-
PDF
- Split View
-
Views
-
Cite
Cite
Jeong Hyun Ha, Young Oh Park, Ung Sik Jin, Revisional Medial Epicanthoplasty Using Reverse Z-Plasty Technique, Aesthetic Surgery Journal, Volume 42, Issue 1, January 2022, Pages 10–15, https://doi.org/10.1093/asj/sjab091
Close - Share Icon Share
Abstract
Medial epicanthoplasty is a common method for correcting epicanthal folds in Asians but sometimes cause unsatisfactory results. Although several procedural variations have been devised, revision techniques have earned little attention. The revision technique the authors have developed employs reverse Z-plasty to restore an overcorrected epicanthal fold.
The aim of this study was to investigate the effectiveness of the authors’ reverse Z-plasty technique in restoring natural medial canthal region harmonizing with Asian face.
From January 2010 to December 2016, reverse Z-plasty was performed in patients seeking revisions after previous medial epicanthoplasties. Patients were surveyed to assess their satisfaction with surgical outcomes. Interepicanthal distance-lengthening ratios and symmetry of palpebral widths were evaluated digitally (ImageJ software) in patients who received revisional epicanthoplasty only.
The reverse Z-plasty technique for revisional epicanthoplasty was performed in 548 Asian patients (83 males, 460 females). Most patients were pleased with the final outcomes. Only 6% submitted to later revisions of scars, which were otherwise scarcely visible after 3 months. Among 60 patients who underwent only revisional epicanthoplasty, interepicanthal distance-lengthening ratios ranged from 2.9% to 31.1% (average, 8.6%), and palpebral width symmetries improved.
This particular technique helps restore the 3-dimensional appearance of medial canthal angle through horizontal skin and soft tissue (including muscle and ligament) restructuring, thus compensating for tissue deficiency. It is simple in design, easy to perform, and satisfactory results were achieved, conferring natural aesthetics to the medial canthal region.

Medial epicanthal folds are characteristic of Asian eyelids, marked by thick skin and muscle, excess fat, absence of superior palpebral fold, or pretarsal fold laxity.1 The web-like covering created in this region imparts a rounded appearance. It leads to shortening of palpebral fissure, often diminishing the potential beauty of the eyelids. The incidence of epicanthal folds is estimated at over 50% in Asian populations and is particularly high (50%-90%) in Korean or Japanese nationalities.2 Many Asians wish to correct their medial canthal areas, desiring a horizontal-lengthening effect. Medial epicanthoplasty may also be performed concurrently with double eyelidplasty when medial epicanthal folds may be tense and prominent if uncorrected. However, overall harmony while maintaining the ethnic identity should be considered because Western eyelids do not compliment the Asian face.3
Since the introduction of epicanthal fold correction by von Ammon, various techniques have been devised and modified.1 Mustardé 4 originated the 4-flap technique, which was further modified by Yoon.5 V-W plasty,6 V-Y advancement flap,4 modified Y-V advancement flap,7,8 W-plasty,9 and Z-plasty10-13 at the epicanthal fold, as well as the re-draping method,1 are some of the procedures utilized for epicanthal fold correction. Some have suggested that individual characteristics, including type and degree of epicanthal fold, dictate the choice of technique.14 In this regard, Wang et al15 believe the severity of the epicanthal fold is key, whereas Park et al16 have generated an algorithm for selecting epicanthoplasty method based on preoperative interepicanthal distance (ICD). These techniques generally make the eyes appear much wider and larger, conveying a softer and kinder impression. However, inappropriate manipulation of the medial canthus may produce undesired results. Ectropion, asymmetrical medial commissures, scarring, and visible sclerae may be problematic. Even without definite complication, excessive lacrimal lake exposure or short ICD making the eyes seem closer together may cause dissatisfaction with Asian patients. Protruding or reddish lacrimal caruncle may also appear unnatural.17 In such circumstances, revisional surgery is entirely warranted, but the techniques reported for doing so are limited.
We reversely employed one of the standard techniques for medial epicanthoplasty, the Z-plasty, to correct unfavorable results. Reverse Z-plasty helps to regain the 3-dimensional (3D) integrity of medial canthal areas. While enabling the manipulation of the damaged muscle or canthal ligaments with minimal scar, it can effectively resolve unsatisfactory appearances from previous surgery.
METHODS
Employing the reverse Z-plasty method, 548 consecutive patients underwent 3D revision epicanthoplasty between January 2010 and December 2016. Patients were preoperatively assessed for complaints leading to surgical revisions. Visual examinations were conducted along with screenings for hypertrophic scars, ectropion, excessive lacrimal lake exposure, and asymmetry. Perioperative photographs were routinely taken from all patients. After receiving approval from the Seoul National University Hospital Institutional Review Board (IRB No. H-2003-161-1113), we reviewed the patients' demographic data, medical information, and photographs. Waivers of informed consent was approved by the Institutional Review Board. The study was conducted in accordance with the guidelines set forth in the Declaration of Helsinki.
Surgical Technique
The surgical procedure (Figure 1) was performed under local anesthesia, with patients in the supine position. Point (a) was marked at the existing location of the medial canthus. Point (b) was an imaginary spot considered the desired medial canthus point. A curvilinear line was drawn from (a) to (b) as a continuous smooth arc. Point (a’) was marked near the area where the medial edge of canthal tendon was projected. Point (b’) was defined as a surface representation of the most medial point of the lacrimal lake. These points were adjusted as required by the severity of previous surgical scars (Figure 2).
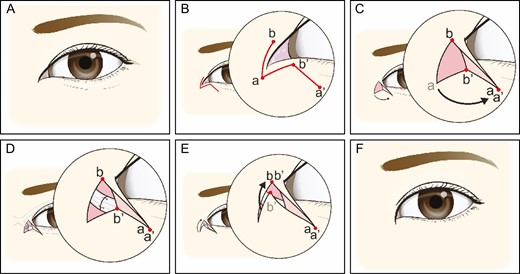
Schematic illustration of surgical technique. (A) Overcorrected medial epicanthus requiring revision medial epicanthoplasty. (B) Point (a) was marked at the existing location of medial canthus. Point (b) was an imaginary spot considered the desired medial canthus point. A curvilinear line was drawn from (a) to (b) as a continuous smooth arc. Point (a’) was marked near the area where the medial edge of canthal tendon was projected. Point (b’) was defined as a surface representation of the most medial point of lacrimal lake. These points were adjusted as required by severity of prior surgical scars. (C) A skin incision was created along the line b-a-b’, and the triangular flap was flipped over b-a-b’ and was anchored to point (a’). (D) Then subcutaneous dissection was performed, undermining the medial area, and residual scar tissue was removed as necessary. Medial canthal tendon and orbicularis oculi muscle were then exposed, utilizing 6-0 Vicryl suture to reposition/realign damaged muscle and canthus. (E) On completion, the skin was closed. (F) Three-dimensionally restored medial epicanthus.
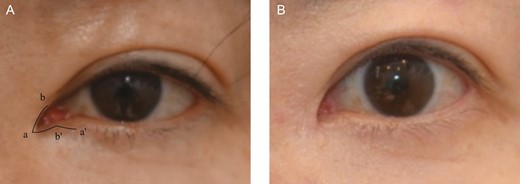
This 46-year-old female patient received the 3-dimensional restoration of medial epicanthus employing the reverse Z-plasty technique. (A) Preoperative photograph with view design and (B) 6-month postoperative view.
A local anesthetic was injected at the designated site (ie, medial canthal area and medial aspect of lower eyelid region). A skin incision was made along the line b-a-b’. We then flipped the triangular flap over b-a-b’ and anchored it to point (a’) with a 6-0 nylon suture. This technique eliminates underlying dead space and forms a natural canthal web. Once point (a) was anchored to point (a’), subcutaneous dissection was performed, undermining the medial area, and residual scar tissue was removed as necessary. Medial canthal tendon and orbicularis oculi muscle were then exposed, utilizing 6-0 PDS or Monosyn suture to reposition/realign damaged muscle and canthus. On completion, the skin was closed (Video).
Assessment of Outcomes
Patients were routinely asked for their overall satisfaction during their clinical visit based on cosmetic appearance and scarring of the medial canthal area. Patient satisfaction was evaluated in 4 grades: poor, fair, good, and excellent.
Photographic analysis was performed in patients who took postoperative photographs after 3 months and who underwent medial epicanthoplasty alone without other eyelid procedures, including double eyelidplasty, lateral canthoplasty, or lower blepharoplasty. We measured the ICD, outer canthal distance (OCD), and palpebral width before and after surgery using ImageJ open-source software (US National Institutes of Health, Bethesda, MD). Improvement in short ICD measurements was gauged by comparing ratios of ICD to OCD. In analyzing ICD increases, the following formula for lengthening ratio was applied: (postoperative [ICD/OCD] – preoperative [ICD/OCD]) / preoperative (ICD/OCD) × 100%.2 The symmetry index of palpebral widths was calculated as follows: | palpebral width (right) / palpebral width (left) −1 |. Absolute values were utilized (Figure 3).
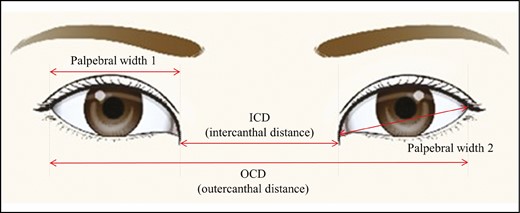
Schematic presentation of interepicanthal distance (ICD), outer canthal distance (OCD), and palpebral width.
RESULTS
Patient Characteristics
A total of 548 patients (88 males, 460 females) underwent 3D revision- epicanthoplasty during the study period. The mean age at surgery was 25 years (range, 17-53 years), and the average follow-up period was 10.3 months (range, 6-24 months). The chief complaints leading to revision procedures included dissatisfaction of the shape, prominent scarring, tissue contracture, loss of pretarsal fullness, and ectropion. Revision epicanthoplasty only was performed in 60 patients, and their photographs were analyzed for measurements.
Assessment of Outcomes
During close follow-up, all patients rated their satisfaction score. A total of 97% (532/548) of patients reported that the medial epicanthus was sufficiently restored (poor, 1 [0.2%]; fair, 15 [2.7%]; good, 402 [73.4%]; excellent, 130 [23.7%]). None experienced abnormal lacrimal drainage function postoperatively. One-stitch abscess was reported in a single instance as a postoperative complication. In terms of scarring, 94% (515/548) of patients felt that existing scars were improved, whereas 6% underwent re-revisions of scars. The scars from reverse Z-plasty remained visible for the first 1 to 2 months but were barely noticeable after 3 months.
Also, 60 patients who had photographs of 3 months after the surgery and who underwent revisional epicanthoplasty only underwent photographic analysis. Among these patients, ICD-lengthening ratios ranged from 2.9% to 24.3% (average 8.4%), and the symmetry of palpebral width was improved after surgery. Symmetry indices of palpebral widths 1 and 2 shifted from 0.044 to 0.025 and from 0.041 to 0.023, respectively (representative preoperative and postoperative figures are depicted in Figures 4-7).

(A) Preoperative view and (B) 12-month postoperative view of this 27-year-old female patient.

(A) Preoperative view and (B) 12-month postoperative view of this 27-year-old male patient.

(A) Preoperative view and (B) 12-month postoperative view of this 35-year-old female patient.

(A) Preoperative view and (B) 12-month postoperative view of this 29-year-old female patient.
Discussion
Medial epicanthoplasty is aimed at correcting the excess skin, fibrofatty tissue, and muscle within these folds and releasing the tension created.2 Unfortunately, the outcomes of epicanthoplasty are often displeasing. Inadequate dissection may damage soft tissue structures, namely the medial canthal ligament; and inappropriate manipulation may force excessive tissue removal. Overcorrection may result in a vertical tissue deficiency of epicanthal fold and insufficient soft tissue within the medial epicanthal area. As a consequence of such tissue deficiency, the medial epicanthal angle becomes flat or concave, and the lacrimal lake may be overexposed. Scar contracture may also cause a rectangular-shaped medial canthus with overexposure of lacrimal caruncle, resulting in an unnatural appearance. Although the harmony of the overall face should be taken into account during the surgery, especially in Asian blepharoplasty, excessive horizontal lengthening may change the expression of the eyes to “angry,” leading to an unpleasing outcome. 3D reconstruction is needed to improve these situations. Asymmetric medial commissures, scarring, loss of pretarsal fullness, visible sclerae, and chronic chemosis may also be problematic in this setting. To our knowledge, only a limited number of articles have discussed the restoration technique for complicated epicanthus despite the fact that the need for further intervention is increasing.
Several surgical efforts have been made that focus on a revision technique for complicated medial canthus.18-21 Kwon et al reported a corrective epicanthoplasty technique that involved muscle and medial canthal tendon rearrangement.18 It emphasized the manipulation of muscle and tendon to avoid tissue distortion or prominent scarring. However, this method mainly targeted patients with undercorrected or relapsed epicanthal folds. In cases of overcorrected epicanthal folds, simple V-Y advancement is commonly performed, but it can only correct the ICD without consideration of the natural canthal shape.20 Shin et al also introduced a restoration technique utilizing V-Y advancement.21 An eagle beak-shaped extension was made at the medial canthal area, which created a V flap, and then V-Y advancement was utilized to restore the medial canthus. However, the nasal-side skin flap was thicker than the eyelid skin, which may have led to an unsatisfactory result.20 It also resulted in obvious scarring on the nasal side. In contrast, Chung et al employed the skin-redraping method, a standard epicanthoplasty method, to remedy overcorrected medial epicanthal folds.19,20 They performed wide dissection of the skin flap, which involved the upper and lower eyelids, to obtain sufficient tissue for new epicanthal folds. This technique can be applied to more severe cases compared with the V-Y advancement technique. It produced favorable results in terms of horizontal restoration, but there were still limitations for the restoration of the 3D canthal shape. Moreover, cases with severe skin deficiencies have a high chance of recurrence.
Z-epicanthoplasty is one of the popular methods employed for epicanthoplasty. We reversely utilized this method to restore overcorrected medial canthus. Our reliance on the Z-plasty technique imposes no further skin excision in the course of addressing tissue inadequacy and severe scar with contracture. The results were satisfactory regardless of the severity. There are salient features of this revision medial epicanthoplasty procedure that deserve emphasis. First, it improves existing scars and restores the medial canthus 3-dimensionally. Hypertrophic and especially depressed or stepped scars are all readily amenable to correction. Conventional surgery enables 2-dimensional reconstruction of planar surfaces without revising vertical planes, but by rotating the flap that we describe and turning it upside down, a web is formed to restore 3D space and improve these types of scars. Pretarsal fullness can be also regained by releasing the scar at medial canthal area, and vertical deficiency is resolved. Another advantage is the flexibility afforded in restoring desired medial canthal angles. By adjusting the flap angle at the time of design, canthal shape is recreated, altering the contours of in-fold and out-fold lines. An overexposed lacrimal lake is also improved to a given extent. This is especially important if patients cannot close their eyes or are plagued by episodic congestion due to past surgeries. Finally, our method helps restore the balance in eye shape for patients with ectropion or scleral show, particularly if the mucous membrane is exposed after concurrent medial and lateral epicanthoplasties. The latter often leads to incomplete eye closure and subsequent side effects, such as redness or epiphora. It may also be accompanied by round and flat medial canthus. Damage of canthal ligaments may be the cause of such conditions. Aside from skin restoration, damaged ligaments and muscles may be repaired in the course of our procedure as well. This is also helpful in avoiding recurrence.
Our study nevertheless has several limitations. First of all, we could not compare the outcomes with the initial appearances because we lack the photographs before any surgery. Most of the patients first visited the clinic for revisional epicanthoplasty. Second, we also could not compare our technique with other surgical methods for revisional epicanthoplasty. Third, many patients underwent other eyelid procedures simultaneously, which excluded them from outcome assessment. Lastly, we did not have the detailed measurement of ICDs or OCDs owing to our retrospective study design. Further study is needed to conduct an exact evaluation of the distances regarding indications and outcomes.
Conclusions
Our revision of medial epicanthoplasty utilizing reverse Z-plasty technique may effectively improve previously scarred or exposed lacrimal lakes and address scleral show or ectropion. It also serves to restore the medial canthal angle 3-dimensionally through horizontal skin and soft tissue restructuring, compensating for tissue loss (ie, depressions) and allowing realignment of the muscle or tendon. It is simple in design, easy to perform, and satisfactory results were achieved, conferring natural aesthetics to the medial canthal region and harmonizing with the Asian face.
Acknowledgments
The authors would like to express sincere gratitude to Joseph Kyu-hyung Park for assisting with language editing.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
Author notes
Dr Park is a plastic surgeon in private practice in Seoul, Korea



