border of the NAC (n = 2); patients undergoing pectoral etching, additional ports are positioned at each axilla | 1000 mL normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; supersweet technique is usually used (1:1 ratio of tumescent injected:aspirate); 15 minutes for epinephrine-induced vasoconstriction; tumescent fluid: 4681 mL (range, 300-5700 mL) |
| Saad et al, 202023 | PAL system (MicroAire Inc., Charlottesville, VA); fat harvest and superficial liposculpting were done by means of bent and straight 5-mm flared Mercedes cannulas (MicroAire) | 5-mm supragluteal region incisions (n = 2); 5-mm posterior axillary fold incisions (n = 2); medial inguinal in the suprapubic region (n = 2); umbilicus, NAC below the nipple (n = 2); axillary crease along the anterior axillary line (n = 2) | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Niddam et al, 201922 | 4-mm 3-hole cannula | Lateral pubic incisions (n = 2); xiphoidal incision (n = 1); lateral incisions (n = 2) | 2 mg of epinephrine in 1000 mL of saline |
| Hoyos and Perez, 202037 | VASER lipoplasty; 4.0 and 3.0 mm connected to PowerX (2018 Solta Medical - Bausch Health Companies, Inc., Raleigh, NC) or Microaire (2019 MicroAire Surgical Instruments, LLC, Charlottesville, VA) | NR | 1000 mL of saline and 1 mL of epinephrine 1:1000; ratio of infiltration/total lipoaspirate volume of approximately 2:1 to 1.5:1; ~20-30 minutes sufficient for vasoconstriction; infiltration: range, 1200-14,400 mL |
| Taha et al, 202024 | NR | NR | 20 mL of 2% xylocaine and 1 mg of 1 mL epinephrine for each 1 L of normal saline |
| Saad et al, 202127 | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Author, year . | Cannula and equipment . | Punctures . | Infiltration solution . |
|---|---|---|---|
| Mentz et al, 199312 | 2- or 3-mm flat Becker-style liposuction cannula; small Mercedes cannula (1.5-2.5 mm) | Pubic hair at the lateral edge of the rectus and at the midline (n = 3); umbilical (n = 1) and in the midline at the upper two rectus inscriptions (n = 2) | Pressure infusion technique: 1 L of normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; 15-min delay was allocated for vasoconstriction |
| Ersek and Salisbury, 19971 | Custom-designed suction cannula 3 mm in diameter, 35 cm in length, with a beveled (semi-sharp) tip; 4- or 5-mm diameter cannulas | Escutcheon incisions in the pubic area (n = 2); umbilicus superiorly (n = 1); 5 cm beyond the extremes of the planned horizontal lines (n = 2) | Solution of 0.18% lidocaine with epinephrine |
| Hoyos and Millard, 20079 | VASER lipoplasty; atraumatic VentX cannulas (Sound Surgical Technologies, Louisville, CO), 3.7- or 2.9-mm 3-groove probe or 3.7-mm 1-groove probe | NR | 1000 mL of normal saline and 1 ampule of epinephrine 1:1000; superficial and deep infiltration; infiltration-aspiration ratio 1.5-2:1; detailed infiltration in areas with skin laxity and that required more superficial work |
| Monarca and Rizzo, 201526 | Basket/accelerator cannulas | NR | Saline and adrenaline |
| Steinbrech and Sinno, 201628 | PAL (MicroAire Inc., Charlottesville, VA) | Underwear line (n = 3), “hidden” umbilical incisions (n = 4), under the nipples (n = 2), upper gluteal crease (n = 2), lateral incision (n = 2) | 0.9% saline with lidocaine 0.1% and epinephrine 1:1,100,000; the tumescent solution is given 10 minutes to take effect |
| Boeni, 202025 | Interconnected flow system with four 28-gauge needles (Vacuson 60 LP, Erlangen, Germany) for infiltration; PAL (MicroAire Inc., Charlottesville, VA) with Mercedes cannula | 3-mm incisions: mons pubis area at the lateral edge of the rectus (n = 2); umbilical puncture (n = 1); anterior armpit crease (n = 2) | Saline, adrenaline, lidocaine (300 mg/L), and prilocaine (250 mg/L); tumescent fluid: 9400 mL (range, 6800-12,000 mL) |
| Husain et al, 201921 | PAL with a blunt-tip cannula (no. 4 or 5); no. 5 Mercedes cannula for deep layers | Superior to umbilicus (n = 1); lower abdominal crease along the linea alba and semilunaris lines (n = 3); lateral incisions (n = 2); “hidden” umbilical incisions (n = 4); under the nipples (n = 2) | 30 mL of 1% lidocaine plus 1000 mL of normal saline plus 1 mL of 1:1000 epinephrine; the tumescent solution is given 10 minutes to take effect; tumescent fluid: range, 2700-11,000 mL |
| Agochukwu-Nwubah and Mentz, 201920 | Small Mercedes cannula; superficial and deep liposuction with 4- and/or 5-mm basket cannula; larger cannula can be used if the tissue is more fibrous. | Pubis (n = 3) (one central and two lateral); inferior border of the NAC (n = 2); patients undergoing pectoral etching, additional ports are positioned at each axilla | 1000 mL normal saline with 1 mL of 1:1000 epinephrine and 50 mL of 1% lidocaine; supersweet technique is usually used (1:1 ratio of tumescent injected:aspirate); 15 minutes for epinephrine-induced vasoconstriction; tumescent fluid: 4681 mL (range, 300-5700 mL) |
| Saad et al, 202023 | PAL system (MicroAire Inc., Charlottesville, VA); fat harvest and superficial liposculpting were done by means of bent and straight 5-mm flared Mercedes cannulas (MicroAire) | 5-mm supragluteal region incisions (n = 2); 5-mm posterior axillary fold incisions (n = 2); medial inguinal in the suprapubic region (n = 2); umbilicus, NAC below the nipple (n = 2); axillary crease along the anterior axillary line (n = 2) | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
| Niddam et al, 201922 | 4-mm 3-hole cannula | Lateral pubic incisions (n = 2); xiphoidal incision (n = 1); lateral incisions (n = 2) | 2 mg of epinephrine in 1000 mL of saline |
| Hoyos and Perez, 202037 | VASER lipoplasty; 4.0 and 3.0 mm connected to PowerX (2018 Solta Medical - Bausch Health Companies, Inc., Raleigh, NC) or Microaire (2019 MicroAire Surgical Instruments, LLC, Charlottesville, VA) | NR | 1000 mL of saline and 1 mL of epinephrine 1:1000; ratio of infiltration/total lipoaspirate volume of approximately 2:1 to 1.5:1; ~20-30 minutes sufficient for vasoconstriction; infiltration: range, 1200-14,400 mL |
| Taha et al, 202024 | NR | NR | 20 mL of 2% xylocaine and 1 mg of 1 mL epinephrine for each 1 L of normal saline |
| Saad et al, 202127 | As detailed by Saad et al, 202023 | As detailed by Saad et al, 202023 | 1000 mL of 0.9% NaCl, 20 mL of 1% lidocaine, 1 mL (1:1000) epinephrine |
NAC, nipple-areola complex; NR, not reported; PAL, power-assisted lipectomy; VASER, vibration amplification of sound energy at resonance.
Surgical Technique and Technology
VASER-Assisted HDL
Hoyos et al reported an initial stage of fat emulsification. After the wetting solution was infiltrated, the superficial subcutaneous fat was treated in VASER (vibration amplification of sound energy at resonance) mode with a 2.9- or 3.7-mm, 3- or 2-grooved probe using an amplitude of 80% (Solta Medical, Bothell, WA).9,10 Energy was augmented to 90% or an alternative probe was selected if unwarranted resistance was experienced. Then, continuous mode was used to emulsify the deeper fat.10 The duration of VASER treatment was 60 to 90 seconds per 100 mL of infiltration.10 Taha et al reported emulsifying fat with VASER at 70% in pulsed mode immediately after infiltration of the wetting solution (Table 4).24
| Author, year . | Anatomic concept (treated areas) . | Step 1 . | Step 2 . | Step 3 . |
|---|---|---|---|---|
| Mentz et al, 199312 | Anterior abdominal wall: linea alba and linea semi-lunaris; transverse intersections or inscriptions of the rectus muscle | 2- or 3-mm flat Becker-style liposuction cannula was used for superficial liposuction in the marked areas, first with the openings facing the skin, then with the openings facing the muscular surface | A groove was created to the desired depth; superficial liposuction was continued at the marked areas until there was apparent furrowing or deepening of the natural crease | Deep liposuction with a small Mercedes cannula (1.5-2.5 mm), leaving a thicker fat pad in the islands where muscular enhancement was necessary |
| Ersek and Salisbury, 19971 | Abdomen and flanks | Custom-designed 3-mm suction cannula is passed in the same channel many times to create a completely defatted groove; a new etched abdomen is obvious at the end of the procedure | NR | NR |
| Hoyos and Millard, 20079 | Areas with large fat deposits; back and posterior arms; inner thighs, waist, and neck; linea alba and its tendinous insertions, the pectoral inferior line, inguinal ligament | Emulsification: VASER: 1 minute/100 mL of infiltration, the clinical endpoint was the loss of resistance; large fat deposits were treated with a 3.7- or 2.9-mm 3-groove probe, 80% power (continuous mode); back and posterior arms were treated with a 3.7-mm 1-groove probe (continuous mode); skin or delicate areas, were treated with a 2.9-mm 3-groove probe, 60% power (pulsed mode). differential emulsification for each muscle group: superficial emulsification with a 2.9-mm 3-groove probe (pulse mode) | Debulking: areas of fat deposits in the deep layer, with 3.7- or 4.6-mm cannulas, and continued in the midlamellar layer and between muscle groups, avoiding aspiration against the delicate subdermal layer; superficial emulsification and extraction in the subdermal lamellar layer selectively over the muscular frame with a 2.9-mm probe for emulsification and a 3.0-mm cannula for aspiration | Transitioning: some of the remaining fat over each of the muscles was debulked with a 3.7- or 4.6-mm cannula, while the surface overlying the creases over the midlamellar layer was smoothed |
| Monarca and Rizzo, 201526 | Outlining the pectoralis major muscle; if gynecomastia is present, the gland is removed; define the alba and the semilunar lines and pulling out the transverse tendinous intersections and muscular adherences; liposuction on the lines drawn over the deltoid, arm muscles, gluteal, and lower extremity muscles | Careful liposuction removes the adipose tissue, ensuring skin adhesion to the muscular plane; deep liposuction to remove the excess abdominal fat and to ensure tight skin above the muscles | Powerful liposuction is performed with basket/accelerator cannulas at the pectoral borders, and at the sternal notch to emphasize the medial insertions; aggressive cannula is used like a chisel in the subcutaneous tissue for the superficial liposuction | Residual adipose tissue homogenization by cannula avoids irregularity of the treated areas |
| Steinbrech and Sinno, 201628 | Selective lipocontouring (levels 1-6): 1 being sculpting alone to 6 being most extreme fat grafting; supine: abdominal wall and the linea alba, lateral vertical margin, serratus, obliques and inscription of the rectus abdominis; prone: flanks | Lipectomy by PAL or standard traditional suction lipectomy | NR | NR |
| Boeni, 202025 | Love handles, hypogastrium, the area over the serratus anterior, and the lower part over the pectoralis major; linea alba and S-shaped linea semilunaris; the transverse intersections were created with the bent cannula; arm definition: the groove between deltoid muscle and biceps was accessed; this sulcus continues on the back of the arm to a groove between the deltoid muscle and lateral head of triceps | All layer debulking was performed starting from deep to superficial to subdermal liposuction; reciprocating PAL (MicroAire Inc., Charlottesville, VA) with 1 straight 4-mm flared Mercedes cannula and 1 bent 4-mm flared Mercedes cannula | Reciprocating PAL (MicroAire); the fat between the tendinous intersections was retained or, when a thicker fat layer was present, reduced to a 1-cm fat layer from the dermis | Fat equalization step (vibration without suction) after HDL ensures smooth skin in the infraumbilical area |
| Husain et al, 201921 | Prone: flanks; supine: anterior flanks and abdomen | PAL of the deep layers of the abdomen and flanks is performed with a no. 5 Mercedes cannula. | PAL with a blunt-tip cannula (no. 4 or 5) to create the linea alba, semilunaris, and iliac crest lines with the cannula superficially next to the dermis; limit the cannula passes to a maximum of 10 (avoid thermal injury) | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Modified abdominal etching (MAE): linea alba is enhanced; etching along the edge of the linea semilunaris; deep liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | “Cross-tunneling” is done in all areas | Both superficial and deep liposuction is performed with a 4- and/or 5-mm basket cannula, and with PAL | NR |
| Full abdominal etching (FAE): linea alba is enhanced; etching along the edge of the linea semilunaris; aggressive deep and superficial liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | ||||
| Saad et al, 202023 | Deep fat compartments in the lower back; superficial fat compartments were treated to mark the lower back lines (caudal border of the latissimus dorsi muscle following along the lateral thoracolumbar fascia and the lateral vertical line of the erector spinae muscle caudally); the posterior upper arms were marked by suctioning the superficial fat between the deltoid and the triceps; deep medial and lateral abdominal compartments (below and above the umbilicus) and the deep fat compartment in the axilla; superficial fat compartments along the preoperatively marked lines on the abdomen and chest; abdominal inscriptions overlying the rectus abdominis | Separation: superficial and deep fat is separated through continuous passing of the cannula while no suctioning is performed; allows release from tethering structures such as blood vessels and fibrous septae | Aspiration: less aggressive cannulas to aspirate this low-resistance, separated fat; size depends on the region of treatment but, on average, ranges from 1 to 4 mm | Fat equalization: no suction; the exploded-tip cannula is used to smooth out irregular areas; equalization of the treated areas is accomplished by further emulsification of the remaining fat bed, evening out the inevitable thicker and thinner areas that exist |
| Niddam et al, 201922 | NS | When additional conventional contouring liposuction was needed, it was performed before the abdominal etching, with the same 4-mm cannula | The abdominal etching was carried out with a 4-mm 3-hole cannula along the drawings; the liposuction was performed mostly in the superficial planes but also in the deep plane, at full-power suction pressure | NR |
| Hoyos and Perez, 202037 | B (basic-definition liposculpture): vertical rectus abdominis, semilunaris line, obliques; posterior: erector spinae; arms: anterior posterior deltoid | Superficial subcutaneous fat was treated first in VASER mode, usually starting with a 3.7-mm 2-groove probe at an amplitude of 80%; if excessive resistance, energy was increased to 90%, or an alternative probe was selected; continuous mode was used to emulsify the deeper fat; 60-90 seconds of ultrasound delivery per 100 mL of tumescent fluid infiltrated | Completed liposuction with 4- and 3-mm cannulas connected to PowerX or MicroAire system; thorough liposuction is performed in the deep layer and after debulking, the 3-mm cannula is used to treat the superficial plane; controlled deformities are created by sculpting the underlying muscle anatomy, following the preoperative markings (lights, shadows, negative spaces, and dynamic zones) | Additional superficial lipoplasty is performed with small cannulas (3 mm) in order to define muscle groups and create shadows by removing almost all of the fat in the subdermal layer |
| M (moderate-definition liposculpture): whole rectus abdominis—transverse insertions, external obliques, pectoralis; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| X (extreme-definition liposculpture): whole rectus abdominis, transverse insertions, external obliques, pectoralis, serratus; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| Taha et al, 202024 | Lateral position: waist, iliac, lateral chest, and back regions: contralateral waist, iliac, lateral chest, and back regions; supine position for liposuction of the abdomen, chest, and thigh (if planned); prone position for completion of liposuction of the gluteal region, upper posterior thighs, and gluteal fat grafting, if needed | When VASER is used, 70%, pulsed mode was used and applied immediately following infiltration; fat emulsification until no resistance was encountered | Liposuction was performed with power-assisted techniques with the Lipomatic (Euromai) | NR |
| Saad et al, 202127 | Upper and lower back, including the gluteal region and the posterior arms; anterior arms, chest, medial and lateral abdomen | Dispersion: use of PAL’s vibratory energy without suction power; maximize the interaction between the tumescent fluid components and the fat tissue | Aspiration: liposuction was performed by PAL; superficial and deep fat harvesting was done with 5 mm (straight and bent) PAL HD cannulas (MicroAire Inc., Charlottesville, VA); superficial fat liposculpting consists of the detailed sculpting of the superficial fat layer to enhance the underlying musculoskeletal structures | Fat equalization: reciprocating movement of the PAL technology without suction; treat irregularities and correct any step-offs that could have been created during the aspiration phase |
| Author, year . | Anatomic concept (treated areas) . | Step 1 . | Step 2 . | Step 3 . |
|---|---|---|---|---|
| Mentz et al, 199312 | Anterior abdominal wall: linea alba and linea semi-lunaris; transverse intersections or inscriptions of the rectus muscle | 2- or 3-mm flat Becker-style liposuction cannula was used for superficial liposuction in the marked areas, first with the openings facing the skin, then with the openings facing the muscular surface | A groove was created to the desired depth; superficial liposuction was continued at the marked areas until there was apparent furrowing or deepening of the natural crease | Deep liposuction with a small Mercedes cannula (1.5-2.5 mm), leaving a thicker fat pad in the islands where muscular enhancement was necessary |
| Ersek and Salisbury, 19971 | Abdomen and flanks | Custom-designed 3-mm suction cannula is passed in the same channel many times to create a completely defatted groove; a new etched abdomen is obvious at the end of the procedure | NR | NR |
| Hoyos and Millard, 20079 | Areas with large fat deposits; back and posterior arms; inner thighs, waist, and neck; linea alba and its tendinous insertions, the pectoral inferior line, inguinal ligament | Emulsification: VASER: 1 minute/100 mL of infiltration, the clinical endpoint was the loss of resistance; large fat deposits were treated with a 3.7- or 2.9-mm 3-groove probe, 80% power (continuous mode); back and posterior arms were treated with a 3.7-mm 1-groove probe (continuous mode); skin or delicate areas, were treated with a 2.9-mm 3-groove probe, 60% power (pulsed mode). differential emulsification for each muscle group: superficial emulsification with a 2.9-mm 3-groove probe (pulse mode) | Debulking: areas of fat deposits in the deep layer, with 3.7- or 4.6-mm cannulas, and continued in the midlamellar layer and between muscle groups, avoiding aspiration against the delicate subdermal layer; superficial emulsification and extraction in the subdermal lamellar layer selectively over the muscular frame with a 2.9-mm probe for emulsification and a 3.0-mm cannula for aspiration | Transitioning: some of the remaining fat over each of the muscles was debulked with a 3.7- or 4.6-mm cannula, while the surface overlying the creases over the midlamellar layer was smoothed |
| Monarca and Rizzo, 201526 | Outlining the pectoralis major muscle; if gynecomastia is present, the gland is removed; define the alba and the semilunar lines and pulling out the transverse tendinous intersections and muscular adherences; liposuction on the lines drawn over the deltoid, arm muscles, gluteal, and lower extremity muscles | Careful liposuction removes the adipose tissue, ensuring skin adhesion to the muscular plane; deep liposuction to remove the excess abdominal fat and to ensure tight skin above the muscles | Powerful liposuction is performed with basket/accelerator cannulas at the pectoral borders, and at the sternal notch to emphasize the medial insertions; aggressive cannula is used like a chisel in the subcutaneous tissue for the superficial liposuction | Residual adipose tissue homogenization by cannula avoids irregularity of the treated areas |
| Steinbrech and Sinno, 201628 | Selective lipocontouring (levels 1-6): 1 being sculpting alone to 6 being most extreme fat grafting; supine: abdominal wall and the linea alba, lateral vertical margin, serratus, obliques and inscription of the rectus abdominis; prone: flanks | Lipectomy by PAL or standard traditional suction lipectomy | NR | NR |
| Boeni, 202025 | Love handles, hypogastrium, the area over the serratus anterior, and the lower part over the pectoralis major; linea alba and S-shaped linea semilunaris; the transverse intersections were created with the bent cannula; arm definition: the groove between deltoid muscle and biceps was accessed; this sulcus continues on the back of the arm to a groove between the deltoid muscle and lateral head of triceps | All layer debulking was performed starting from deep to superficial to subdermal liposuction; reciprocating PAL (MicroAire Inc., Charlottesville, VA) with 1 straight 4-mm flared Mercedes cannula and 1 bent 4-mm flared Mercedes cannula | Reciprocating PAL (MicroAire); the fat between the tendinous intersections was retained or, when a thicker fat layer was present, reduced to a 1-cm fat layer from the dermis | Fat equalization step (vibration without suction) after HDL ensures smooth skin in the infraumbilical area |
| Husain et al, 201921 | Prone: flanks; supine: anterior flanks and abdomen | PAL of the deep layers of the abdomen and flanks is performed with a no. 5 Mercedes cannula. | PAL with a blunt-tip cannula (no. 4 or 5) to create the linea alba, semilunaris, and iliac crest lines with the cannula superficially next to the dermis; limit the cannula passes to a maximum of 10 (avoid thermal injury) | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Modified abdominal etching (MAE): linea alba is enhanced; etching along the edge of the linea semilunaris; deep liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | “Cross-tunneling” is done in all areas | Both superficial and deep liposuction is performed with a 4- and/or 5-mm basket cannula, and with PAL | NR |
| Full abdominal etching (FAE): linea alba is enhanced; etching along the edge of the linea semilunaris; aggressive deep and superficial liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | ||||
| Saad et al, 202023 | Deep fat compartments in the lower back; superficial fat compartments were treated to mark the lower back lines (caudal border of the latissimus dorsi muscle following along the lateral thoracolumbar fascia and the lateral vertical line of the erector spinae muscle caudally); the posterior upper arms were marked by suctioning the superficial fat between the deltoid and the triceps; deep medial and lateral abdominal compartments (below and above the umbilicus) and the deep fat compartment in the axilla; superficial fat compartments along the preoperatively marked lines on the abdomen and chest; abdominal inscriptions overlying the rectus abdominis | Separation: superficial and deep fat is separated through continuous passing of the cannula while no suctioning is performed; allows release from tethering structures such as blood vessels and fibrous septae | Aspiration: less aggressive cannulas to aspirate this low-resistance, separated fat; size depends on the region of treatment but, on average, ranges from 1 to 4 mm | Fat equalization: no suction; the exploded-tip cannula is used to smooth out irregular areas; equalization of the treated areas is accomplished by further emulsification of the remaining fat bed, evening out the inevitable thicker and thinner areas that exist |
| Niddam et al, 201922 | NS | When additional conventional contouring liposuction was needed, it was performed before the abdominal etching, with the same 4-mm cannula | The abdominal etching was carried out with a 4-mm 3-hole cannula along the drawings; the liposuction was performed mostly in the superficial planes but also in the deep plane, at full-power suction pressure | NR |
| Hoyos and Perez, 202037 | B (basic-definition liposculpture): vertical rectus abdominis, semilunaris line, obliques; posterior: erector spinae; arms: anterior posterior deltoid | Superficial subcutaneous fat was treated first in VASER mode, usually starting with a 3.7-mm 2-groove probe at an amplitude of 80%; if excessive resistance, energy was increased to 90%, or an alternative probe was selected; continuous mode was used to emulsify the deeper fat; 60-90 seconds of ultrasound delivery per 100 mL of tumescent fluid infiltrated | Completed liposuction with 4- and 3-mm cannulas connected to PowerX or MicroAire system; thorough liposuction is performed in the deep layer and after debulking, the 3-mm cannula is used to treat the superficial plane; controlled deformities are created by sculpting the underlying muscle anatomy, following the preoperative markings (lights, shadows, negative spaces, and dynamic zones) | Additional superficial lipoplasty is performed with small cannulas (3 mm) in order to define muscle groups and create shadows by removing almost all of the fat in the subdermal layer |
| M (moderate-definition liposculpture): whole rectus abdominis—transverse insertions, external obliques, pectoralis; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| X (extreme-definition liposculpture): whole rectus abdominis, transverse insertions, external obliques, pectoralis, serratus; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| Taha et al, 202024 | Lateral position: waist, iliac, lateral chest, and back regions: contralateral waist, iliac, lateral chest, and back regions; supine position for liposuction of the abdomen, chest, and thigh (if planned); prone position for completion of liposuction of the gluteal region, upper posterior thighs, and gluteal fat grafting, if needed | When VASER is used, 70%, pulsed mode was used and applied immediately following infiltration; fat emulsification until no resistance was encountered | Liposuction was performed with power-assisted techniques with the Lipomatic (Euromai) | NR |
| Saad et al, 202127 | Upper and lower back, including the gluteal region and the posterior arms; anterior arms, chest, medial and lateral abdomen | Dispersion: use of PAL’s vibratory energy without suction power; maximize the interaction between the tumescent fluid components and the fat tissue | Aspiration: liposuction was performed by PAL; superficial and deep fat harvesting was done with 5 mm (straight and bent) PAL HD cannulas (MicroAire Inc., Charlottesville, VA); superficial fat liposculpting consists of the detailed sculpting of the superficial fat layer to enhance the underlying musculoskeletal structures | Fat equalization: reciprocating movement of the PAL technology without suction; treat irregularities and correct any step-offs that could have been created during the aspiration phase |
HD, high definition; NR, not reported; NS, not specified; PAL, power-assisted lipectomy; VASER, vibration amplification of sound energy at resonance.
| Author, year . | Anatomic concept (treated areas) . | Step 1 . | Step 2 . | Step 3 . |
|---|---|---|---|---|
| Mentz et al, 199312 | Anterior abdominal wall: linea alba and linea semi-lunaris; transverse intersections or inscriptions of the rectus muscle | 2- or 3-mm flat Becker-style liposuction cannula was used for superficial liposuction in the marked areas, first with the openings facing the skin, then with the openings facing the muscular surface | A groove was created to the desired depth; superficial liposuction was continued at the marked areas until there was apparent furrowing or deepening of the natural crease | Deep liposuction with a small Mercedes cannula (1.5-2.5 mm), leaving a thicker fat pad in the islands where muscular enhancement was necessary |
| Ersek and Salisbury, 19971 | Abdomen and flanks | Custom-designed 3-mm suction cannula is passed in the same channel many times to create a completely defatted groove; a new etched abdomen is obvious at the end of the procedure | NR | NR |
| Hoyos and Millard, 20079 | Areas with large fat deposits; back and posterior arms; inner thighs, waist, and neck; linea alba and its tendinous insertions, the pectoral inferior line, inguinal ligament | Emulsification: VASER: 1 minute/100 mL of infiltration, the clinical endpoint was the loss of resistance; large fat deposits were treated with a 3.7- or 2.9-mm 3-groove probe, 80% power (continuous mode); back and posterior arms were treated with a 3.7-mm 1-groove probe (continuous mode); skin or delicate areas, were treated with a 2.9-mm 3-groove probe, 60% power (pulsed mode). differential emulsification for each muscle group: superficial emulsification with a 2.9-mm 3-groove probe (pulse mode) | Debulking: areas of fat deposits in the deep layer, with 3.7- or 4.6-mm cannulas, and continued in the midlamellar layer and between muscle groups, avoiding aspiration against the delicate subdermal layer; superficial emulsification and extraction in the subdermal lamellar layer selectively over the muscular frame with a 2.9-mm probe for emulsification and a 3.0-mm cannula for aspiration | Transitioning: some of the remaining fat over each of the muscles was debulked with a 3.7- or 4.6-mm cannula, while the surface overlying the creases over the midlamellar layer was smoothed |
| Monarca and Rizzo, 201526 | Outlining the pectoralis major muscle; if gynecomastia is present, the gland is removed; define the alba and the semilunar lines and pulling out the transverse tendinous intersections and muscular adherences; liposuction on the lines drawn over the deltoid, arm muscles, gluteal, and lower extremity muscles | Careful liposuction removes the adipose tissue, ensuring skin adhesion to the muscular plane; deep liposuction to remove the excess abdominal fat and to ensure tight skin above the muscles | Powerful liposuction is performed with basket/accelerator cannulas at the pectoral borders, and at the sternal notch to emphasize the medial insertions; aggressive cannula is used like a chisel in the subcutaneous tissue for the superficial liposuction | Residual adipose tissue homogenization by cannula avoids irregularity of the treated areas |
| Steinbrech and Sinno, 201628 | Selective lipocontouring (levels 1-6): 1 being sculpting alone to 6 being most extreme fat grafting; supine: abdominal wall and the linea alba, lateral vertical margin, serratus, obliques and inscription of the rectus abdominis; prone: flanks | Lipectomy by PAL or standard traditional suction lipectomy | NR | NR |
| Boeni, 202025 | Love handles, hypogastrium, the area over the serratus anterior, and the lower part over the pectoralis major; linea alba and S-shaped linea semilunaris; the transverse intersections were created with the bent cannula; arm definition: the groove between deltoid muscle and biceps was accessed; this sulcus continues on the back of the arm to a groove between the deltoid muscle and lateral head of triceps | All layer debulking was performed starting from deep to superficial to subdermal liposuction; reciprocating PAL (MicroAire Inc., Charlottesville, VA) with 1 straight 4-mm flared Mercedes cannula and 1 bent 4-mm flared Mercedes cannula | Reciprocating PAL (MicroAire); the fat between the tendinous intersections was retained or, when a thicker fat layer was present, reduced to a 1-cm fat layer from the dermis | Fat equalization step (vibration without suction) after HDL ensures smooth skin in the infraumbilical area |
| Husain et al, 201921 | Prone: flanks; supine: anterior flanks and abdomen | PAL of the deep layers of the abdomen and flanks is performed with a no. 5 Mercedes cannula. | PAL with a blunt-tip cannula (no. 4 or 5) to create the linea alba, semilunaris, and iliac crest lines with the cannula superficially next to the dermis; limit the cannula passes to a maximum of 10 (avoid thermal injury) | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Modified abdominal etching (MAE): linea alba is enhanced; etching along the edge of the linea semilunaris; deep liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | “Cross-tunneling” is done in all areas | Both superficial and deep liposuction is performed with a 4- and/or 5-mm basket cannula, and with PAL | NR |
| Full abdominal etching (FAE): linea alba is enhanced; etching along the edge of the linea semilunaris; aggressive deep and superficial liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | ||||
| Saad et al, 202023 | Deep fat compartments in the lower back; superficial fat compartments were treated to mark the lower back lines (caudal border of the latissimus dorsi muscle following along the lateral thoracolumbar fascia and the lateral vertical line of the erector spinae muscle caudally); the posterior upper arms were marked by suctioning the superficial fat between the deltoid and the triceps; deep medial and lateral abdominal compartments (below and above the umbilicus) and the deep fat compartment in the axilla; superficial fat compartments along the preoperatively marked lines on the abdomen and chest; abdominal inscriptions overlying the rectus abdominis | Separation: superficial and deep fat is separated through continuous passing of the cannula while no suctioning is performed; allows release from tethering structures such as blood vessels and fibrous septae | Aspiration: less aggressive cannulas to aspirate this low-resistance, separated fat; size depends on the region of treatment but, on average, ranges from 1 to 4 mm | Fat equalization: no suction; the exploded-tip cannula is used to smooth out irregular areas; equalization of the treated areas is accomplished by further emulsification of the remaining fat bed, evening out the inevitable thicker and thinner areas that exist |
| Niddam et al, 201922 | NS | When additional conventional contouring liposuction was needed, it was performed before the abdominal etching, with the same 4-mm cannula | The abdominal etching was carried out with a 4-mm 3-hole cannula along the drawings; the liposuction was performed mostly in the superficial planes but also in the deep plane, at full-power suction pressure | NR |
| Hoyos and Perez, 202037 | B (basic-definition liposculpture): vertical rectus abdominis, semilunaris line, obliques; posterior: erector spinae; arms: anterior posterior deltoid | Superficial subcutaneous fat was treated first in VASER mode, usually starting with a 3.7-mm 2-groove probe at an amplitude of 80%; if excessive resistance, energy was increased to 90%, or an alternative probe was selected; continuous mode was used to emulsify the deeper fat; 60-90 seconds of ultrasound delivery per 100 mL of tumescent fluid infiltrated | Completed liposuction with 4- and 3-mm cannulas connected to PowerX or MicroAire system; thorough liposuction is performed in the deep layer and after debulking, the 3-mm cannula is used to treat the superficial plane; controlled deformities are created by sculpting the underlying muscle anatomy, following the preoperative markings (lights, shadows, negative spaces, and dynamic zones) | Additional superficial lipoplasty is performed with small cannulas (3 mm) in order to define muscle groups and create shadows by removing almost all of the fat in the subdermal layer |
| M (moderate-definition liposculpture): whole rectus abdominis—transverse insertions, external obliques, pectoralis; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| X (extreme-definition liposculpture): whole rectus abdominis, transverse insertions, external obliques, pectoralis, serratus; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| Taha et al, 202024 | Lateral position: waist, iliac, lateral chest, and back regions: contralateral waist, iliac, lateral chest, and back regions; supine position for liposuction of the abdomen, chest, and thigh (if planned); prone position for completion of liposuction of the gluteal region, upper posterior thighs, and gluteal fat grafting, if needed | When VASER is used, 70%, pulsed mode was used and applied immediately following infiltration; fat emulsification until no resistance was encountered | Liposuction was performed with power-assisted techniques with the Lipomatic (Euromai) | NR |
| Saad et al, 202127 | Upper and lower back, including the gluteal region and the posterior arms; anterior arms, chest, medial and lateral abdomen | Dispersion: use of PAL’s vibratory energy without suction power; maximize the interaction between the tumescent fluid components and the fat tissue | Aspiration: liposuction was performed by PAL; superficial and deep fat harvesting was done with 5 mm (straight and bent) PAL HD cannulas (MicroAire Inc., Charlottesville, VA); superficial fat liposculpting consists of the detailed sculpting of the superficial fat layer to enhance the underlying musculoskeletal structures | Fat equalization: reciprocating movement of the PAL technology without suction; treat irregularities and correct any step-offs that could have been created during the aspiration phase |
| Author, year . | Anatomic concept (treated areas) . | Step 1 . | Step 2 . | Step 3 . |
|---|---|---|---|---|
| Mentz et al, 199312 | Anterior abdominal wall: linea alba and linea semi-lunaris; transverse intersections or inscriptions of the rectus muscle | 2- or 3-mm flat Becker-style liposuction cannula was used for superficial liposuction in the marked areas, first with the openings facing the skin, then with the openings facing the muscular surface | A groove was created to the desired depth; superficial liposuction was continued at the marked areas until there was apparent furrowing or deepening of the natural crease | Deep liposuction with a small Mercedes cannula (1.5-2.5 mm), leaving a thicker fat pad in the islands where muscular enhancement was necessary |
| Ersek and Salisbury, 19971 | Abdomen and flanks | Custom-designed 3-mm suction cannula is passed in the same channel many times to create a completely defatted groove; a new etched abdomen is obvious at the end of the procedure | NR | NR |
| Hoyos and Millard, 20079 | Areas with large fat deposits; back and posterior arms; inner thighs, waist, and neck; linea alba and its tendinous insertions, the pectoral inferior line, inguinal ligament | Emulsification: VASER: 1 minute/100 mL of infiltration, the clinical endpoint was the loss of resistance; large fat deposits were treated with a 3.7- or 2.9-mm 3-groove probe, 80% power (continuous mode); back and posterior arms were treated with a 3.7-mm 1-groove probe (continuous mode); skin or delicate areas, were treated with a 2.9-mm 3-groove probe, 60% power (pulsed mode). differential emulsification for each muscle group: superficial emulsification with a 2.9-mm 3-groove probe (pulse mode) | Debulking: areas of fat deposits in the deep layer, with 3.7- or 4.6-mm cannulas, and continued in the midlamellar layer and between muscle groups, avoiding aspiration against the delicate subdermal layer; superficial emulsification and extraction in the subdermal lamellar layer selectively over the muscular frame with a 2.9-mm probe for emulsification and a 3.0-mm cannula for aspiration | Transitioning: some of the remaining fat over each of the muscles was debulked with a 3.7- or 4.6-mm cannula, while the surface overlying the creases over the midlamellar layer was smoothed |
| Monarca and Rizzo, 201526 | Outlining the pectoralis major muscle; if gynecomastia is present, the gland is removed; define the alba and the semilunar lines and pulling out the transverse tendinous intersections and muscular adherences; liposuction on the lines drawn over the deltoid, arm muscles, gluteal, and lower extremity muscles | Careful liposuction removes the adipose tissue, ensuring skin adhesion to the muscular plane; deep liposuction to remove the excess abdominal fat and to ensure tight skin above the muscles | Powerful liposuction is performed with basket/accelerator cannulas at the pectoral borders, and at the sternal notch to emphasize the medial insertions; aggressive cannula is used like a chisel in the subcutaneous tissue for the superficial liposuction | Residual adipose tissue homogenization by cannula avoids irregularity of the treated areas |
| Steinbrech and Sinno, 201628 | Selective lipocontouring (levels 1-6): 1 being sculpting alone to 6 being most extreme fat grafting; supine: abdominal wall and the linea alba, lateral vertical margin, serratus, obliques and inscription of the rectus abdominis; prone: flanks | Lipectomy by PAL or standard traditional suction lipectomy | NR | NR |
| Boeni, 202025 | Love handles, hypogastrium, the area over the serratus anterior, and the lower part over the pectoralis major; linea alba and S-shaped linea semilunaris; the transverse intersections were created with the bent cannula; arm definition: the groove between deltoid muscle and biceps was accessed; this sulcus continues on the back of the arm to a groove between the deltoid muscle and lateral head of triceps | All layer debulking was performed starting from deep to superficial to subdermal liposuction; reciprocating PAL (MicroAire Inc., Charlottesville, VA) with 1 straight 4-mm flared Mercedes cannula and 1 bent 4-mm flared Mercedes cannula | Reciprocating PAL (MicroAire); the fat between the tendinous intersections was retained or, when a thicker fat layer was present, reduced to a 1-cm fat layer from the dermis | Fat equalization step (vibration without suction) after HDL ensures smooth skin in the infraumbilical area |
| Husain et al, 201921 | Prone: flanks; supine: anterior flanks and abdomen | PAL of the deep layers of the abdomen and flanks is performed with a no. 5 Mercedes cannula. | PAL with a blunt-tip cannula (no. 4 or 5) to create the linea alba, semilunaris, and iliac crest lines with the cannula superficially next to the dermis; limit the cannula passes to a maximum of 10 (avoid thermal injury) | NR |
| Agochukwu-Nwubah and Mentz, 201920 | Modified abdominal etching (MAE): linea alba is enhanced; etching along the edge of the linea semilunaris; deep liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | “Cross-tunneling” is done in all areas | Both superficial and deep liposuction is performed with a 4- and/or 5-mm basket cannula, and with PAL | NR |
| Full abdominal etching (FAE): linea alba is enhanced; etching along the edge of the linea semilunaris; aggressive deep and superficial liposuction is performed along the linea semilunaris and along the transverse rectus inscriptions; etch 2-3 cm surrounding the umbilicus; deep and superficial liposuction is performed lateral to the rectus muscle | ||||
| Saad et al, 202023 | Deep fat compartments in the lower back; superficial fat compartments were treated to mark the lower back lines (caudal border of the latissimus dorsi muscle following along the lateral thoracolumbar fascia and the lateral vertical line of the erector spinae muscle caudally); the posterior upper arms were marked by suctioning the superficial fat between the deltoid and the triceps; deep medial and lateral abdominal compartments (below and above the umbilicus) and the deep fat compartment in the axilla; superficial fat compartments along the preoperatively marked lines on the abdomen and chest; abdominal inscriptions overlying the rectus abdominis | Separation: superficial and deep fat is separated through continuous passing of the cannula while no suctioning is performed; allows release from tethering structures such as blood vessels and fibrous septae | Aspiration: less aggressive cannulas to aspirate this low-resistance, separated fat; size depends on the region of treatment but, on average, ranges from 1 to 4 mm | Fat equalization: no suction; the exploded-tip cannula is used to smooth out irregular areas; equalization of the treated areas is accomplished by further emulsification of the remaining fat bed, evening out the inevitable thicker and thinner areas that exist |
| Niddam et al, 201922 | NS | When additional conventional contouring liposuction was needed, it was performed before the abdominal etching, with the same 4-mm cannula | The abdominal etching was carried out with a 4-mm 3-hole cannula along the drawings; the liposuction was performed mostly in the superficial planes but also in the deep plane, at full-power suction pressure | NR |
| Hoyos and Perez, 202037 | B (basic-definition liposculpture): vertical rectus abdominis, semilunaris line, obliques; posterior: erector spinae; arms: anterior posterior deltoid | Superficial subcutaneous fat was treated first in VASER mode, usually starting with a 3.7-mm 2-groove probe at an amplitude of 80%; if excessive resistance, energy was increased to 90%, or an alternative probe was selected; continuous mode was used to emulsify the deeper fat; 60-90 seconds of ultrasound delivery per 100 mL of tumescent fluid infiltrated | Completed liposuction with 4- and 3-mm cannulas connected to PowerX or MicroAire system; thorough liposuction is performed in the deep layer and after debulking, the 3-mm cannula is used to treat the superficial plane; controlled deformities are created by sculpting the underlying muscle anatomy, following the preoperative markings (lights, shadows, negative spaces, and dynamic zones) | Additional superficial lipoplasty is performed with small cannulas (3 mm) in order to define muscle groups and create shadows by removing almost all of the fat in the subdermal layer |
| M (moderate-definition liposculpture): whole rectus abdominis—transverse insertions, external obliques, pectoralis; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| X (extreme-definition liposculpture): whole rectus abdominis, transverse insertions, external obliques, pectoralis, serratus; posterior: erector spinae, upper and lower trapezius; arms: anterior posterior deltoid, biceps triceps | ||||
| Taha et al, 202024 | Lateral position: waist, iliac, lateral chest, and back regions: contralateral waist, iliac, lateral chest, and back regions; supine position for liposuction of the abdomen, chest, and thigh (if planned); prone position for completion of liposuction of the gluteal region, upper posterior thighs, and gluteal fat grafting, if needed | When VASER is used, 70%, pulsed mode was used and applied immediately following infiltration; fat emulsification until no resistance was encountered | Liposuction was performed with power-assisted techniques with the Lipomatic (Euromai) | NR |
| Saad et al, 202127 | Upper and lower back, including the gluteal region and the posterior arms; anterior arms, chest, medial and lateral abdomen | Dispersion: use of PAL’s vibratory energy without suction power; maximize the interaction between the tumescent fluid components and the fat tissue | Aspiration: liposuction was performed by PAL; superficial and deep fat harvesting was done with 5 mm (straight and bent) PAL HD cannulas (MicroAire Inc., Charlottesville, VA); superficial fat liposculpting consists of the detailed sculpting of the superficial fat layer to enhance the underlying musculoskeletal structures | Fat equalization: reciprocating movement of the PAL technology without suction; treat irregularities and correct any step-offs that could have been created during the aspiration phase |
HD, high definition; NR, not reported; NS, not specified; PAL, power-assisted lipectomy; VASER, vibration amplification of sound energy at resonance.
As described by Hoyos et al, once emulsification was finished, debulking was accomplished in the deep fat layer with 3.7- or 4.6-mm cannulas and then the superficial plane was treated with a 3.0-mm cannula (Sound Surgical Technologies, Louisville, CO).9,10 Controlled irregularities were crafted over the preoperative markings to sculpt the muscle anatomy. HDL was accomplished by means of small cannulas, removing almost all of the fat in the subdermal layer to define muscle groups.10 Finally, Hoyos and Millard also reported a transitioning phase accomplished by debulking some of the remaining fat over muscles, while smoothing the surface overlying the creases at the mid-lamellar layer with 3.7- or 4.6-mm cannulas (Table 4).9
Power-Assisted Liposculpture
Boeni performed all-layer reciprocating power-assisted liposuction (PAL) (MicroAire Surgical Instruments, Charlottesville, VA) with straight and bent 4-mm flared Mercedes cannulas, starting from deep to superficial, to subdermal liposuction.25 Agochukwu-Nwubah and Mentz initially performed “cross-tunneling” over all areas, and then performed both superficial and deep PAL with 4- and/or 5-mm basket cannulas (MicroAire).20 Husain et al performed PAL of the deep fat layer over the abdomen and flanks with a Mercedes cannula no. 5 (MicroAire); and then, with a blunt-tip cannula, superficially sculpted the linea alba, semilunaris, and iliac crest lines, placing the cannula superficially next to the dermis and limiting the cannula passes to a maximum of 10.21 Steinbrech and Sinno also reported the use of PAL or standard traditional SAL.28
Saad et al initially used the vibratory energy of PAL (MicroAire) without suction power to maximize the interaction between the tumescent fluid components and the fat tissue by continuously passing the cannula while no suctioning was performed. Then, superficial and deep fat harvesting was done with 5-mm (straight and bent) PAL HD cannulas (MicroAire). Superficial fat liposculpting consisted of a detailed liposuction over the superficial fat layer to enhance the underlying musculoskeletal structures.23,27 Fat equalization (vibration without suction) was reported by Saad et al and Boeni after HDL to ensure smooth blending of the skin in the infraumbilical areas (Table 4).23,25,27
Conventional Liposuction
Mentz et al commenced with superficial liposuction in the marked areas with a 2- or 3-mm flat Becker-style cannula until the desired groove was created.12 Deep liposuction with a small MicroAire Mercedes cannula (1.5-2.5 mm) was then performed, leaving a thicker fat pad in the islands where muscular enhancement was required.12
Niddam et al used conventional contouring liposuction before abdominal etching when needed with a 4-mm cannula. Abdominal etching was subsequently carried out with a 4-mm 3-hole cannula along the drawings, mostly in the superficial planes but also in the deep plane.22 Monarca and Rizzo reported a similar technique to that of Niddam et al. However, they added a final step with residual adipose tissue homogenization by cannula which avoided irregularities over the treated areas (Table 4).26
Fat Grafting
Nine articles reported the use of fat grafting as an adjunct to liposuction to improve outcomes of aesthetic lipoplasty.9,10,21,23,25-28 Monarca and Rizzo described fat grafting in the lower and upper extremities where greater projection was required to achieve a more athletic appearance.26 Steinbrech and Sinno reported selective fat grafting to the rectus muscle and serratus anterior in an attempt to enhance the muscular contour.28 Husain et al delivered fat to the deltoids and biceps.21 Hoyos et al described a multilayered fat-grafting technique in which small amounts of fat were delivered into the subcutaneous and intramuscular planes as the cannula moved in retrograde manner over the deltoids and pectoralis.10 In comparison to Hoyos et al, Saad et al performed fat grafting solely in the subcutaneous pectoral area, similar to Boeni.27 In the gluteal area fat was solely grafted in the subcutaneous layer (Table 5).10
Fat Grafting Technique and Use of Technical Considerations on the Use of Drains
| Author, year . | Fat grafting . | Drains . |
|---|---|---|
| Mentz et al, 199312 | NR | The puncture sites were closed with a single 5-0 nylon suture |
| Ersek and Salisbury, 19971 | NR | Escutcheon incisions closed with 5-0 absorbable buried stitches; abdominal incisions are closed with suture strips |
| Hoyos et al, 20079 | Fat grafting in the pectoral area | Open drains (small Jackson-Pratt–type drain cut short, without suction) were left for 48 to 72 hours in the inguinal area |
| Monarca and Rizzo, 201526 | Lipofilling for superficial muscle bulk of the upper and the lower extremities | NR |
| Steinbrech and Sinno, 201628 | The fat is transplanted with a 1.2 Tulip fat grafting cannula (Tulip Medical Products, San Diego, CA); fat grafting to the rectus muscle and serratus anterior | Liposuction sites are closed with 5-0 black nylon; lower pelvic incisions remain open for drainage |
| Boeni, 202025 | Fat grafting to the upper pole of the pectoralis muscle | Incisions were left open |
| Husain et al, 201921 | Fat grafting over deltoids and biceps | Incisions are left open to drain; Jackson-Pratt drains were used in a few patients |
| Agochukwu-Nwubah and Mentz, 201920 | No fat grafting | The liposuction access ports are left open to drain |
| Saad et al, 202023 | Fat processing with a Lipofilter system (MicroAire Inc., Charlottesville, VA); microdroplet grafting was performed in the subcutaneous pectoral area; fat grafting/chest side 85 mL (range, 65-120 mL) | None of the patients had drains placed in the surgical bed |
| Niddam et al, 201922 | No fat grafting | NR |
| Hoyos and Perez, 202037 | Gluteus maximus and medius, pectorals, deltoids, calves (if needed); arms: biceps and triceps; fat is delivered in the pectoralis and deltoids in the subcutaneous, submuscular, and intramuscular planes with multiple fine strokes to ensure small parcels are left; the gluteal area was only grafted in the subcutaneous layer, following the EVL technique within a closed system | Some incisions were left open for lymphatic drainage in slope points and Blake drains (Ethicon Inc., Johnson & Johnson) were placed in the subcutaneous space; the remaining incisions were sutured with inverted deep dermal sutures |
| Taha et al, 202024 | NS | A silicone drain was placed in the inguinal region, one on each side, and in the iliac region as well; incision sites were left open |
| Saad et al, 202127 | Fat is collected and processed with the Lipofilter System (MicroAire Inc., Charlottesville, VA) in case fat is needed for transfer; fat transfer to the chest was performed whenever indicated | No drains were used; wounds were closed with absorbable sutures |
| Author, year . | Fat grafting . | Drains . |
|---|---|---|
| Mentz et al, 199312 | NR | The puncture sites were closed with a single 5-0 nylon suture |
| Ersek and Salisbury, 19971 | NR | Escutcheon incisions closed with 5-0 absorbable buried stitches; abdominal incisions are closed with suture strips |
| Hoyos et al, 20079 | Fat grafting in the pectoral area | Open drains (small Jackson-Pratt–type drain cut short, without suction) were left for 48 to 72 hours in the inguinal area |
| Monarca and Rizzo, 201526 | Lipofilling for superficial muscle bulk of the upper and the lower extremities | NR |
| Steinbrech and Sinno, 201628 | The fat is transplanted with a 1.2 Tulip fat grafting cannula (Tulip Medical Products, San Diego, CA); fat grafting to the rectus muscle and serratus anterior | Liposuction sites are closed with 5-0 black nylon; lower pelvic incisions remain open for drainage |
| Boeni, 202025 | Fat grafting to the upper pole of the pectoralis muscle | Incisions were left open |
| Husain et al, 201921 | Fat grafting over deltoids and biceps | Incisions are left open to drain; Jackson-Pratt drains were used in a few patients |
| Agochukwu-Nwubah and Mentz, 201920 | No fat grafting | The liposuction access ports are left open to drain |
| Saad et al, 202023 | Fat processing with a Lipofilter system (MicroAire Inc., Charlottesville, VA); microdroplet grafting was performed in the subcutaneous pectoral area; fat grafting/chest side 85 mL (range, 65-120 mL) | None of the patients had drains placed in the surgical bed |
| Niddam et al, 201922 | No fat grafting | NR |
| Hoyos and Perez, 202037 | Gluteus maximus and medius, pectorals, deltoids, calves (if needed); arms: biceps and triceps; fat is delivered in the pectoralis and deltoids in the subcutaneous, submuscular, and intramuscular planes with multiple fine strokes to ensure small parcels are left; the gluteal area was only grafted in the subcutaneous layer, following the EVL technique within a closed system | Some incisions were left open for lymphatic drainage in slope points and Blake drains (Ethicon Inc., Johnson & Johnson) were placed in the subcutaneous space; the remaining incisions were sutured with inverted deep dermal sutures |
| Taha et al, 202024 | NS | A silicone drain was placed in the inguinal region, one on each side, and in the iliac region as well; incision sites were left open |
| Saad et al, 202127 | Fat is collected and processed with the Lipofilter System (MicroAire Inc., Charlottesville, VA) in case fat is needed for transfer; fat transfer to the chest was performed whenever indicated | No drains were used; wounds were closed with absorbable sutures |
EVL, expansion vibration lipofilling; NS, not specified; NR, not reported.
Fat Grafting Technique and Use of Technical Considerations on the Use of Drains
| Author, year . | Fat grafting . | Drains . |
|---|---|---|
| Mentz et al, 199312 | NR | The puncture sites were closed with a single 5-0 nylon suture |
| Ersek and Salisbury, 19971 | NR | Escutcheon incisions closed with 5-0 absorbable buried stitches; abdominal incisions are closed with suture strips |
| Hoyos et al, 20079 | Fat grafting in the pectoral area | Open drains (small Jackson-Pratt–type drain cut short, without suction) were left for 48 to 72 hours in the inguinal area |
| Monarca and Rizzo, 201526 | Lipofilling for superficial muscle bulk of the upper and the lower extremities | NR |
| Steinbrech and Sinno, 201628 | The fat is transplanted with a 1.2 Tulip fat grafting cannula (Tulip Medical Products, San Diego, CA); fat grafting to the rectus muscle and serratus anterior | Liposuction sites are closed with 5-0 black nylon; lower pelvic incisions remain open for drainage |
| Boeni, 202025 | Fat grafting to the upper pole of the pectoralis muscle | Incisions were left open |
| Husain et al, 201921 | Fat grafting over deltoids and biceps | Incisions are left open to drain; Jackson-Pratt drains were used in a few patients |
| Agochukwu-Nwubah and Mentz, 201920 | No fat grafting | The liposuction access ports are left open to drain |
| Saad et al, 202023 | Fat processing with a Lipofilter system (MicroAire Inc., Charlottesville, VA); microdroplet grafting was performed in the subcutaneous pectoral area; fat grafting/chest side 85 mL (range, 65-120 mL) | None of the patients had drains placed in the surgical bed |
| Niddam et al, 201922 | No fat grafting | NR |
| Hoyos and Perez, 202037 | Gluteus maximus and medius, pectorals, deltoids, calves (if needed); arms: biceps and triceps; fat is delivered in the pectoralis and deltoids in the subcutaneous, submuscular, and intramuscular planes with multiple fine strokes to ensure small parcels are left; the gluteal area was only grafted in the subcutaneous layer, following the EVL technique within a closed system | Some incisions were left open for lymphatic drainage in slope points and Blake drains (Ethicon Inc., Johnson & Johnson) were placed in the subcutaneous space; the remaining incisions were sutured with inverted deep dermal sutures |
| Taha et al, 202024 | NS | A silicone drain was placed in the inguinal region, one on each side, and in the iliac region as well; incision sites were left open |
| Saad et al, 202127 | Fat is collected and processed with the Lipofilter System (MicroAire Inc., Charlottesville, VA) in case fat is needed for transfer; fat transfer to the chest was performed whenever indicated | No drains were used; wounds were closed with absorbable sutures |
| Author, year . | Fat grafting . | Drains . |
|---|---|---|
| Mentz et al, 199312 | NR | The puncture sites were closed with a single 5-0 nylon suture |
| Ersek and Salisbury, 19971 | NR | Escutcheon incisions closed with 5-0 absorbable buried stitches; abdominal incisions are closed with suture strips |
| Hoyos et al, 20079 | Fat grafting in the pectoral area | Open drains (small Jackson-Pratt–type drain cut short, without suction) were left for 48 to 72 hours in the inguinal area |
| Monarca and Rizzo, 201526 | Lipofilling for superficial muscle bulk of the upper and the lower extremities | NR |
| Steinbrech and Sinno, 201628 | The fat is transplanted with a 1.2 Tulip fat grafting cannula (Tulip Medical Products, San Diego, CA); fat grafting to the rectus muscle and serratus anterior | Liposuction sites are closed with 5-0 black nylon; lower pelvic incisions remain open for drainage |
| Boeni, 202025 | Fat grafting to the upper pole of the pectoralis muscle | Incisions were left open |
| Husain et al, 201921 | Fat grafting over deltoids and biceps | Incisions are left open to drain; Jackson-Pratt drains were used in a few patients |
| Agochukwu-Nwubah and Mentz, 201920 | No fat grafting | The liposuction access ports are left open to drain |
| Saad et al, 202023 | Fat processing with a Lipofilter system (MicroAire Inc., Charlottesville, VA); microdroplet grafting was performed in the subcutaneous pectoral area; fat grafting/chest side 85 mL (range, 65-120 mL) | None of the patients had drains placed in the surgical bed |
| Niddam et al, 201922 | No fat grafting | NR |
| Hoyos and Perez, 202037 | Gluteus maximus and medius, pectorals, deltoids, calves (if needed); arms: biceps and triceps; fat is delivered in the pectoralis and deltoids in the subcutaneous, submuscular, and intramuscular planes with multiple fine strokes to ensure small parcels are left; the gluteal area was only grafted in the subcutaneous layer, following the EVL technique within a closed system | Some incisions were left open for lymphatic drainage in slope points and Blake drains (Ethicon Inc., Johnson & Johnson) were placed in the subcutaneous space; the remaining incisions were sutured with inverted deep dermal sutures |
| Taha et al, 202024 | NS | A silicone drain was placed in the inguinal region, one on each side, and in the iliac region as well; incision sites were left open |
| Saad et al, 202127 | Fat is collected and processed with the Lipofilter System (MicroAire Inc., Charlottesville, VA) in case fat is needed for transfer; fat transfer to the chest was performed whenever indicated | No drains were used; wounds were closed with absorbable sutures |
EVL, expansion vibration lipofilling; NS, not specified; NR, not reported.
Wound Closure and Drains
Ersek and Salisbury, Mentz et al, and Saad et al and closed the puncture sites with 5-0 nonabsorbable or absorbable sutures.1,12,27 Hoyos et al reported the use of open drains in the inguinal area, and also stated that some puncture sites were left open for lymphatic drainage in slope points. The rest were closed with inverted deep dermal sutures.10 Taha et al inserted drains in the inguinal region and left some incisions open to drain.24 In 4 studies incisions were left open without additional drains (Table 5).20,21,25,28
Postoperative Protocol
The majority of studies used abdominal compression garments for 2 to 6 weeks and adhesive foam strips over the superficially sculpted regions for 2 to 7 days. Niddam et al reported the use of 4-mm custom plastic rods positioned along the superficial liposculpted areas for 10 days.22 Postoperative lymphatic drainage and massage therapy started during the first postoperative week was reported in 5 studies.9,24,25,27,29 Exercise was allowed on postoperative days 5 or 14; 12,20 however, heavy exercise was delayed until 4 weeks postoperatively.21 Boeni reported the administration of vitamin C (1000 mg) per os to limit methemoglobinemia caused by local anesthetics (Table 6).25
Immediate Postoperative Dressings and Postoperative Wound Protocol of Included Studies
| Author, year . | Immediate postoperative dressings . | Postoperative wound protocol . |
|---|---|---|
| Mentz et al, 199312 | Abdominal garment | Patient was placed in an abdominal garment; sutures were removed on POD 7, and exercise was allowed on POD 14 |
| Ersek and Salisbury, 19971 | Constricting corset with 0.5-inch rubber foam pad placed over the etched area | The patient is then placed in a constricting corset with 0.5-inch rubber foam pad placed over the etched area to prevent any unexpected folds |
| Hoyos et al, 20079 | Mild-compression garment; deep-vein thrombosis stockings; cotton-laminated soft foam band (4 weeks) | Oral antibiotic and anti-inflammatory drugs; after 48 hours, postoperative lymphatic drainage massages and adjunctive external ultrasound (once a day/10 days) |
| Monarca and Rizzo, 201526 | Elastocompressive dressing | Antithrombotic prophylaxis (1 week); elastocompressive dressing (10-15 days) |
| Steinbrech and Sinno, 201628 | Strips of Reston foam (3M, St Paul, MN) over the areas contoured (3-5 days); abdominal binder | Sponge bathes are acceptable until first postoperative visit; baths and swimming are not allowed for 3 weeks |
| Boeni, 202025 | Foam pads (Epifoam, Biodermis, Henderson, NV) to enhance definition lines (3 days); compression garments | Vitamin C (1000 mg) was given orally; compression garments (3 weeks); lymphatic drainage after 48 hours; endermology starting 1 month after surgery |
| Husain et al, 201921 | Compression over the etched areas with TopiFoam (Mentor-Aesthetics, Irvine, CA); abdominal binder | Binder with TopiFoam (2-3 days); compression garment (worn permanently for 2 weeks, part time for 2 weeks); heavy exercise (which involves core and/or trunk) delayed until 4 weeks postoperatively |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal pads, or 4x4 adhesive foam (Reston), and a binder | Foam dressing (1 week); compressive binder (2-6 weeks); exercise is allowed 5 days after surgery |
| Saad et al, 202023 | Compression foam (Epifoam) strips were applied over the superficially marked areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Lymphatic massage: 2 sessions the first postoperative week; manual lymphatic massage: includes draining areas of swelling to the closest anatomic lymph node pool, as well as drainage of superficial fat areas that were treated |
| Niddam et al, 201922 | Cut-to-size plastic rods of 4 mm diameter were positioned along the liposuction muscle mass (10 days); these rods were held between 2 strips of adhesive tape to prevent skin damage | Conventional compression girdle for 21 extra days |
| Hoyos and Perez, 202037 | Garments and foam | Mild compression anti-DVT stockings (7 days) |
| Taha et al, 202024 | All patients were padded with cotton dressings and placed in a pressure garment | Daily dressing with fusidic acid around the drains; drains were removed after first postoperative week; antibiotics were prescribed if fat injection (1 week); pressure garment worn for 6 weeks—for most of the day in the first 3 weeks and during the day for the next 3 weeks; massage sessions: within POD 5 (every other day in the first week, twice per week in the second week, and then once per week) |
| Saad et al, 202127 | EpiFoam (Biodermis Inc., Henderson, NV) strips over the superficially sculpted regions in both anterior and posterior areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Admitted to the hospital for overnight observation and discharged on POD 1; lymphatic draining massage: 2 sessions starting the second postoperative week, followed by additional sessions as needed; compression garments for 3 weeks |
| Author, year . | Immediate postoperative dressings . | Postoperative wound protocol . |
|---|---|---|
| Mentz et al, 199312 | Abdominal garment | Patient was placed in an abdominal garment; sutures were removed on POD 7, and exercise was allowed on POD 14 |
| Ersek and Salisbury, 19971 | Constricting corset with 0.5-inch rubber foam pad placed over the etched area | The patient is then placed in a constricting corset with 0.5-inch rubber foam pad placed over the etched area to prevent any unexpected folds |
| Hoyos et al, 20079 | Mild-compression garment; deep-vein thrombosis stockings; cotton-laminated soft foam band (4 weeks) | Oral antibiotic and anti-inflammatory drugs; after 48 hours, postoperative lymphatic drainage massages and adjunctive external ultrasound (once a day/10 days) |
| Monarca and Rizzo, 201526 | Elastocompressive dressing | Antithrombotic prophylaxis (1 week); elastocompressive dressing (10-15 days) |
| Steinbrech and Sinno, 201628 | Strips of Reston foam (3M, St Paul, MN) over the areas contoured (3-5 days); abdominal binder | Sponge bathes are acceptable until first postoperative visit; baths and swimming are not allowed for 3 weeks |
| Boeni, 202025 | Foam pads (Epifoam, Biodermis, Henderson, NV) to enhance definition lines (3 days); compression garments | Vitamin C (1000 mg) was given orally; compression garments (3 weeks); lymphatic drainage after 48 hours; endermology starting 1 month after surgery |
| Husain et al, 201921 | Compression over the etched areas with TopiFoam (Mentor-Aesthetics, Irvine, CA); abdominal binder | Binder with TopiFoam (2-3 days); compression garment (worn permanently for 2 weeks, part time for 2 weeks); heavy exercise (which involves core and/or trunk) delayed until 4 weeks postoperatively |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal pads, or 4x4 adhesive foam (Reston), and a binder | Foam dressing (1 week); compressive binder (2-6 weeks); exercise is allowed 5 days after surgery |
| Saad et al, 202023 | Compression foam (Epifoam) strips were applied over the superficially marked areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Lymphatic massage: 2 sessions the first postoperative week; manual lymphatic massage: includes draining areas of swelling to the closest anatomic lymph node pool, as well as drainage of superficial fat areas that were treated |
| Niddam et al, 201922 | Cut-to-size plastic rods of 4 mm diameter were positioned along the liposuction muscle mass (10 days); these rods were held between 2 strips of adhesive tape to prevent skin damage | Conventional compression girdle for 21 extra days |
| Hoyos and Perez, 202037 | Garments and foam | Mild compression anti-DVT stockings (7 days) |
| Taha et al, 202024 | All patients were padded with cotton dressings and placed in a pressure garment | Daily dressing with fusidic acid around the drains; drains were removed after first postoperative week; antibiotics were prescribed if fat injection (1 week); pressure garment worn for 6 weeks—for most of the day in the first 3 weeks and during the day for the next 3 weeks; massage sessions: within POD 5 (every other day in the first week, twice per week in the second week, and then once per week) |
| Saad et al, 202127 | EpiFoam (Biodermis Inc., Henderson, NV) strips over the superficially sculpted regions in both anterior and posterior areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Admitted to the hospital for overnight observation and discharged on POD 1; lymphatic draining massage: 2 sessions starting the second postoperative week, followed by additional sessions as needed; compression garments for 3 weeks |
DVT, deep venous thrombosis; POD, postoperative day.
Immediate Postoperative Dressings and Postoperative Wound Protocol of Included Studies
| Author, year . | Immediate postoperative dressings . | Postoperative wound protocol . |
|---|---|---|
| Mentz et al, 199312 | Abdominal garment | Patient was placed in an abdominal garment; sutures were removed on POD 7, and exercise was allowed on POD 14 |
| Ersek and Salisbury, 19971 | Constricting corset with 0.5-inch rubber foam pad placed over the etched area | The patient is then placed in a constricting corset with 0.5-inch rubber foam pad placed over the etched area to prevent any unexpected folds |
| Hoyos et al, 20079 | Mild-compression garment; deep-vein thrombosis stockings; cotton-laminated soft foam band (4 weeks) | Oral antibiotic and anti-inflammatory drugs; after 48 hours, postoperative lymphatic drainage massages and adjunctive external ultrasound (once a day/10 days) |
| Monarca and Rizzo, 201526 | Elastocompressive dressing | Antithrombotic prophylaxis (1 week); elastocompressive dressing (10-15 days) |
| Steinbrech and Sinno, 201628 | Strips of Reston foam (3M, St Paul, MN) over the areas contoured (3-5 days); abdominal binder | Sponge bathes are acceptable until first postoperative visit; baths and swimming are not allowed for 3 weeks |
| Boeni, 202025 | Foam pads (Epifoam, Biodermis, Henderson, NV) to enhance definition lines (3 days); compression garments | Vitamin C (1000 mg) was given orally; compression garments (3 weeks); lymphatic drainage after 48 hours; endermology starting 1 month after surgery |
| Husain et al, 201921 | Compression over the etched areas with TopiFoam (Mentor-Aesthetics, Irvine, CA); abdominal binder | Binder with TopiFoam (2-3 days); compression garment (worn permanently for 2 weeks, part time for 2 weeks); heavy exercise (which involves core and/or trunk) delayed until 4 weeks postoperatively |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal pads, or 4x4 adhesive foam (Reston), and a binder | Foam dressing (1 week); compressive binder (2-6 weeks); exercise is allowed 5 days after surgery |
| Saad et al, 202023 | Compression foam (Epifoam) strips were applied over the superficially marked areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Lymphatic massage: 2 sessions the first postoperative week; manual lymphatic massage: includes draining areas of swelling to the closest anatomic lymph node pool, as well as drainage of superficial fat areas that were treated |
| Niddam et al, 201922 | Cut-to-size plastic rods of 4 mm diameter were positioned along the liposuction muscle mass (10 days); these rods were held between 2 strips of adhesive tape to prevent skin damage | Conventional compression girdle for 21 extra days |
| Hoyos and Perez, 202037 | Garments and foam | Mild compression anti-DVT stockings (7 days) |
| Taha et al, 202024 | All patients were padded with cotton dressings and placed in a pressure garment | Daily dressing with fusidic acid around the drains; drains were removed after first postoperative week; antibiotics were prescribed if fat injection (1 week); pressure garment worn for 6 weeks—for most of the day in the first 3 weeks and during the day for the next 3 weeks; massage sessions: within POD 5 (every other day in the first week, twice per week in the second week, and then once per week) |
| Saad et al, 202127 | EpiFoam (Biodermis Inc., Henderson, NV) strips over the superficially sculpted regions in both anterior and posterior areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Admitted to the hospital for overnight observation and discharged on POD 1; lymphatic draining massage: 2 sessions starting the second postoperative week, followed by additional sessions as needed; compression garments for 3 weeks |
| Author, year . | Immediate postoperative dressings . | Postoperative wound protocol . |
|---|---|---|
| Mentz et al, 199312 | Abdominal garment | Patient was placed in an abdominal garment; sutures were removed on POD 7, and exercise was allowed on POD 14 |
| Ersek and Salisbury, 19971 | Constricting corset with 0.5-inch rubber foam pad placed over the etched area | The patient is then placed in a constricting corset with 0.5-inch rubber foam pad placed over the etched area to prevent any unexpected folds |
| Hoyos et al, 20079 | Mild-compression garment; deep-vein thrombosis stockings; cotton-laminated soft foam band (4 weeks) | Oral antibiotic and anti-inflammatory drugs; after 48 hours, postoperative lymphatic drainage massages and adjunctive external ultrasound (once a day/10 days) |
| Monarca and Rizzo, 201526 | Elastocompressive dressing | Antithrombotic prophylaxis (1 week); elastocompressive dressing (10-15 days) |
| Steinbrech and Sinno, 201628 | Strips of Reston foam (3M, St Paul, MN) over the areas contoured (3-5 days); abdominal binder | Sponge bathes are acceptable until first postoperative visit; baths and swimming are not allowed for 3 weeks |
| Boeni, 202025 | Foam pads (Epifoam, Biodermis, Henderson, NV) to enhance definition lines (3 days); compression garments | Vitamin C (1000 mg) was given orally; compression garments (3 weeks); lymphatic drainage after 48 hours; endermology starting 1 month after surgery |
| Husain et al, 201921 | Compression over the etched areas with TopiFoam (Mentor-Aesthetics, Irvine, CA); abdominal binder | Binder with TopiFoam (2-3 days); compression garment (worn permanently for 2 weeks, part time for 2 weeks); heavy exercise (which involves core and/or trunk) delayed until 4 weeks postoperatively |
| Agochukwu-Nwubah and Mentz, 201920 | Abdominal pads, or 4x4 adhesive foam (Reston), and a binder | Foam dressing (1 week); compressive binder (2-6 weeks); exercise is allowed 5 days after surgery |
| Saad et al, 202023 | Compression foam (Epifoam) strips were applied over the superficially marked areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Lymphatic massage: 2 sessions the first postoperative week; manual lymphatic massage: includes draining areas of swelling to the closest anatomic lymph node pool, as well as drainage of superficial fat areas that were treated |
| Niddam et al, 201922 | Cut-to-size plastic rods of 4 mm diameter were positioned along the liposuction muscle mass (10 days); these rods were held between 2 strips of adhesive tape to prevent skin damage | Conventional compression girdle for 21 extra days |
| Hoyos and Perez, 202037 | Garments and foam | Mild compression anti-DVT stockings (7 days) |
| Taha et al, 202024 | All patients were padded with cotton dressings and placed in a pressure garment | Daily dressing with fusidic acid around the drains; drains were removed after first postoperative week; antibiotics were prescribed if fat injection (1 week); pressure garment worn for 6 weeks—for most of the day in the first 3 weeks and during the day for the next 3 weeks; massage sessions: within POD 5 (every other day in the first week, twice per week in the second week, and then once per week) |
| Saad et al, 202127 | EpiFoam (Biodermis Inc., Henderson, NV) strips over the superficially sculpted regions in both anterior and posterior areas; patients were placed in compression garments (Marena, Lawrenceville, GA) | Admitted to the hospital for overnight observation and discharged on POD 1; lymphatic draining massage: 2 sessions starting the second postoperative week, followed by additional sessions as needed; compression garments for 3 weeks |
DVT, deep venous thrombosis; POD, postoperative day.
Outcomes
Overall satisfaction ranged from 84% to 100%. Mentz et al reported a satisfaction of 100%, and results were above or at preoperative expectations in 87.5%.12 Husain et al reported a 95% satisfaction rate and most patients said that would have the procedure performed again.21 Saad et al reported an average satisfaction score of 9.2/10 at 1.5 months postoperatively, which increased to 9.8/10 over a period of 6 months.23 Niddam et al reported a satisfaction above 95%, whereas Hoyos et al reported a satisfaction index of 92%, considering “above expectations” and “good” as optimum results (Table 7).10,22
Surgical Outcomes of Aesthetic Abdominal High-Definition Lipoplasty in Male Patients
| Author, year . | Lipoaspirate (mL) . | Operative time (minutes) . | Outcomes . | Complications . | Follow-up (months) . |
|---|---|---|---|---|---|
| Mentz et al, 199312 | 581 | NR | Pre- and postoperative hemoglobin changes were minimal; patients resumed normal activities in 1-10 days and were back to regular exercise activities in 5-30 days; postoperative results were above or at preoperative expectations (87.5%, n = 7); 100% satisfaction (n = 8) | Severe pain (n = 1) | 3-8 |
| Ersek and Salisbury, 19971 | 1500-2400 | NR | All of patients very pleased with this procedure; bodybuilders find this to be of great benefit to their efforts; exaggerated groove at the level of the umbilicus that could not be completely corrected by repeated lipoplasty and fat grafting | Exaggerated groove at the level of the umbilicus (n = 2) | NS |
| Hoyos et al, 20079 | NR | NR | Secondary procedures were required to correct contour irregularities; despite the patient’s age, note the high muscular definition of the rectus abdominis, the obliques, and the pectoralis | Burns in the port areas; seromas; infections at port sites; localized residual fat deposits; generalized low fat extraction | ≥8 |
| Monarca and Rizzo, 201526 | NR | NR | Sculpted bodies with a trapezoid chest, pronounced alba and semilunar lines, evident muscular bulk and highlighted adherences, both in abdomen and in extremities (100%) | NR | NR |
| Steinbrech and Sinno, 201628 | Lower abdomen: 272; muscular inscriptions, 136; lateral abdomen: 313; flanks: 537 | NR | Fat grafting: lower “6-pack”, 42 mL each; middle “6-pack”, 58 mL each; upper “6-pack”, 55 mL each; and serratus muscle, 31 mL each; asymmetric abdominal muscle alignment relatively common in patients (n = 35); variability in fat resorption most significantly related to the age of the patient | Oil cyst (n = 1); fluid collection (n = 3); revision lipectomy (n = 1); seroma (n = 6); irregularities (n = 3); infection (n = 1); seroma requiring drain placement (n = 1) | 6-16 |
| Boeni, 202025 | NR | NR | HDL resulted in a more athletic appearance and pronounced muscular definition; touch-up surgery due to residual fat deposits in the hypogastrium (n = 2); touch-up surgery over the pectorals (n = 1) | Seroma (n = 2); touch-up surgery (n = 3) | >6 |
| Husain et al, 201921 | 500-9000 | NR | Most patients were satisfied (>96%) and would have the procedure performed again; no thermal injuries or full-thickness burns (although hyperpigmentation may be considered a minor burn) | Major complications (n = 0); contour irregularities (n ≤ 4); seroma (n ≤ 5); hyperpigmentation (n ≤ 1) | 27 |
| Agochukwu-Nwubah and Mentz, 201920 | 3325 (100-10,200) | NR | Number of patients: FAE (n = 160), MAE (n = 352); chest liposuction/pectoral etching with or without puncture glandular removal (n = 273) | No infections, no seroma, no skin necrosis; contour defects which required revisions (n = 3); no thromboembolic events | 36 (6-120) |
| Saad et al, 202023 | 4529 (2700-6100) | 206 (180-230) | Satisfaction score was 9.2 (range, 9-10) at 1.5 months and 9.8 (range, 9-10) at 6 months; all of the patients reported that they would undergo the procedure again; return to work: 6.1 days (range, 5-8); return to normal activity/exercise 22.7 days (range, 22-25) | Fluid collection detected inferomedial pectoral triangle (n = 1); fluid collection detected supragluteal region (n = 1) | 7.6 (4-12) |
| Niddam et al. 201922 | >500 | NR | The vast majority of patients (>95%) were happy or very happy; the majority of patients (>50%) reported an increase in their self-esteem and an improvement in their sexual life Weight of patients has not changed after the surgery. | No hematoma or infection was reported; no seroma was observed | >6 |
| Hoyos and Perez, 202037 | 500-9700 | NR | Mean volume of fat grafting: buttocks, 300 mL; pectorals, 150 mL; calves, 120 mL; deltoids, 80 mL; biceps, 50 mL; none of the patients reported poor results; the satisfaction index was >90% considering “above expectations” and “good” answers as the optimum results | Hyperchromia (n = 52); seroma (n = 18); retouch HD (n = 7); anemia (n = 7); hematoma/bruising (n = 5); dehiscence (n = 6); erratic skin adhesion (n = 2); burn (n = 4); necrosis (n = 1); infection (n = 2) | 2-24 |
| Taha et al, 202024 | NR | NR | Seroma incidence: group A, no adjunctive draining procedures (n = 13); group B, draining procedures added (n = 4) | Seroma (n = 17): lower abdomen (n = 11); back (n = 4); lower chest (n = 2) | 0.75 (0.5-1) |
| Saad et al, 202127 | 5021 [1062] (2700-7800) | 188.30 [16.18] (155-230) | Number of patients: MiD (n = 5), MoD (n = 17), and HD (n=28); no significant complications and no revisional surgeries; no significant difference in the lipoaspirated volumes between groups (P = 0.2); overall satisfaction (1-10): 9.1 [0.8]; MiD, 8.7 [0.8]; MoD, 9.1 [0.7]; HD, 9.3 [0.8] | Fluid collection in moderate definition (n=1); fluid collection in high definition (n=6); fibrosis of the linea alba (n=1) | 13 (6-24) |
| Author, year . | Lipoaspirate (mL) . | Operative time (minutes) . | Outcomes . | Complications . | Follow-up (months) . |
|---|---|---|---|---|---|
| Mentz et al, 199312 | 581 | NR | Pre- and postoperative hemoglobin changes were minimal; patients resumed normal activities in 1-10 days and were back to regular exercise activities in 5-30 days; postoperative results were above or at preoperative expectations (87.5%, n = 7); 100% satisfaction (n = 8) | Severe pain (n = 1) | 3-8 |
| Ersek and Salisbury, 19971 | 1500-2400 | NR | All of patients very pleased with this procedure; bodybuilders find this to be of great benefit to their efforts; exaggerated groove at the level of the umbilicus that could not be completely corrected by repeated lipoplasty and fat grafting | Exaggerated groove at the level of the umbilicus (n = 2) | NS |
| Hoyos et al, 20079 | NR | NR | Secondary procedures were required to correct contour irregularities; despite the patient’s age, note the high muscular definition of the rectus abdominis, the obliques, and the pectoralis | Burns in the port areas; seromas; infections at port sites; localized residual fat deposits; generalized low fat extraction | ≥8 |
| Monarca and Rizzo, 201526 | NR | NR | Sculpted bodies with a trapezoid chest, pronounced alba and semilunar lines, evident muscular bulk and highlighted adherences, both in abdomen and in extremities (100%) | NR | NR |
| Steinbrech and Sinno, 201628 | Lower abdomen: 272; muscular inscriptions, 136; lateral abdomen: 313; flanks: 537 | NR | Fat grafting: lower “6-pack”, 42 mL each; middle “6-pack”, 58 mL each; upper “6-pack”, 55 mL each; and serratus muscle, 31 mL each; asymmetric abdominal muscle alignment relatively common in patients (n = 35); variability in fat resorption most significantly related to the age of the patient | Oil cyst (n = 1); fluid collection (n = 3); revision lipectomy (n = 1); seroma (n = 6); irregularities (n = 3); infection (n = 1); seroma requiring drain placement (n = 1) | 6-16 |
| Boeni, 202025 | NR | NR | HDL resulted in a more athletic appearance and pronounced muscular definition; touch-up surgery due to residual fat deposits in the hypogastrium (n = 2); touch-up surgery over the pectorals (n = 1) | Seroma (n = 2); touch-up surgery (n = 3) | >6 |
| Husain et al, 201921 | 500-9000 | NR | Most patients were satisfied (>96%) and would have the procedure performed again; no thermal injuries or full-thickness burns (although hyperpigmentation may be considered a minor burn) | Major complications (n = 0); contour irregularities (n ≤ 4); seroma (n ≤ 5); hyperpigmentation (n ≤ 1) | 27 |
| Agochukwu-Nwubah and Mentz, 201920 | 3325 (100-10,200) | NR | Number of patients: FAE (n = 160), MAE (n = 352); chest liposuction/pectoral etching with or without puncture glandular removal (n = 273) | No infections, no seroma, no skin necrosis; contour defects which required revisions (n = 3); no thromboembolic events | 36 (6-120) |
| Saad et al, 202023 | 4529 (2700-6100) | 206 (180-230) | Satisfaction score was 9.2 (range, 9-10) at 1.5 months and 9.8 (range, 9-10) at 6 months; all of the patients reported that they would undergo the procedure again; return to work: 6.1 days (range, 5-8); return to normal activity/exercise 22.7 days (range, 22-25) | Fluid collection detected inferomedial pectoral triangle (n = 1); fluid collection detected supragluteal region (n = 1) | 7.6 (4-12) |
| Niddam et al. 201922 | >500 | NR | The vast majority of patients (>95%) were happy or very happy; the majority of patients (>50%) reported an increase in their self-esteem and an improvement in their sexual life Weight of patients has not changed after the surgery. | No hematoma or infection was reported; no seroma was observed | >6 |
| Hoyos and Perez, 202037 | 500-9700 | NR | Mean volume of fat grafting: buttocks, 300 mL; pectorals, 150 mL; calves, 120 mL; deltoids, 80 mL; biceps, 50 mL; none of the patients reported poor results; the satisfaction index was >90% considering “above expectations” and “good” answers as the optimum results | Hyperchromia (n = 52); seroma (n = 18); retouch HD (n = 7); anemia (n = 7); hematoma/bruising (n = 5); dehiscence (n = 6); erratic skin adhesion (n = 2); burn (n = 4); necrosis (n = 1); infection (n = 2) | 2-24 |
| Taha et al, 202024 | NR | NR | Seroma incidence: group A, no adjunctive draining procedures (n = 13); group B, draining procedures added (n = 4) | Seroma (n = 17): lower abdomen (n = 11); back (n = 4); lower chest (n = 2) | 0.75 (0.5-1) |
| Saad et al, 202127 | 5021 [1062] (2700-7800) | 188.30 [16.18] (155-230) | Number of patients: MiD (n = 5), MoD (n = 17), and HD (n=28); no significant complications and no revisional surgeries; no significant difference in the lipoaspirated volumes between groups (P = 0.2); overall satisfaction (1-10): 9.1 [0.8]; MiD, 8.7 [0.8]; MoD, 9.1 [0.7]; HD, 9.3 [0.8] | Fluid collection in moderate definition (n=1); fluid collection in high definition (n=6); fibrosis of the linea alba (n=1) | 13 (6-24) |
Values are mean [standard deviation] (range) where applicable. FAE, full abdominal etching; HD(L), high-definition (liposuction); MAE, modified abdominal etching; MiD, mild definition; MoD, moderate definition; NS, not specified; NR, not reported.
Surgical Outcomes of Aesthetic Abdominal High-Definition Lipoplasty in Male Patients
| Author, year . | Lipoaspirate (mL) . | Operative time (minutes) . | Outcomes . | Complications . | Follow-up (months) . |
|---|---|---|---|---|---|
| Mentz et al, 199312 | 581 | NR | Pre- and postoperative hemoglobin changes were minimal; patients resumed normal activities in 1-10 days and were back to regular exercise activities in 5-30 days; postoperative results were above or at preoperative expectations (87.5%, n = 7); 100% satisfaction (n = 8) | Severe pain (n = 1) | 3-8 |
| Ersek and Salisbury, 19971 | 1500-2400 | NR | All of patients very pleased with this procedure; bodybuilders find this to be of great benefit to their efforts; exaggerated groove at the level of the umbilicus that could not be completely corrected by repeated lipoplasty and fat grafting | Exaggerated groove at the level of the umbilicus (n = 2) | NS |
| Hoyos et al, 20079 | NR | NR | Secondary procedures were required to correct contour irregularities; despite the patient’s age, note the high muscular definition of the rectus abdominis, the obliques, and the pectoralis | Burns in the port areas; seromas; infections at port sites; localized residual fat deposits; generalized low fat extraction | ≥8 |
| Monarca and Rizzo, 201526 | NR | NR | Sculpted bodies with a trapezoid chest, pronounced alba and semilunar lines, evident muscular bulk and highlighted adherences, both in abdomen and in extremities (100%) | NR | NR |
| Steinbrech and Sinno, 201628 | Lower abdomen: 272; muscular inscriptions, 136; lateral abdomen: 313; flanks: 537 | NR | Fat grafting: lower “6-pack”, 42 mL each; middle “6-pack”, 58 mL each; upper “6-pack”, 55 mL each; and serratus muscle, 31 mL each; asymmetric abdominal muscle alignment relatively common in patients (n = 35); variability in fat resorption most significantly related to the age of the patient | Oil cyst (n = 1); fluid collection (n = 3); revision lipectomy (n = 1); seroma (n = 6); irregularities (n = 3); infection (n = 1); seroma requiring drain placement (n = 1) | 6-16 |
| Boeni, 202025 | NR | NR | HDL resulted in a more athletic appearance and pronounced muscular definition; touch-up surgery due to residual fat deposits in the hypogastrium (n = 2); touch-up surgery over the pectorals (n = 1) | Seroma (n = 2); touch-up surgery (n = 3) | >6 |
| Husain et al, 201921 | 500-9000 | NR | Most patients were satisfied (>96%) and would have the procedure performed again; no thermal injuries or full-thickness burns (although hyperpigmentation may be considered a minor burn) | Major complications (n = 0); contour irregularities (n ≤ 4); seroma (n ≤ 5); hyperpigmentation (n ≤ 1) | 27 |
| Agochukwu-Nwubah and Mentz, 201920 | 3325 (100-10,200) | NR | Number of patients: FAE (n = 160), MAE (n = 352); chest liposuction/pectoral etching with or without puncture glandular removal (n = 273) | No infections, no seroma, no skin necrosis; contour defects which required revisions (n = 3); no thromboembolic events | 36 (6-120) |
| Saad et al, 202023 | 4529 (2700-6100) | 206 (180-230) | Satisfaction score was 9.2 (range, 9-10) at 1.5 months and 9.8 (range, 9-10) at 6 months; all of the patients reported that they would undergo the procedure again; return to work: 6.1 days (range, 5-8); return to normal activity/exercise 22.7 days (range, 22-25) | Fluid collection detected inferomedial pectoral triangle (n = 1); fluid collection detected supragluteal region (n = 1) | 7.6 (4-12) |
| Niddam et al. 201922 | >500 | NR | The vast majority of patients (>95%) were happy or very happy; the majority of patients (>50%) reported an increase in their self-esteem and an improvement in their sexual life Weight of patients has not changed after the surgery. | No hematoma or infection was reported; no seroma was observed | >6 |
| Hoyos and Perez, 202037 | 500-9700 | NR | Mean volume of fat grafting: buttocks, 300 mL; pectorals, 150 mL; calves, 120 mL; deltoids, 80 mL; biceps, 50 mL; none of the patients reported poor results; the satisfaction index was >90% considering “above expectations” and “good” answers as the optimum results | Hyperchromia (n = 52); seroma (n = 18); retouch HD (n = 7); anemia (n = 7); hematoma/bruising (n = 5); dehiscence (n = 6); erratic skin adhesion (n = 2); burn (n = 4); necrosis (n = 1); infection (n = 2) | 2-24 |
| Taha et al, 202024 | NR | NR | Seroma incidence: group A, no adjunctive draining procedures (n = 13); group B, draining procedures added (n = 4) | Seroma (n = 17): lower abdomen (n = 11); back (n = 4); lower chest (n = 2) | 0.75 (0.5-1) |
| Saad et al, 202127 | 5021 [1062] (2700-7800) | 188.30 [16.18] (155-230) | Number of patients: MiD (n = 5), MoD (n = 17), and HD (n=28); no significant complications and no revisional surgeries; no significant difference in the lipoaspirated volumes between groups (P = 0.2); overall satisfaction (1-10): 9.1 [0.8]; MiD, 8.7 [0.8]; MoD, 9.1 [0.7]; HD, 9.3 [0.8] | Fluid collection in moderate definition (n=1); fluid collection in high definition (n=6); fibrosis of the linea alba (n=1) | 13 (6-24) |
| Author, year . | Lipoaspirate (mL) . | Operative time (minutes) . | Outcomes . | Complications . | Follow-up (months) . |
|---|---|---|---|---|---|
| Mentz et al, 199312 | 581 | NR | Pre- and postoperative hemoglobin changes were minimal; patients resumed normal activities in 1-10 days and were back to regular exercise activities in 5-30 days; postoperative results were above or at preoperative expectations (87.5%, n = 7); 100% satisfaction (n = 8) | Severe pain (n = 1) | 3-8 |
| Ersek and Salisbury, 19971 | 1500-2400 | NR | All of patients very pleased with this procedure; bodybuilders find this to be of great benefit to their efforts; exaggerated groove at the level of the umbilicus that could not be completely corrected by repeated lipoplasty and fat grafting | Exaggerated groove at the level of the umbilicus (n = 2) | NS |
| Hoyos et al, 20079 | NR | NR | Secondary procedures were required to correct contour irregularities; despite the patient’s age, note the high muscular definition of the rectus abdominis, the obliques, and the pectoralis | Burns in the port areas; seromas; infections at port sites; localized residual fat deposits; generalized low fat extraction | ≥8 |
| Monarca and Rizzo, 201526 | NR | NR | Sculpted bodies with a trapezoid chest, pronounced alba and semilunar lines, evident muscular bulk and highlighted adherences, both in abdomen and in extremities (100%) | NR | NR |
| Steinbrech and Sinno, 201628 | Lower abdomen: 272; muscular inscriptions, 136; lateral abdomen: 313; flanks: 537 | NR | Fat grafting: lower “6-pack”, 42 mL each; middle “6-pack”, 58 mL each; upper “6-pack”, 55 mL each; and serratus muscle, 31 mL each; asymmetric abdominal muscle alignment relatively common in patients (n = 35); variability in fat resorption most significantly related to the age of the patient | Oil cyst (n = 1); fluid collection (n = 3); revision lipectomy (n = 1); seroma (n = 6); irregularities (n = 3); infection (n = 1); seroma requiring drain placement (n = 1) | 6-16 |
| Boeni, 202025 | NR | NR | HDL resulted in a more athletic appearance and pronounced muscular definition; touch-up surgery due to residual fat deposits in the hypogastrium (n = 2); touch-up surgery over the pectorals (n = 1) | Seroma (n = 2); touch-up surgery (n = 3) | >6 |
| Husain et al, 201921 | 500-9000 | NR | Most patients were satisfied (>96%) and would have the procedure performed again; no thermal injuries or full-thickness burns (although hyperpigmentation may be considered a minor burn) | Major complications (n = 0); contour irregularities (n ≤ 4); seroma (n ≤ 5); hyperpigmentation (n ≤ 1) | 27 |
| Agochukwu-Nwubah and Mentz, 201920 | 3325 (100-10,200) | NR | Number of patients: FAE (n = 160), MAE (n = 352); chest liposuction/pectoral etching with or without puncture glandular removal (n = 273) | No infections, no seroma, no skin necrosis; contour defects which required revisions (n = 3); no thromboembolic events | 36 (6-120) |
| Saad et al, 202023 | 4529 (2700-6100) | 206 (180-230) | Satisfaction score was 9.2 (range, 9-10) at 1.5 months and 9.8 (range, 9-10) at 6 months; all of the patients reported that they would undergo the procedure again; return to work: 6.1 days (range, 5-8); return to normal activity/exercise 22.7 days (range, 22-25) | Fluid collection detected inferomedial pectoral triangle (n = 1); fluid collection detected supragluteal region (n = 1) | 7.6 (4-12) |
| Niddam et al. 201922 | >500 | NR | The vast majority of patients (>95%) were happy or very happy; the majority of patients (>50%) reported an increase in their self-esteem and an improvement in their sexual life Weight of patients has not changed after the surgery. | No hematoma or infection was reported; no seroma was observed | >6 |
| Hoyos and Perez, 202037 | 500-9700 | NR | Mean volume of fat grafting: buttocks, 300 mL; pectorals, 150 mL; calves, 120 mL; deltoids, 80 mL; biceps, 50 mL; none of the patients reported poor results; the satisfaction index was >90% considering “above expectations” and “good” answers as the optimum results | Hyperchromia (n = 52); seroma (n = 18); retouch HD (n = 7); anemia (n = 7); hematoma/bruising (n = 5); dehiscence (n = 6); erratic skin adhesion (n = 2); burn (n = 4); necrosis (n = 1); infection (n = 2) | 2-24 |
| Taha et al, 202024 | NR | NR | Seroma incidence: group A, no adjunctive draining procedures (n = 13); group B, draining procedures added (n = 4) | Seroma (n = 17): lower abdomen (n = 11); back (n = 4); lower chest (n = 2) | 0.75 (0.5-1) |
| Saad et al, 202127 | 5021 [1062] (2700-7800) | 188.30 [16.18] (155-230) | Number of patients: MiD (n = 5), MoD (n = 17), and HD (n=28); no significant complications and no revisional surgeries; no significant difference in the lipoaspirated volumes between groups (P = 0.2); overall satisfaction (1-10): 9.1 [0.8]; MiD, 8.7 [0.8]; MoD, 9.1 [0.7]; HD, 9.3 [0.8] | Fluid collection in moderate definition (n=1); fluid collection in high definition (n=6); fibrosis of the linea alba (n=1) | 13 (6-24) |
Values are mean [standard deviation] (range) where applicable. FAE, full abdominal etching; HD(L), high-definition (liposuction); MAE, modified abdominal etching; MiD, mild definition; MoD, moderate definition; NS, not specified; NR, not reported.
The mean operative time was 191.7 minutes (range, 155-230 minutes), reported in 2 articles.23,27 The average lipoaspirate was reported in 9 articles.1,10,12,20-22,27 The average lipoaspirate with abdominal etching was 3325 mL (range 100-10,200 mL) and the mean lipoaspirate following HDL and HD2 was 4925.77 mL (range of means, 500-9700 mL) (Table 7).1,10,12,20-22,27
Complications
Reported complications are shown in Table 7. Complications were not reported in 1 study,26 and were not explicitly reported for male liposuction in 1 article.9 Fluid collection or seroma formation was the most common complication, reported in 60 patients, followed by hyperpigmentation (n = 53), contour irregularities (n = 11), revision surgery (n = 11), anemia (n = 7), port dehiscence (n = 6), and hematoma or bruising (n = 5). Other complications reported were severe pain (n = 1), an exaggerated groove at the level of the umbilicus (n = 1), an oil cyst (n = 1), erratic skin adhesion or fibrosis (n = 3), and necrosis (n = 2). An additional indentation at the level of the umbilicus turned out to be an exaggerated groove as a result of sitting. The authors were unable to completely correct the groove by repeated fat injections and liposuction.1
Taha et al reported a seroma rate of 52% in a standard group in comparison to 16% in patients treated with draining procedures (evacuation of the infiltrate through the incision sites at the end of the procedure, cannula sites left open to help drainage, early ambulation, compressive garments, and silicone drains at the inguinal and iliac regions).24
DISCUSSION
Subcutaneous adipose tissue (SAT) differs anatomically and functionally from intra-abdominal visceral fat, but is nevertheless still deleterious to health and generates a dissonant and amorphous appearance of the body.26,30 SAT in males tends to accumulate in the anterior abdominal region where the topographic anatomy of the abdominal musculature cannot be visualized, even with an adequate muscle volume if the total body fat is beyond 15%.12 Additionally, the chest acquires a gynecoid semblance and the SAT of arms and legs does not undergo hyperplastic changes in the same proportion as the torso, giving a thin appearance to the limbs.26
Traditional SAL integrates wet techniques and deep lipoplasty while preserving a quantity of subcutaneous fat to avoid contour irregularities and wrinkling.9,26,31 Nonetheless, this approach is not comprehensive and does not offer athletic-build results.26,31 In 1993 Mentz et al described the technique of “abdominal etching,” which aimed to enhance the details of the abdominal wall musculature by applying differential liposuction.12 However, this technique was limited to the anterior abdominal wall. In 2003, Hoyos presented the technique of “high-definition liposculpture” at the Colombian National Congress where lipoplasty was not only performed to remove fat but to outline the superficial anatomy of the body.32 This technique was further developed and improved with the inclusion of VASER-assisted liposuction to perform HDL with a precision technique for abdominal etching with the integration of a 3-dimensional multilayer concept of body contouring for the entire torso, lower and upper extremities, and back.9 Finally, the latest concept of HD2 not only includes the concept of the body as a whole homogeneous unit described with HDL, but incorporates a finely detailed definition of musculature based on the pattern of precise muscle movements by creating “dynamic zones,” predicting the form of muscles during physical activity.13,14
All the aforementioned concepts include abdominal etching by creating controlled irregularities at the linea alba, the linea semilunaris bilaterally, as well as the inscriptions of the rectus abdominis muscles.22,26 Remarkably, the transverse inscriptions can be arranged as an intersection in a transverse direction, extending perpendicular to the linea alba; in an oblique fashion; a biphasic type of inscription; or in a stair-step configuration, in which the levels of the intersections can differ from side to side by several millimeters in the vertical axis.12,22,28,33 Therefore, this asymmetry should be respected because the purpose of abdominal HDL is to accentuate a natural result and normal anatomy.22
Regarding the lowest insertion at the level of the umbilicus, several authors recommended avoiding horizontal liposuction at or below this point because it creates an exaggerated and artificial appearance of such lines.1 Moreover, the linea alba should mainly be visible and marked above the umbilicus and not below in order to achieve more natural outcomes.22 Finally, several authors mentioned it was also necessary to etch a 2- to 3-cm radius around the umbilicus to prevent a periumbilical “doughnut.” 20
A common challenge faced during HDL or HD2 is artificial or unrealistic results, which occur when the surgeon does not identify the patient biotype and mistakenly applies HDL as a standardized procedure to every patient.10 In response to this, Hoyos et al implemented a BMX algorithm in which an endomorphic (overweight) biotype, or patients who desire moderate definition receive basic (mild) to moderate HDL mainly to extract a significant volume of fat and etch the underlying musculature; whereas patients with mesomorphic or ectomorphic biotypes receive a moderate to extreme (aggressive) HDL, focused mainly on reproducing an athletic appearance.10,13,14 Saad et al reported a similar approach in which the extent of definition was decided through a consensus between the patient and the surgeon, taking into consideration the patient’s body habitus, anatomy, and expectations.27 Although these approaches provide a clear and explanatory algorithm,10,27 the reproducibility in terms of surgical outcomes for less-experienced surgeons remains a critical concern due to the limited number of studies.
Regarding the different technologies, VASER-assisted HDL has a more measured learning curve and is more time-consuming than traditional lipoplasty. However, several authors have reported better outcomes, with a low complication rate, by never letting the skin become warmer than the hand of the surgeon and limiting the cannula to a maximum of 10 passes in the subdermal plane.9 The fragmentation of all the deep, intermediate, and subdermal lamellae SAT is gentle and precise, avoiding the morbidity associated with multilayer techniques. In addition, the superficial emulsification addresses the subcutaneous plane, thus allowing augmented skin retraction in areas of muscle or fascial laxity.9,34 On the other hand, PAL is an intensification of SAL that involves a rapidly reciprocating cannula tip, which replicates the “back-and-forth” motion of the surgeon’s arm but at an amplitude of 3 mm. In previous series, PAL has been shown to reduce vascular injury, increase the overall efficiency, and provide a favorable cost-benefit ratio in comparison to SAL and vibration-assisted liposuction.23,35 However, due to the divergent methodologic protocols applied in the included studies and the lack of a control group or a comparative cohort, pairwise comparison in terms of outcomes, effectiveness, and complications remains uncertain among surgical technologies, hindering the formulation of further recommendations in favor of a particular technique.36,37
Niddam et al avoided injecting fat in the rectus abdominis muscles or in the deep layers of the skin to increase the volume of the rectus abdominis because of the associated morbidity and the eccentric appearance. Instead, they found that the regions of gluteus maximus muscle, the deltoid muscle, or the pectoralis major muscle were more suitable for fat injection to increase volume in a more natural fashion.22 Hoyos et al did not include rectus abdominis fat grafting because most of the patients did not desire a fat-grafted appearance over the abdominal musculature.21 In comparison, Steinbrech and Sinno reported superior abdominal contouring results when they performed selective lipocontouring with fat grafting, specially over the rectus abdominis and the serratus anterior to provide a bodybuilder-like appearance.28
In this setting, if muscle expansion is still desired in the rectus abdominis, ultrasound-guided rectus abdominis fat transfer has been described as a safe approach for this purpose.38 With this modality, fat is administered below the anterior rectus sheath, avoiding a posterior approach where the inferior epigastric vessels are located.38 Additionally, the bolus injection technique is preferred because the ultrasound image becomes distorted once fat injection is started, preventing fat from being delivered in a precise and safe way if the cannula is in motion.38
Interventions directed to decrease seroma and hematoma formation are extremely important in HDL because minor seromas can have devastating consequences.21 Therefore, seromas are managed with aggressive aspiration and compression to preclude the obliteration of sculpted regions.9 Some authors left open (<1.5 cm) the stab incisions to allow for drainage and prevent seroma/hematoma formation. Nevertheless, when excessive drainage was expected, drains were sometimes used.21 In these cases, the incidence of seroma dramatically decreased with the use of drains in the inguinal area in male patients.9 In addition to drains, evacuation of all the infiltrate through the incision sites at the end of the procedure, tight dressings applied over superficially treated areas, pressure garments applied immediately after the procedure and worn for 6 weeks, early ambulation, and massage therapy for 4 weeks, were shown to significantly reduce the incidence of seroma (P < 0.007) in comparison to nondraining interventions.24 However, further studies with an increased sample size are required to increase the strength of these recommendations for HDL and to adequately ascertain the benefits of these postoperative protocols.39
Other common minor complications of liposuction include bruising or pigmentation, and contour deformities; more serious complications include infection, lidocaine toxicity, anemia, hypovolemic shock, thromboembolism, and death.21,40 Skin laxity, particularly above the umbilicus, caused postoperative wrinkling in older and sun-damaged patients; issues with waviness usually occurred below the umbilicus.20 This highlights the importance of evaluating skin features and laxity preoperatively and assessing the thickness irregularities intraoperatively.20
Finally, patient selection for this procedure is paramount because preservation of long-term results is reliant on patient motivation, adherence to a diet, and an exercise regimen.9,20 Conversely, weight gain can negatively impact long-term results and reduce the definition of the abdominal wall musculature.20 In fact, patients who receive this procedure and gain weight eventually require further SAL but are likely to have an evident deformity with an artificial etched 6-pack over an obese abdomen.20
Limitations
Quantitative analysis was limited due to the sample size of some studies. Complications were not reported ubiquitously. Most studies had a OCEBM score of 4 and were limited to single-arm cohort studies or were case series, which limited comparability among surgical techniques. Satisfaction was not reported according to standardized scales in the majority of studies.
CONCLUSIONS
A wide variety of techniques are available to perform HDL to achieve various degrees of definition. However, careful patient selection is critical for successful results; the concept of “one type of definition fits all” must unequivocally be abandoned.10,27 The different liposuction techniques are technically moderate/complex; therefore, proper training with a straightforward learning curve and adequate knowledge of the superficial anatomy of bodies are necessary to avoid complications and achieve optimum results.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES



