-
PDF
- Split View
-
Views
-
Cite
Cite
Shayan Dasdar, Nika Kianfar, Mohammad Sadeghi, Babak Saedi, The Impact of Facial Asymmetry on the Surgical Outcome of Crooked Nose: A Case Control Study, Aesthetic Surgery Journal, Volume 41, Issue 6, June 2021, Pages NP284–NP294, https://doi.org/10.1093/asj/sjaa405
Close - Share Icon Share
Abstract
Facial asymmetry is considered a reason for patient dissatisfaction with the outcome of rhinoplasty.
The aim of this study was to evaluate the impact of facial asymmetry on patient postoperative satisfaction with crooked nose and to investigate the relationship between visual perception of asymmetry and anthropometric measurements.
In this retrospective study, 61 rhinoplasty patients with crooked noses were assessed. Utilizing frontal view photos, pre- and postoperative nasal deviation angles were calculated. The patients were divided into 2 groups based on the visual presence of facial asymmetry. Moreover, anthropometric characteristics of the face were evaluated utilizing facial soft tissue landmarks. Patient satisfaction with surgery outcomes, including both aesthetic and functional aspects, was assessed employing the Persian version of the Standardized Cosmesis and Health Nasal Outcomes Survey.
Based on the observations, 19 (30.2%) and 44 (69.8%) patients had I-type and C-type noses, respectively. In both groups, the deviation angle decreased significantly postoperatively (P < 0.001). Regarding the subjective evaluation of facial asymmetry, 22 (34.9%) and 41 (65.1%) cases had symmetric and asymmetric faces, respectively. Anthropometric measurements were also consistent with visual assessments of asymmetry. Satisfaction scores were significantly higher after surgery in all patients; however, there was no significant difference in the mean aesthetic improvement between symmetric (15.83 ± 2.68) and asymmetric faces (15.23 ± 4.46) (P = 0.531). The power of study was 97.8%.
Rhinoplasty in patients with deviated noses and asymmetric faces may have comparable results with symmetric ones.

Rhinoplasty is among the most commonly performed procedures in cosmetic and functional operations.1 The surgical outcome of rhinoplasty as an elective plastic procedure largely depends on subjective criteria.2 This indicates a reason for patient dissatisfaction despite the successful nasal correction. Among different types of noses, patients with crooked noses require special attention for a better outcome.3,4
Any deviation of the nasal pyramid from the vertical midline plane of the face is defined as “crooked nose.” The nose, as a central component of the face, plays an important role in the overall facial aesthetic and harmony.5 Therefore, it is not surprising that even a slight nasal deviation would have a great negative effect on the perception of attractiveness.6-8 Nasal deviation can be divided into 3 subgroups: linear (I-shaped), C-shaped, and S-shaped. In the linear type, the nasal tip and dorsum are shifted to the same side of the vertical midline of the face. In a C-shaped nose, the contour is concave on one side and convex on the other side.9,10
A crooked nose causes both functional and aesthetic problems, making rhinoplasty one of the most difficult and unpredictable plastic operations.11 Moreover, this cosmetic procedure has a lower rate of satisfaction compared with others.12 It is suggested that a major cause of patient dissatisfaction is their unrealistic perception.13 Patients mostly complain about residual nose deviation while they are unaware of the underlying facial asymmetry.7,14 Facial symmetry refers to the similarity between homologous elements of the face. The symmetry of facial components is considered as a determinant of attractiveness.15,16
This study was conducted to expand previous findings and to evaluate the possible impact of inherent facial asymmetries on the postoperative outcome. Moreover, this study investigated the accuracy of subjective visual assessment for detecting pre-existing facial asymmetry. Thereafter, its correlation with anthropometric measurements was evaluated.
METHODS
Patients and Study Design
This cohort study was performed in the facial plastic clinic of the otolaryngology department of a tertiary referral center. Sixty-three patients who had deviated noses and were scheduled for septorhinoplasty between April 2015 and November 2019 were enrolled in this study. The exclusion criteria (which may affect the final results) were as follows: revision rhinoplasty, presence of congenital malformation, need for other rhinology procedures, uncontrolled systemic diseases, major psychologic problems, and age younger than 18 years. Moreover, due to the low prevalence and complexity of angle measurement of S-type noses, patients with this type of nose were also excluded.
The patients were divided into 2 groups. The first group included patients with symmetric faces (group A) and the second group included patients with asymmetric faces (group B). Moreover, according to the shape of crookedness, each group was divided into 2 subgroups: I-type and C-type nose. This classification is determined according to the position of the bony pyramid and cartilaginous vault relative to each other. In I-type noses, the bony pyramid and cartilaginous dorsum are tilted to the same direction, whereas in C-type noses, the bony pyramid and cartilaginous dorsum are tilted to opposite directions.
Ethical Approval
The protocol of this study was approved by the institutional review board of Tehran University of Medical Sciences. Detailed information about the study was given to the participants, and written informed consent was obtained from each one.
Test and Variable Measurement
The demographic characteristics of all patients were documented. A complete physical examination was performed by the senior authors, and positive findings were collected in predesigned questionnaires. The thickness of the skin was examined and classified as thin, normal, and thick employing the Obagy skin pinch test.17
All participants had standard preoperative photos (6 views) taken with a Nikon DSLR camera (D80, Nikon, Melville, NY) utilizing a 70-mm macro lens (105-mm effective focal length). The frontal (anterior) images were taken in the Frankfurt horizontal plane. A constant point (a small 1-cm paper ruler) was utilized to match the size of the patients’ photos. The patients were followed up for 1 year, and the same standard pictures were obtained for comparison (detailed below). The analysis on images was performed employing measurements tools in Adobe Photoshop CS3 (Adobe Systems Inc., San Jose, CA).
Assessment of Facial Asymmetry
In the first part of the current study, any relationship between visual perception of asymmetry and anthropometric measurements was investigated.
For subjective evaluation of facial asymmetry, frontal view images were divided into 3 units (upper, middle, and lower) by one of the authors (S.D.). The units were evaluated for facial asymmetry by 3 blinded authors. Each photograph was shown for 5 seconds, and an interval of 3 seconds was given to the authors to express their opinion. Asymmetry was defined as any discrepancy between 2 sides of a unit based on a subjective point of view. A unit was considered asymmetric if 2 out of 3 authors considered it so. The whole face perception of symmetry was due to symmetry of all units (Figure 1).
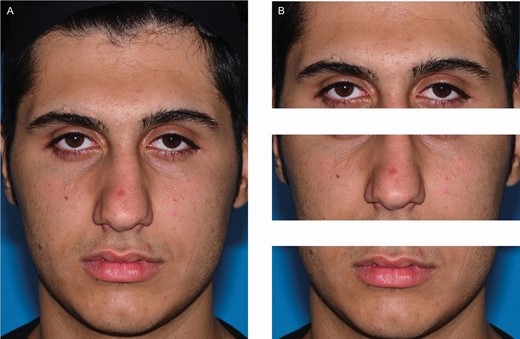
Subjective assessment of facial asymmetry. (A) Preoperative image of this 21-year-old male patient. (B) The image was divided into 3 units. Authors’ opinions about asymmetry of each unit were noted subsequently.
Anthropometric characteristics of the face were employed for objective assessment of facial asymmetry. Soft tissue landmarks of the face, including the lateral canthus, alar margin, tragus, oral commissure, cupid’s bow (Cu), and the most prominent point of the chin, were marked by 1 author (N.K.). Anthropometric measurements started with determination of a reference midline, a sagittal midline plane toward the glabella. Then, the distance between each landmark and the reference line was measured as shown in Figure 2A. The measured values were converted to a ratio by dividing the smaller amount by the larger one. Moreover, the angle between the reference line and the line passing through each central landmark (Cu and chin) and glabella was measured for assessing the axial deviation of the face (Figure 2B). Perfect values indicating facial symmetry were ratio = 1 and angle = 0°.
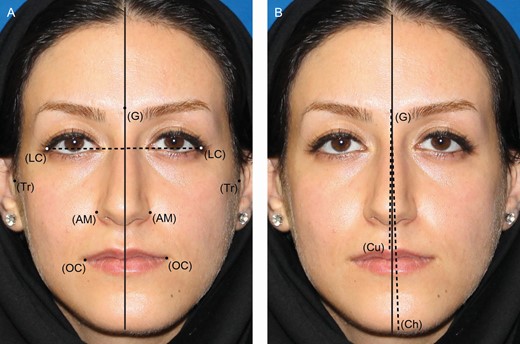
Objective assessment of facial asymmetry. Soft tissue landmarks for anthropometric measurements of this 36-year-old female: glabella (G), lateral canthus (LC), alar margin (AM), tragus (Tr), oral commissure (OC), cupid’s bow (Cu), and the most prominent point of chin (Ch). (A) Measuring distance between landmarks and reference line. (B) Measuring axial deviation of face.
Evaluation of Rhinoplasty Outcome
In the second part, 2 methods were adopted to investigate the outcome of rhinoplasty surgery.
The first method was evaluation of the nasal deviation angle. In I-type noses, a line lying between the nasion (N) and the tip of nose (T) was employed, which represented the nasal dorsal axis and consisted of both osseous and cartilaginous parts (Figure 3). The angle between the NT line and the reference midline was measured as the I-type deviation angle. The ideal angular value for I-type noses was considered 0°. Two lines were utilized in C-type noses. The first one was drawn from the N to the most prominent point of convexity defining the nasal bony axis. The second one representing the cartilaginous axis was drawn between the most prominent point and the T (Figure 4). For accurate assessment, 2 angles were measured in C-type noses: the fracture angle between the NC and CT lines, and the deviation angle between the NC line and the reference midline. In C-type noses, the perfect values for deviation angle and fracture angle were 0° and 180°, respectively.

Nose deviation angle measurement for I-type noses: glabella (G), nasion (N), and tip of nose (T). (A) Preoperative image of this 28-year-old female. (B) Measuring the angle between the NT line and reference line.
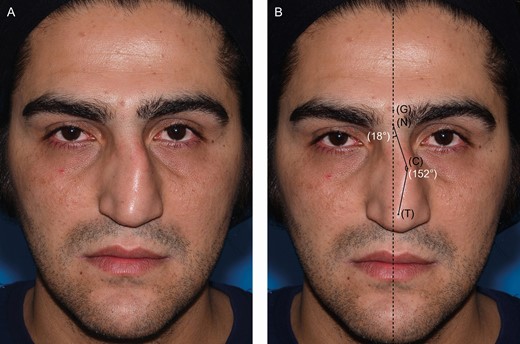
Nose deviation angle measurement for C-type noses: glabella (G), nasion (N), prominent point of convexity (C), and tip of nose (T). (A) Preoperative image of this 37-year-old male. (B) Measuring the angle between the NC line and reference line, and the angle between NC line and CT line.
The second method was assessment of the patient’s satisfaction with the surgery outcome. The severity of nasal obstruction, the level of aesthetic satisfaction, and social acceptance were measured utilizing a validated Persian version of the Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS).18,19 The questionnaire contains 10 items in 2 main domains: obstruction (questions 1-4) and cosmesis (questions 5-10). The patients answered the questions on a 0 to 5 Likert scale, with the highest score indicating the least satisfaction before and after the surgery (at least 1 year after surgery). Two authors (S.D., N.K.) explained the details of the questionnaire to the participants and completed them individually and anonymously. A blank copy of the questionnaire is provided in the Appendix.
Type of Procedure and Medical Treatment
The authors utilized an external incision rhinoplasty approach. All procedures were performed under general anesthesia by one of the senior authors. After complete skeletonization of the tip and dorsal area, the medial crura were detached from each other and the nasal septum was approached from this part. Subsequently, a bilateral sub-mucoperichondrial flap was dissected, and the upper lateral cartilage was detached from the septum. If routine septoplasty, which was performed in all cases, was inadequate, modified extracorporeal septoplasty was conducted.20
Reconstruction of the anterior or dorsal resected parts was performed utilizing septal grafts. Upper lateral spreader flaps were employed for all cases if possible.21 Moreover, if there was still any remaining dorsal deviation, the spreader graft was employed unilaterally or bilaterally. Additionally, internal lateral and medial osteotomy was performed in all cases and intermediate osteotomy in selected ones. The tongue-in-groove technique was employed in all cases for reconstruction of tip position in the middle part and to achieve the desired rotation and projection.4 No packing was applied. Furthermore, 8 mg dexamethasone was administered during the surgery, and antibiotic prophylaxis (cephalexin 500 mg/QID for 5 days) was given to all patients. The only prescribed analgesic was acetaminophen. Subsequently, internal and external nasal splints were removed after 7 days, but taping continued for 2 weeks thereafter.
Statistical Analysis
Data were analyzed with SPSS 21 for Windows (SPSS Inc., Chicago, IL). Measurements are reported as absolute number and percentage for categorical variables and mean ± standard deviation (SD) for quantitative variables. Normal distribution of the data was evaluated employing the 1-Sample Kolmogorov-Smirnov test. Pearson’s chi-square was utilized to compare proportions. Independent-sample t test (for variables with a normal distribution) and Mann-Whitney U test (for variables without a normal distribution) were employed to assess differences between groups. Changes in the facial measurements and patient satisfaction score of the SCHNOS questionnaire after rhinoplasty were compared utilizing paired t test (for variables with a normal distribution) and Wilcoxon test (for variables without a normal distribution). Statistical significance was defined as P < 0.05.
RESULTS
Patients’ Demographic Data
Sixty-three patients who met the inclusion criteria were enrolled in the study, of whom 28 (44.4%) were male and 35 (55.6%) were female with a female to male ratio of 1.25:1. The mean age of the patients at the time of operation was 32.9 years (range, 20-50 years). The skin thickness was normal in 38 (60.3%), thick in 21 (33.3%), and thin in 4 (6.3%) cases.
Assessment of Pre- and Postoperative Nasal Angles
Nineteen (30.2%) patients had I-type and 44 (69.8%) patients had C-type noses. In patients with I-type noses, the mean deviation angle changed from 4.3° preoperatively (range: 1.0°-8.6°) to 1.8° postoperatively (range: 0.0°-4.7°) (P < 0.001). The mean preoperative fracture angle and deviation angle of the patients with C-type nose were 168.8° (range: 148.8°-177.8°) and 7.6° (range: 1.6°-19.7°), respectively. In this group, the mean fracture angle changed to 178.0° (range: 168.9°-189.5°) (P < 0.001) and the mean deviation angle changed to 3.1° (range: 0.0°-8.1°) (P < 0.001) postoperatively. The mean ala ratio was 0.88 preoperatively (SD = 0.08) and 0.92 (SD = 0.06) postoperatively (P = 0.006).
Assessment of Facial Asymmetry
Regarding the visual perception of the facial units, the asymmetry rate in the lower unit was 41.3% (26 patients) followed by 36.5% (23 patients) and 34.9% (22 patients) in mid and upper units, respectively. Moreover, 38% (24 patients) of the patients had mixed type asymmetry (asymmetry in more than 1 unit). Regarding the relationship between direction of the nasal deviation and facial width, it was found that the direction of nasal deviation was toward the short side of the face in 55.5% of the patients (n = 35) and opposite to the short side of the face in 45.5% of the patients (n = 28) (Table 1).
| Variable . | Short side of face . | . |
|---|---|---|
| . | Left (n = 35) . | Right (n = 28) . |
| Nasal deviation, No. (%) | ||
| Left | 20 (57.1%) | 13 (46.4%) |
| Right | 15 (42.9%) | 15 (53.6%) |
| Variable . | Short side of face . | . |
|---|---|---|
| . | Left (n = 35) . | Right (n = 28) . |
| Nasal deviation, No. (%) | ||
| Left | 20 (57.1%) | 13 (46.4%) |
| Right | 15 (42.9%) | 15 (53.6%) |
| Variable . | Short side of face . | . |
|---|---|---|
| . | Left (n = 35) . | Right (n = 28) . |
| Nasal deviation, No. (%) | ||
| Left | 20 (57.1%) | 13 (46.4%) |
| Right | 15 (42.9%) | 15 (53.6%) |
| Variable . | Short side of face . | . |
|---|---|---|
| . | Left (n = 35) . | Right (n = 28) . |
| Nasal deviation, No. (%) | ||
| Left | 20 (57.1%) | 13 (46.4%) |
| Right | 15 (42.9%) | 15 (53.6%) |
In 22 patients (34.9%), the whole face was considered as a symmetric face with respect to lack of asymmetry in any of the units. A perfect value of ratio for all facial landmarks (ratio = 1) was not detected in any of the patients. Therefore, all of our patients had some degree of asymmetry in anthropometric measurements. The dot plots of each anthropometric landmark ratio regarding the asymmetry perception of its related unit (lateral canthus for upper unit, tragus for mid unit, oral commissure for lower unit) are demonstrated in Figure 5.
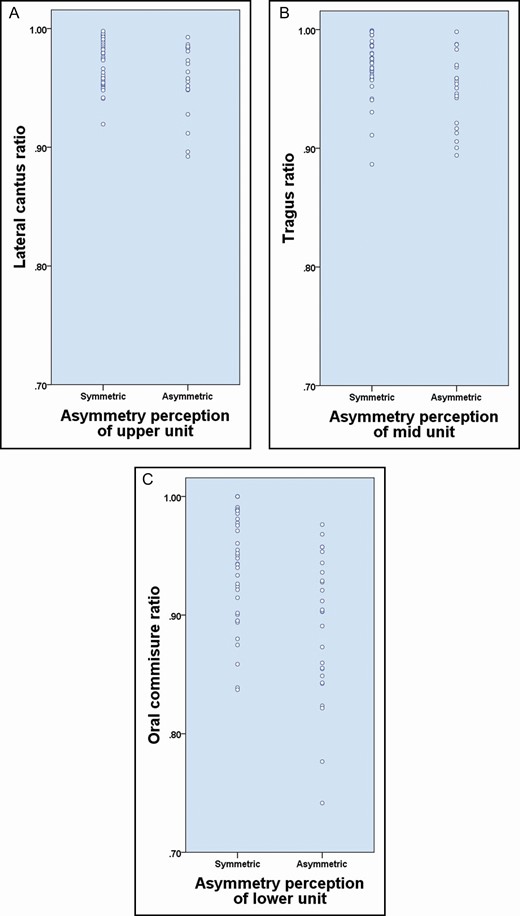
The anthropometric landmark ratio in each unit based on asymmetry perception. (A) Lateral cantus for upper unit, (B) Tragus for mid unit, (C) Oral commissure for lower unit.
The mean ratio of each anthropometric landmark according to the visual perception of asymmetry in each unit and the mean angle of central landmarks according to the whole face asymmetry are shown in Table 2. Regarding the measurements in each subunit, the mean ratios were significantly lower in asymmetric perceived subunits. In the whole face assessment, only the deviation of the line between glabella (G) and cupid’s bow (Cu) reached a level of significance (P = 0.042).
| Facial unit . | Facial asymmetry, No (%) . | . | Anthropometric measurement . | Mean ± SD . | P value . |
|---|---|---|---|---|---|
| Upper | Sym | 41 (65.1%) | RML-LC | 0.97 ± 0.02 | 0.041a |
| Asym | 22 (34.9%) | 0.96 ± 0.03 | |||
| Mid | Sym | 40 (63.5%) | RML-Tr | 0.97 ± 0.02 | 0.006a |
| Asym | 23 (36.5%) | 0.95 ± 0.03 | |||
| Lower | Sym | 37 (58.7%) | RML-OC | 0.94 ± 0.05 | <0.001a |
| Asym | 26 (41.3%) | 0.89 ± 0.06 | |||
| Whole face | Sym | 22 (34.9%) | AML-CuG,° | 0.53 ± 0.39 | 0.042a |
| Asym | 41 (65.1%) | 0.85 ± 0.66 | |||
| Sym | 22 (34.9%) | AML-ChG,° | 0.43 ± 0.24 | 0.165b | |
| Asym | 41 (65.1%) | 0.71 ± 0.61 |
| Facial unit . | Facial asymmetry, No (%) . | . | Anthropometric measurement . | Mean ± SD . | P value . |
|---|---|---|---|---|---|
| Upper | Sym | 41 (65.1%) | RML-LC | 0.97 ± 0.02 | 0.041a |
| Asym | 22 (34.9%) | 0.96 ± 0.03 | |||
| Mid | Sym | 40 (63.5%) | RML-Tr | 0.97 ± 0.02 | 0.006a |
| Asym | 23 (36.5%) | 0.95 ± 0.03 | |||
| Lower | Sym | 37 (58.7%) | RML-OC | 0.94 ± 0.05 | <0.001a |
| Asym | 26 (41.3%) | 0.89 ± 0.06 | |||
| Whole face | Sym | 22 (34.9%) | AML-CuG,° | 0.53 ± 0.39 | 0.042a |
| Asym | 41 (65.1%) | 0.85 ± 0.66 | |||
| Sym | 22 (34.9%) | AML-ChG,° | 0.43 ± 0.24 | 0.165b | |
| Asym | 41 (65.1%) | 0.71 ± 0.61 |
AML-ChG, angle of midline and the line through glabella to chin; AML-CuG, angle between midline and the line through glabella to cupid’s bow; Asym, asymmetric; RML-LC, midline to lateral cantus ratio; RML-OC, midline to oral commissure ratio; RML-Tr, midline to tragus ratio; Sym, symmetric. aBased on independent-sample t test. bBased on Mann-Whitney U test.
| Facial unit . | Facial asymmetry, No (%) . | . | Anthropometric measurement . | Mean ± SD . | P value . |
|---|---|---|---|---|---|
| Upper | Sym | 41 (65.1%) | RML-LC | 0.97 ± 0.02 | 0.041a |
| Asym | 22 (34.9%) | 0.96 ± 0.03 | |||
| Mid | Sym | 40 (63.5%) | RML-Tr | 0.97 ± 0.02 | 0.006a |
| Asym | 23 (36.5%) | 0.95 ± 0.03 | |||
| Lower | Sym | 37 (58.7%) | RML-OC | 0.94 ± 0.05 | <0.001a |
| Asym | 26 (41.3%) | 0.89 ± 0.06 | |||
| Whole face | Sym | 22 (34.9%) | AML-CuG,° | 0.53 ± 0.39 | 0.042a |
| Asym | 41 (65.1%) | 0.85 ± 0.66 | |||
| Sym | 22 (34.9%) | AML-ChG,° | 0.43 ± 0.24 | 0.165b | |
| Asym | 41 (65.1%) | 0.71 ± 0.61 |
| Facial unit . | Facial asymmetry, No (%) . | . | Anthropometric measurement . | Mean ± SD . | P value . |
|---|---|---|---|---|---|
| Upper | Sym | 41 (65.1%) | RML-LC | 0.97 ± 0.02 | 0.041a |
| Asym | 22 (34.9%) | 0.96 ± 0.03 | |||
| Mid | Sym | 40 (63.5%) | RML-Tr | 0.97 ± 0.02 | 0.006a |
| Asym | 23 (36.5%) | 0.95 ± 0.03 | |||
| Lower | Sym | 37 (58.7%) | RML-OC | 0.94 ± 0.05 | <0.001a |
| Asym | 26 (41.3%) | 0.89 ± 0.06 | |||
| Whole face | Sym | 22 (34.9%) | AML-CuG,° | 0.53 ± 0.39 | 0.042a |
| Asym | 41 (65.1%) | 0.85 ± 0.66 | |||
| Sym | 22 (34.9%) | AML-ChG,° | 0.43 ± 0.24 | 0.165b | |
| Asym | 41 (65.1%) | 0.71 ± 0.61 |
AML-ChG, angle of midline and the line through glabella to chin; AML-CuG, angle between midline and the line through glabella to cupid’s bow; Asym, asymmetric; RML-LC, midline to lateral cantus ratio; RML-OC, midline to oral commissure ratio; RML-Tr, midline to tragus ratio; Sym, symmetric. aBased on independent-sample t test. bBased on Mann-Whitney U test.
No differences were found in sex, age, skin thickness, deviation type, or pre- and postoperative nasal angles between patients with symmetric and asymmetric faces (Table 3). Therefore, the characteristics and nasal angle correction were similar in both groups to assess the possible effect of facial asymmetry on the patient satisfaction score.
Demographic Data and Nose Measurements of Patients With Symmetric and Asymmetric Faces
| Variables . | . | Facial asymmetry perception . | . | . |
|---|---|---|---|---|
| . | . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Sex, No. (%) | Male | 12 (54.5%) | 16 (39%) | 0.237a |
| Female | 10 (45.5%) | 25 (61%) | ||
| Age at surgery, y (mean ± SD) | 33.61 ± 8.01 | 32.60 ± 6.94 | 0.627b | |
| Skin thickness, No. (%) | Thin | 1 (4.5%) | 3 (7.3%) | 0.418a |
| Normal | 15 (68.2%) | 23 (56.1%) | ||
| Thick | 6 (27.3%) | 15 (36.6%) | ||
| C-type nose, No. (%) | 17 (77.3%) | 27 (65.9%) | 0.215b | |
| Preoperative nasal angle, ° (mean ± SD) | Fracture angle | 167.11 ± 6.11 | 169.92 ± 6.26 | 0.151b |
| Deviation angle | 8.85 ± 3.95 | 6.85 ± 4.15 | 0.120b | |
| Postoperative nasal angle, ° (mean ± SD) | Fracture angle | 177.49 ± 5.01 | 178.50 ± 3.12 | 0.414c |
| Deviation angle | 3.55 ± 2.39 | 2.81 ± 1.84 | 0.252b | |
| I-type nose, No. (%) | 5 (22.7%) | 14 (34.1%) | — | |
| Preoperative nasal angle, ° (mean ± SD) | Deviation angle | 4.38 ± 1.83 | 4.23 ± 2.16 | 0.896b |
| Postoperative nasal angle, ° (mean ± SD) | Deviation angle | 1.26 ± 1.15 | 2.01 ± 1.38 | 0.292b |
| Ala ratio, preoperative, (mean ± SD) | 0.89 ± 0.06 | 0.88 ± 0.08 | 0.342b | |
| Ala ratio, postoperative, (mean ± SD) | 0.93 ± 0.06 | 0.92 ± 0.06 | 0.282b |
| Variables . | . | Facial asymmetry perception . | . | . |
|---|---|---|---|---|
| . | . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Sex, No. (%) | Male | 12 (54.5%) | 16 (39%) | 0.237a |
| Female | 10 (45.5%) | 25 (61%) | ||
| Age at surgery, y (mean ± SD) | 33.61 ± 8.01 | 32.60 ± 6.94 | 0.627b | |
| Skin thickness, No. (%) | Thin | 1 (4.5%) | 3 (7.3%) | 0.418a |
| Normal | 15 (68.2%) | 23 (56.1%) | ||
| Thick | 6 (27.3%) | 15 (36.6%) | ||
| C-type nose, No. (%) | 17 (77.3%) | 27 (65.9%) | 0.215b | |
| Preoperative nasal angle, ° (mean ± SD) | Fracture angle | 167.11 ± 6.11 | 169.92 ± 6.26 | 0.151b |
| Deviation angle | 8.85 ± 3.95 | 6.85 ± 4.15 | 0.120b | |
| Postoperative nasal angle, ° (mean ± SD) | Fracture angle | 177.49 ± 5.01 | 178.50 ± 3.12 | 0.414c |
| Deviation angle | 3.55 ± 2.39 | 2.81 ± 1.84 | 0.252b | |
| I-type nose, No. (%) | 5 (22.7%) | 14 (34.1%) | — | |
| Preoperative nasal angle, ° (mean ± SD) | Deviation angle | 4.38 ± 1.83 | 4.23 ± 2.16 | 0.896b |
| Postoperative nasal angle, ° (mean ± SD) | Deviation angle | 1.26 ± 1.15 | 2.01 ± 1.38 | 0.292b |
| Ala ratio, preoperative, (mean ± SD) | 0.89 ± 0.06 | 0.88 ± 0.08 | 0.342b | |
| Ala ratio, postoperative, (mean ± SD) | 0.93 ± 0.06 | 0.92 ± 0.06 | 0.282b |
SD, standard deviation. aBased on χ 2 test. bBased on independent-sample t test. cBased on Mann-Whitney U test.
Demographic Data and Nose Measurements of Patients With Symmetric and Asymmetric Faces
| Variables . | . | Facial asymmetry perception . | . | . |
|---|---|---|---|---|
| . | . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Sex, No. (%) | Male | 12 (54.5%) | 16 (39%) | 0.237a |
| Female | 10 (45.5%) | 25 (61%) | ||
| Age at surgery, y (mean ± SD) | 33.61 ± 8.01 | 32.60 ± 6.94 | 0.627b | |
| Skin thickness, No. (%) | Thin | 1 (4.5%) | 3 (7.3%) | 0.418a |
| Normal | 15 (68.2%) | 23 (56.1%) | ||
| Thick | 6 (27.3%) | 15 (36.6%) | ||
| C-type nose, No. (%) | 17 (77.3%) | 27 (65.9%) | 0.215b | |
| Preoperative nasal angle, ° (mean ± SD) | Fracture angle | 167.11 ± 6.11 | 169.92 ± 6.26 | 0.151b |
| Deviation angle | 8.85 ± 3.95 | 6.85 ± 4.15 | 0.120b | |
| Postoperative nasal angle, ° (mean ± SD) | Fracture angle | 177.49 ± 5.01 | 178.50 ± 3.12 | 0.414c |
| Deviation angle | 3.55 ± 2.39 | 2.81 ± 1.84 | 0.252b | |
| I-type nose, No. (%) | 5 (22.7%) | 14 (34.1%) | — | |
| Preoperative nasal angle, ° (mean ± SD) | Deviation angle | 4.38 ± 1.83 | 4.23 ± 2.16 | 0.896b |
| Postoperative nasal angle, ° (mean ± SD) | Deviation angle | 1.26 ± 1.15 | 2.01 ± 1.38 | 0.292b |
| Ala ratio, preoperative, (mean ± SD) | 0.89 ± 0.06 | 0.88 ± 0.08 | 0.342b | |
| Ala ratio, postoperative, (mean ± SD) | 0.93 ± 0.06 | 0.92 ± 0.06 | 0.282b |
| Variables . | . | Facial asymmetry perception . | . | . |
|---|---|---|---|---|
| . | . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Sex, No. (%) | Male | 12 (54.5%) | 16 (39%) | 0.237a |
| Female | 10 (45.5%) | 25 (61%) | ||
| Age at surgery, y (mean ± SD) | 33.61 ± 8.01 | 32.60 ± 6.94 | 0.627b | |
| Skin thickness, No. (%) | Thin | 1 (4.5%) | 3 (7.3%) | 0.418a |
| Normal | 15 (68.2%) | 23 (56.1%) | ||
| Thick | 6 (27.3%) | 15 (36.6%) | ||
| C-type nose, No. (%) | 17 (77.3%) | 27 (65.9%) | 0.215b | |
| Preoperative nasal angle, ° (mean ± SD) | Fracture angle | 167.11 ± 6.11 | 169.92 ± 6.26 | 0.151b |
| Deviation angle | 8.85 ± 3.95 | 6.85 ± 4.15 | 0.120b | |
| Postoperative nasal angle, ° (mean ± SD) | Fracture angle | 177.49 ± 5.01 | 178.50 ± 3.12 | 0.414c |
| Deviation angle | 3.55 ± 2.39 | 2.81 ± 1.84 | 0.252b | |
| I-type nose, No. (%) | 5 (22.7%) | 14 (34.1%) | — | |
| Preoperative nasal angle, ° (mean ± SD) | Deviation angle | 4.38 ± 1.83 | 4.23 ± 2.16 | 0.896b |
| Postoperative nasal angle, ° (mean ± SD) | Deviation angle | 1.26 ± 1.15 | 2.01 ± 1.38 | 0.292b |
| Ala ratio, preoperative, (mean ± SD) | 0.89 ± 0.06 | 0.88 ± 0.08 | 0.342b | |
| Ala ratio, postoperative, (mean ± SD) | 0.93 ± 0.06 | 0.92 ± 0.06 | 0.282b |
SD, standard deviation. aBased on χ 2 test. bBased on independent-sample t test. cBased on Mann-Whitney U test.
Assessment of Pre- and Postoperative Patient Satisfaction
Postoperative SCHNOS scores were higher than preoperative scores for all the patients. The mean preoperative score was 35.82 (SD = 4.31), which increased to 10.67 (SD = 6.06) after the operation. The mean difference between the pre- and postoperative satisfaction scores (the improvement in satisfaction scores) was 25.16 (SD = 6.31) (P ≤ 0.001). No significant relationship was found between satisfaction score improvement and demographic characteristics, including age, sex, and skin thickness. There was no significant difference in satisfaction score based on laterality of the face/nose structures deviation. Additionally, the correlation between satisfaction score improvement and deviation angle correction was not significant (Figure 6). Assessment of the patient satisfaction score based on asymmetry perception of the face showed no significant difference. Table 4 compares the aesthetic, functional, and total improvement scores of patients within symmetric and asymmetric face groups. The power of study was 97.8%.
Comparison of Patients’ Satisfaction Score Within Symmetric and Asymmetric Face Groups
| Variables . | Facial asymmetry perception . | . | . |
|---|---|---|---|
| . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Functional improvement scorea (mean ± SD) | 10.00 ± 3.43 | 9.62 ± 4.11 | 0.731d |
| Aesthetic improvement scoreb (mean ± SD) | 15.83 ± 2.68 | 15.23 ± 4.46 | 0.531d |
| Total improvement scorec (mean ± SD) | 25.83 ± 3.98 | 24.85 ± 7.15 | 0.508d |
| Variables . | Facial asymmetry perception . | . | . |
|---|---|---|---|
| . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Functional improvement scorea (mean ± SD) | 10.00 ± 3.43 | 9.62 ± 4.11 | 0.731d |
| Aesthetic improvement scoreb (mean ± SD) | 15.83 ± 2.68 | 15.23 ± 4.46 | 0.531d |
| Total improvement scorec (mean ± SD) | 25.83 ± 3.98 | 24.85 ± 7.15 | 0.508d |
SD, standard deviation. aThe difference of pre- and postoperative functional satisfaction score. bThe difference of pre- and postoperative aesthetic satisfaction score. cThe difference of pre- and postoperative total satisfaction score. dBased on independent-sample t test.
Comparison of Patients’ Satisfaction Score Within Symmetric and Asymmetric Face Groups
| Variables . | Facial asymmetry perception . | . | . |
|---|---|---|---|
| . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Functional improvement scorea (mean ± SD) | 10.00 ± 3.43 | 9.62 ± 4.11 | 0.731d |
| Aesthetic improvement scoreb (mean ± SD) | 15.83 ± 2.68 | 15.23 ± 4.46 | 0.531d |
| Total improvement scorec (mean ± SD) | 25.83 ± 3.98 | 24.85 ± 7.15 | 0.508d |
| Variables . | Facial asymmetry perception . | . | . |
|---|---|---|---|
| . | Symmetric (n = 22) . | Asymmetric (n = 41) . | P value . |
| Functional improvement scorea (mean ± SD) | 10.00 ± 3.43 | 9.62 ± 4.11 | 0.731d |
| Aesthetic improvement scoreb (mean ± SD) | 15.83 ± 2.68 | 15.23 ± 4.46 | 0.531d |
| Total improvement scorec (mean ± SD) | 25.83 ± 3.98 | 24.85 ± 7.15 | 0.508d |
SD, standard deviation. aThe difference of pre- and postoperative functional satisfaction score. bThe difference of pre- and postoperative aesthetic satisfaction score. cThe difference of pre- and postoperative total satisfaction score. dBased on independent-sample t test.
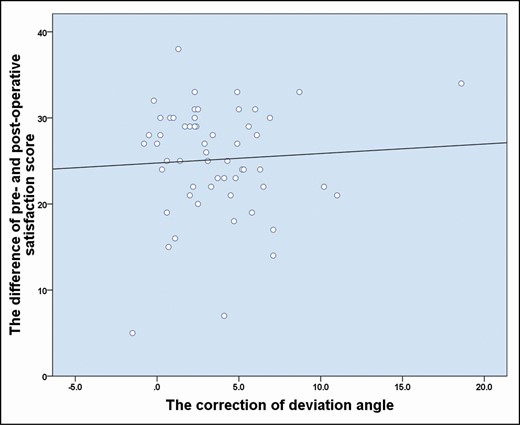
Correlation between satisfaction score improvement and deviation angle correction (difference between pre- and postoperative deviation angle).
Complications
Epistaxis occurred in 1 of the patients (1.58%) in the first week after surgery, which was controlled with endoscopy and suction cautery. In addition, synechia was detected in another patient (1.58%) during the follow-up period. Three patients (4.76%) needed revision rhinoplasty for aesthetic reasons.
DISCUSSION
Management of crooked nose is still among the most difficult challenges in rhinoplasty. Recent advances in surgical techniques have improved the results. However, concomitant facial asymmetry and its possible effect on the long-term results of surgery are yet unclear. The effect of nasal septal growth abnormality on facial growth asymmetry is a well-addressed subject. Despite the high prevalence of these abnormalities in patients with deviated noses, the possible effect of facial asymmetry on final patient satisfaction is a controversial issue. In this series of 63 patients with deviated noses, we did not find any significant differences between the functional and aesthetic outcomes of patients with and without facial asymmetry. Moreover, no significant relationship was found among other variables.
Facial asymmetry in patients with cleft nose is an important example of the effect of septal deviation on facial growth. Nasal growth can be considered a pacemaker of facial growth in the early stages of life. The same effect can also be assumed for facial asymmetry due to the development of a deviated nose.22-24 This concurrency of nasal deviation and facial asymmetry was investigated in many previous studies. Hafezi et al25 conducted a review and found that facial asymmetry was very common in patients with deviated nose. However, it was also detected in patients with straight noses. Furthermore, they carried out a study on 89 rhinoplasty patients with facial asymmetry and concluded that all of them had some degree of upper lateral asymmetry on the deviated side.26
Likewise, Carvalho et al27 found that facial asymmetry was very common in patients who sought rhinoplasty. Therefore, special attention should be paid to patient selection and surgical technique. Hartman et al28 emphasized the role of septal deformity in the development of facial asymmetry. They tried to define the relationship between more localized aspects of asymmetry and different parts of septum and found a correlation between septal deviation and facial asymmetry; however, its relationship with the site and severity of facial asymmetry was not significant.
Although a large body of literature underlies the concomitance of facial asymmetry with crooked nose, a few studies have investigated its possible effect on patient satisfaction after rhinoplasty. Abbas et al13 performed a prospective study about the social perception of asymmetry in rhinoplasty patients. They concluded that it was an important determinant of patient satisfaction after rhinoplasty and that asymmetry was more prevalent in revision cases. Baudouin et al16 evaluated female attractiveness and reported that facial symmetry was very important in attractiveness.
In the present study, visual perception and anthropometric features of the upper, mid, and lower subunits of the face were evaluated to assess facial asymmetry. In anthropometric measurements, none of the faces were truly symmetrical, whereas about one-third of the patients were subjectively classified in this group. A possible explanation for these findings may be related to variability in the observers’ perception of a symmetric face. Furthermore, visual perception of symmetry lacks the precision of anthropometric measurements in such a way that a study found a threshold of at least 3 mm triggered the conscious perception in an observer.29
Yet, as was revealed in the result section of the present study, each measurement had a significant correlation with perception of asymmetry. Thus, the surgeon’s judgment about facial asymmetry can work properly despite overlooking slight amounts of asymmetry. In the present study, 41 (65.1%) and 22 (34.9%) patients had asymmetric and symmetric faces, respectively. The results showed significant improvement in aesthetics and function of patients with deviated nose in both groups. Moreover, there was no significant difference in the mean satisfaction score between patients with symmetric and asymmetric faces despite obvious facial asymmetry in the latter group.
These findings are consistent with the results of a study by Hussein et al30 in 2015. They found that straightening of the nose, as the most noticeable part of the face, might obscure the residual facial deformity.
Although the results of the present study need to be confirmed in further studies, it seems that functional and aesthetic improvement after rhinoplasty may have a positive psychological effect, resulting in pleasant feelings in patients regardless of the underlying facial asymmetry. Similarly, Nouraie et al8 studied 100 rhinoplasty patients and reported that psychological feelings about facial asymmetry perception changed after rhinoplasty.
Moreover, in the present study, demographic characteristics of the patients, including age, sex, skin thickness, and laterality of the face/nose deviation, had no effect on patient satisfaction. Importantly, it was found that the rate of correction of nasal deviation had no significant effect on patient satisfaction.
Despite using different techniques for outcome evaluation, there are some elements of subjectivity in such studies and this study was no exception to this limitation. We tried to reduce the impact of subjectivity through employing the computer and objective analysis beside subjective assessment. Moreover, the complex condition of the deviated nose requires different specific techniques for each special case, which would result in an inconsistent series affecting the final result. Larger studies considering the participants’ psychological attitude, which may affect their perception of asymmetry, may confirm the results of the present study.
However, it is still necessary for surgeons to have realistic discussions with rhinoplasty candidates before surgery, especially those with deviated noses. Moreover, they need to discuss the presence of facial asymmetry, which is mostly unnoticeable to patients, considering that sufficient preoperative consultation explanation of all aspects of facial asymmetry can play an important role in postoperative patient satisfaction. Additionally, reasonable selection of candidates has a key role in patient satisfaction after surgery. Finally, surgeons need to improve nasal symmetry and place the nose in the center of the face between the glabella and the midline of the lip in nasal plastic surgery.7
CONCLUSIONS
Rhinoplasty in patients with deviated noses and asymmetric faces may have comparable results with patients with symmetric faces. Careful patient selection and comprehensive preoperative consultation are mandatory for postoperative satisfaction.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES



