-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan Cook, Barry E DiBernardo, Jason N Pozner, Bipolar Radiofrequency as an Adjunct to Face and Body Contouring: A 745-Patient Clinical Experience, Aesthetic Surgery Journal, Volume 41, Issue 6, June 2021, Pages 685–694, https://doi.org/10.1093/asj/sjaa417
Close - Share Icon Share
Abstract
Radiofrequency (RF) technology has ushered in a new paradigm in body contouring for patients with mild to moderate skin laxity who desire fat removal without exacerbating skin laxity issues. A bipolar internal RF device, used as an adjunct to liposuction, has been found to be simpler and more accurate than previous technologies.
The aim of this study was to review the authors’ clinical experience with bipolar RF-assisted liposuction (RFAL).
We conducted a review of our large experience with bipolar RFAL, evaluating the nuances from appropriate patient selection and specific treatment areas. The review covered 745 patients treated from January 2017 to January 2020 at 2 centers. A retrospective chart review was performed of the first and last 50 patients treated at each center (for a total of 100 patients in each group) to assess trends in outcomes and adverse events.
Results were generally excellent from physician evaluation, and overall patient satisfaction was high (96%). The two most common adverse events were temporary swelling (9%) and nodules (8.5%). Selected examples of a variety of cases are reviewed.
The ability to tighten skin with a minimally invasive tool adds much to the contemporary approach to the body-contouring patient with skin laxity. Adverse events were minimal and greatly decreased after an initial short learning curve. Bipolar RFAL is a strong addition to our surgical armamentarium and has become an essential tool for our practices.

The addition of energy devices to liposuction has evolved since ultrasound-assisted liposuction (UAL) was first introduced in the 1990s.1 Initial reports of UAL suggested better skin tightening through a suspected skin-heating mechanism than with traditional liposuction,2 but lack of temperature monitoring and difficulties with the delivery of ultrasound energy led to inconsistent results.2,3 Power-assisted liposuction (PAL) devices were subsequently introduced and allowed rapid fat removal but without skin heating and skin tightening.4,5 The technology evolved from initial UAL and PAL devices to laser-assisted liposuction (LAL), which was the first energy-based technology to include precise temperature monitoring and subsequently improve the consistency of results.6-9 Radiofrequency (RF) devices emerged as an adjunct to liposuction; these devices offered precise internal temperature monitoring and external camera temperature monitoring, and completely changed the way surgeons approach skin tightening with liposuction. Initial monopolar RF devices with external monitoring and thin probes increased the popularity of RF as a modality in the skin tightening arena.10,11
Bipolar RF-assisted liposuction (RFAL) was first introduced in 200911 but was not approved in the United States until late 2016. We have been using the latest generation of bipolar RF devices since early 2017 and have noticed an evolution in the way we approach patients and areas treated. Patients who were previously considered not ideal candidates for traditional liposuction, due to age and issues with skin laxity, could be effectively treated with this technology. A trend towards treating smaller areas under local anesthesia was also noticed as this type of anesthesia became more requested. In our clinical experience with the latest bipolar RF devices, a consistent approach for achieving high-quality results was developed by utilizing this technology in a variety of treatment areas. The mechanism of bipolar RF contouring, the bipolar device used, as well as a review of our preferred approach to using bipolar RF in a variety of situations will be discussed here. We hope this paper will serve as a guide to the use of bipolar RF, for surgeons interested in expanding liposuction in patients with mild to moderate skin laxity, both in common areas and those not routinely treated.
METHODS
All patients treated with the InMode bipolar RF system (BodyTite, FaceTite, AccuTite; InMode Corporation, Lake Forest, CA) from January 2017 through January 2020 at 2 centers (Sanctuary Plastic Surgery, Boca Raton, FL and New Jersey Plastic Surgery, Montclair, NJ) were included in this study. Patient selection was based on the clinical judgment and experience of the senior authors. Patients were excluded if they were considered poor candidates for bipolar RF, such as those with areas of hanging skin more amenable to excisional treatment. Basic demographic data were obtained for all patients. Patients undergoing retreatment of previously treated areas were excluded from this study, so that all unique treatment areas could be counted separately. A retrospective chart review was performed of the first and last 50 patients treated at each center (for a total of 100 patients in each group), in order to assess trends in outcomes and adverse events. At both centers, patient satisfaction was assessed during routine surgical follow-up and recorded for this chart review. Statistical comparisons between groups were made with Fischer’s exact test and Student’s t test, where appropriate. This study was conducted in compliance with the Declaration of Helsinki12 and all patients provided their written informed consent.
Technology
A brief overview of the InMode bipolar RF platform is helpful in order to understand its use in the present study. The initial device had a power of 20 W and had 2 bipolar applicators—a body handpiece called BodyTite (Figure 1A) and a smaller face handpiece called FaceTite (Figure 1B). The device was upgraded to 40 W within the first year and additional handpieces were introduced to take advantage of this increased power. Subsequently a smaller handpiece called AccuTite was also introduced (Figure 1C). Table 1 describes the different dimensions and properties of each handpiece. With all bipolar RF handpieces, RF energy flows between the internal and external electrodes (Figure 2). The depth of flow, or cone of energy, can be controlled via a spring mechanism on the handpiece. This variable mechanism allows for a deep flow of energy to the underlying fibrous tissue network (Figure 3) for “vertical” tightening, as well as a transdermal application of thermal energy for “horizontal” skin tightening.7
| . | Length (cm) . | Diameter (mm) . | Energy depth (cm) . |
|---|---|---|---|
| BodyTite | 17 | 2.2 | 2-6 |
| FaceTite | 10 | 1.3 | 1-2 |
| AccuTite | 6 | 0.9 | <1 |
| . | Length (cm) . | Diameter (mm) . | Energy depth (cm) . |
|---|---|---|---|
| BodyTite | 17 | 2.2 | 2-6 |
| FaceTite | 10 | 1.3 | 1-2 |
| AccuTite | 6 | 0.9 | <1 |
| . | Length (cm) . | Diameter (mm) . | Energy depth (cm) . |
|---|---|---|---|
| BodyTite | 17 | 2.2 | 2-6 |
| FaceTite | 10 | 1.3 | 1-2 |
| AccuTite | 6 | 0.9 | <1 |
| . | Length (cm) . | Diameter (mm) . | Energy depth (cm) . |
|---|---|---|---|
| BodyTite | 17 | 2.2 | 2-6 |
| FaceTite | 10 | 1.3 | 1-2 |
| AccuTite | 6 | 0.9 | <1 |
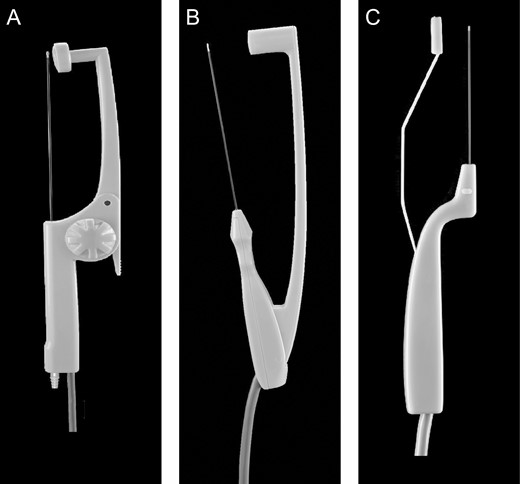
(A) BodyTite handpiece. (B) FaceTite handpiece. (C) AccuTite handpiece.
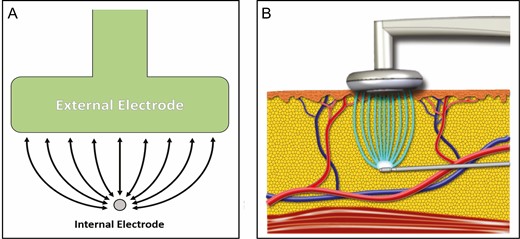
(A) Schematic depicting the flow of radiofrequency energy between the internal and external electrodes. (B) Idealized image of radiofrequency energy transfer within tissue.
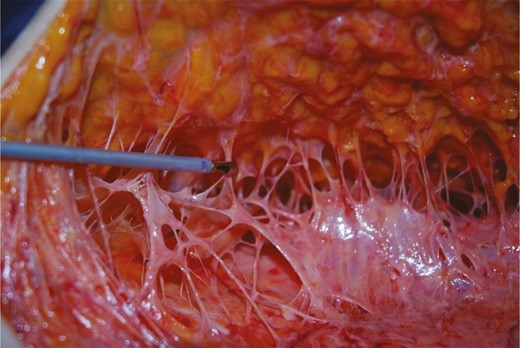
Deep fibrous tissue target for radiofrequency energy. (Reprinted with permission of Oxford University Press.16)
Technique
Tumescent fluid infiltration is performed for all areas undergoing bipolar RF treatment, both under general and local anesthesia with intravenous sedation. Our preferred tumescent fluid is 50 mL of 1% lidocaine and 1 mg epinephrine mixed into 1 L of lactated Ringer’s solution.13 Fractional volumes are prepared for smaller areas, and we increase the concentration of lidocaine for procedures performed under local or intravenous sedation. We adhere to the American Society of Plastic Surgeons guideline for maximal lidocaine during tumescent liposuction (35 mg/kg body weight),14 taking into account any additional lidocaine used for a concurrent local procedure. Small stab incisions are made with a 14-gauge needle or an 11-blade scalpel, and infiltration is performed with a 14-gauge infiltration cannula (Black & Black Surgical, Inc., Tucker, GA) until turgor of the overlying soft tissues is achieved. As has been previously noted,15,16 this subcutaneous fluid aids in RF conductivity, and the tissue turgor provides a smooth surface upon which to move the device while facilitating adequate coupling between the external and internal electrodes.
The appropriate handpiece is selected based upon treatment area. In general, the 40-W BodyTite probe is used on the abdomen, flanks, back, arms, thighs, and calves. The FaceTite probe is used selectively for narrower areas, such as the neck, “bra fat,” breast, and knees. The AccuTite probe is limited to the most superficial areas, such as the submental region in patients with “short necks,” the jowls, nasolabial folds, and other facial areas. Standard settings for both practices are a set target temperature of 42°C for the external probe and 70°C for the internal probe. Initially, it is recommended to use settings 2 to 4°C less than this during the learning period for most areas. For thinner face and neck tissues, it is common to limit the temperature to 40°C external and 68°C internal.
Once the tumescent fluid has been infused and the appropriate size handpiece has been selected, the internal probe is inserted into the subcutaneous adipose layer and the external probe is positioned on the skin surface (Figure 2). The internal probe heats the tissue and monitors the internal temperature. The external “return” electrode monitors external temperature. The device is activated and the handpiece is passed back and forth; the visual and auditory cues provided by the device enable to operator to heat the tissue to the setpoint temperatures. Internal and external temperatures are set prior to treatment, and the device automatically modulates RF energy according to tissue impedance and measured temperature, turning itself on and off as necessary.
Treatment areas are divided into smaller constituent areas to facilitate efficient uniform heating. Once the set temperature is achieved there is no need to “re-treat” or “stack” treatments. Target temperatures are the primary treatment “endpoint”; secondary endpoints include easy gliding of the internal probe through the subcutaneous tissues, and tactile warmth of the treated skin. A thermal camera could be used, but is not necessary because this technology offers built-in temperature monitoring.
After the treatment area has been uniformly heated to the target temperature, liposuction is performed to aspirate the liquified subcutaneous fat and heated tumescent fluid. The exception to this rule would be in cases where autologous fat grafting will be performed, in which case liposuction must be completed before performing bipolar RF. In all cases, the final step is subcutaneous basket cannula “equalization.” 17 All stab incisions are closed with 5-0 Prolene, and all 16-gauge needle holes are allowed to close on their own. Occasionally, cases with minimal fat may receive no additional liposuction (Video, available as supplemental material online at www.aestheticsurgeryjournal.com).
Aftercare following bipolar RF and liposuction is identical to suction-assisted lipectomy (SAL) or PAL in our practice. We utilize foam padding and compression garments for the first 3 to 7 days following the procedure. Lymphatic massage is considered on a case-by-case basis. Patients resume light activity and exercise at 3 days postprocedure, and regular activity after 1 week. We counsel patients to expect to wait until 6 months after the procedure before they see the final results.
RESULTS
We treated 745 patients (106 men and 639 women) at both centers. A total of 608 patients were treated at the Florida center and 137 patients at the New Jersey center. Thirty patients underwent retreatment of previous areas and were not included in this analysis. The average age was 50.5 years (range, 18-84 years) (Table 2). The total number of treatment areas was 895 and the average number of areas treated per patient was 1.62 (range, 1-7 areas) (Table 2). The most commonly treated areas were abdomens (218), necks (192), flanks (120), thighs (105), and arms (64) (Table 3). The proportions of areas treated remained relatively stable over time, apart from an increase in the number of necks treated, reflecting the introduction of the AccuTite handpiece and our increasing familiarity with its use (Figure 4). The BMI of the initial 100 patients treated was compared with that of the last 100 patients to evaluate differences in patient selection with increased experience (Table 4). The difference between average initial BMI (24.5 kg/m2; range, 17.3-34.6 kg/m2) and final BMI (24.6 kg/m2; range, 17.1-36.9 kg/m2) did not reach statistical significance (P = 0.69).
| Number of patients . | 745 . |
|---|---|
| Female | 639 (86%) |
| Male | 106 (14%) |
| Average age (years) | 50.5 (range, 18-84) |
| Average areas treated per patient | 1.62 (range, 1-7) |
| Number of patients . | 745 . |
|---|---|
| Female | 639 (86%) |
| Male | 106 (14%) |
| Average age (years) | 50.5 (range, 18-84) |
| Average areas treated per patient | 1.62 (range, 1-7) |
| Number of patients . | 745 . |
|---|---|
| Female | 639 (86%) |
| Male | 106 (14%) |
| Average age (years) | 50.5 (range, 18-84) |
| Average areas treated per patient | 1.62 (range, 1-7) |
| Number of patients . | 745 . |
|---|---|
| Female | 639 (86%) |
| Male | 106 (14%) |
| Average age (years) | 50.5 (range, 18-84) |
| Average areas treated per patient | 1.62 (range, 1-7) |
| Area . | Total . | First 100 . | Last 100 . |
|---|---|---|---|
| Abdomen | 218 | 26 | 27 |
| Thighs | 192 | 22 | 8 |
| Neck | 120 | 21 | 45 |
| Flanks | 105 | 17 | 16 |
| Back | 64 | 17 | 3 |
| Arms | 62 | 14 | 11 |
| Banana rolls | 27 | 8 | 1 |
| Axilla | 26 | 5 | 5 |
| Knees | 17 | 5 | 1 |
| Chest | 16 | 2 | 0 |
| Breasts | 15 | 1 | 2 |
| Mons | 14 | 1 | 1 |
| Jowls | 10 | 0 | 0 |
| Buttocks | 9 | 0 | 1 |
| Total | 895 | 139 | 121 |
| Area . | Total . | First 100 . | Last 100 . |
|---|---|---|---|
| Abdomen | 218 | 26 | 27 |
| Thighs | 192 | 22 | 8 |
| Neck | 120 | 21 | 45 |
| Flanks | 105 | 17 | 16 |
| Back | 64 | 17 | 3 |
| Arms | 62 | 14 | 11 |
| Banana rolls | 27 | 8 | 1 |
| Axilla | 26 | 5 | 5 |
| Knees | 17 | 5 | 1 |
| Chest | 16 | 2 | 0 |
| Breasts | 15 | 1 | 2 |
| Mons | 14 | 1 | 1 |
| Jowls | 10 | 0 | 0 |
| Buttocks | 9 | 0 | 1 |
| Total | 895 | 139 | 121 |
| Area . | Total . | First 100 . | Last 100 . |
|---|---|---|---|
| Abdomen | 218 | 26 | 27 |
| Thighs | 192 | 22 | 8 |
| Neck | 120 | 21 | 45 |
| Flanks | 105 | 17 | 16 |
| Back | 64 | 17 | 3 |
| Arms | 62 | 14 | 11 |
| Banana rolls | 27 | 8 | 1 |
| Axilla | 26 | 5 | 5 |
| Knees | 17 | 5 | 1 |
| Chest | 16 | 2 | 0 |
| Breasts | 15 | 1 | 2 |
| Mons | 14 | 1 | 1 |
| Jowls | 10 | 0 | 0 |
| Buttocks | 9 | 0 | 1 |
| Total | 895 | 139 | 121 |
| Area . | Total . | First 100 . | Last 100 . |
|---|---|---|---|
| Abdomen | 218 | 26 | 27 |
| Thighs | 192 | 22 | 8 |
| Neck | 120 | 21 | 45 |
| Flanks | 105 | 17 | 16 |
| Back | 64 | 17 | 3 |
| Arms | 62 | 14 | 11 |
| Banana rolls | 27 | 8 | 1 |
| Axilla | 26 | 5 | 5 |
| Knees | 17 | 5 | 1 |
| Chest | 16 | 2 | 0 |
| Breasts | 15 | 1 | 2 |
| Mons | 14 | 1 | 1 |
| Jowls | 10 | 0 | 0 |
| Buttocks | 9 | 0 | 1 |
| Total | 895 | 139 | 121 |
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| Average | 22.7 | 23.3 | 23.1 | 26.1 | 25.8 | 26 | 24.5 | 24.6 | 24.5 |
| Minimum | 17.3 | 17.1 | 17.1 | 19.4 | 19.1 | 19.1 | 17.3 | 17.1 | 17.1 |
| Maximum | 34 | 29.3 | 34 | 34.6 | 36.9 | 36.9 | 34.6 | 36.9 | 36.9 |
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| Average | 22.7 | 23.3 | 23.1 | 26.1 | 25.8 | 26 | 24.5 | 24.6 | 24.5 |
| Minimum | 17.3 | 17.1 | 17.1 | 19.4 | 19.1 | 19.1 | 17.3 | 17.1 | 17.1 |
| Maximum | 34 | 29.3 | 34 | 34.6 | 36.9 | 36.9 | 34.6 | 36.9 | 36.9 |
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| Average | 22.7 | 23.3 | 23.1 | 26.1 | 25.8 | 26 | 24.5 | 24.6 | 24.5 |
| Minimum | 17.3 | 17.1 | 17.1 | 19.4 | 19.1 | 19.1 | 17.3 | 17.1 | 17.1 |
| Maximum | 34 | 29.3 | 34 | 34.6 | 36.9 | 36.9 | 34.6 | 36.9 | 36.9 |
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| Average | 22.7 | 23.3 | 23.1 | 26.1 | 25.8 | 26 | 24.5 | 24.6 | 24.5 |
| Minimum | 17.3 | 17.1 | 17.1 | 19.4 | 19.1 | 19.1 | 17.3 | 17.1 | 17.1 |
| Maximum | 34 | 29.3 | 34 | 34.6 | 36.9 | 36.9 | 34.6 | 36.9 | 36.9 |
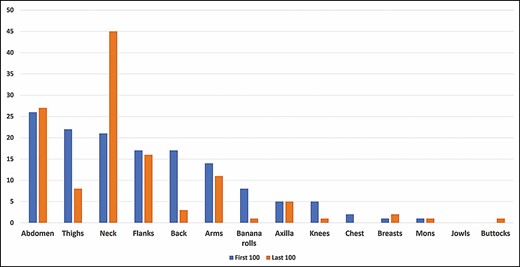
Number of treatments performed by area for the first 100 and last 100 patients.
General anesthesia was used for 242 patients (32%) and local anesthesia was used for 503 (68%); this proportion remained stable over time (Table 5). Local anesthesia cases received 1 mg Ativan and 75 Demerol intramuscularly preoperatively until December 2019, when MKO melt sublingual tabs (ImprimisRx, San Diego, CA) were used at 1 clinical site; the other site used Valium 10 to 20 mg and 1 to 2 Percocet (325 mg/5 mg) orally. Pro-Nox (CAREstream Medical, Surrey, British Columbia, Canada) on-demand inhalational nitrous oxide was used in some local anesthesia cases as well, enabling patients to self-administer nitrous oxide during the procedure.
| . | All cases (%) . | First 100 . | Last 100 . |
|---|---|---|---|
| General anesthesia | 242 (32.5) | 30 | 29 |
| Local anesthesia | 503 (67.5) | 70 | 71 |
| . | All cases (%) . | First 100 . | Last 100 . |
|---|---|---|---|
| General anesthesia | 242 (32.5) | 30 | 29 |
| Local anesthesia | 503 (67.5) | 70 | 71 |
| . | All cases (%) . | First 100 . | Last 100 . |
|---|---|---|---|
| General anesthesia | 242 (32.5) | 30 | 29 |
| Local anesthesia | 503 (67.5) | 70 | 71 |
| . | All cases (%) . | First 100 . | Last 100 . |
|---|---|---|---|
| General anesthesia | 242 (32.5) | 30 | 29 |
| Local anesthesia | 503 (67.5) | 70 | 71 |
The first and last 100 patients treated were reviewed retrospectively to assess for the occurrence of complications. In this manner, if there was a true learning curve as evidenced by adverse events (AEs), it would be detected. Complication data are listed in Table 6. From the initial 100 patients treated to the final 100 patients in this study, the incidence of AEs decreased from 21% to 19%, although this did not reach statistical significance (P = 0.86) The 2 most common complications were temporary swelling (9%) and nodules (8.5%), and these were self-limited. Other minor complications included hyperpigmentation (0.5%) and contour irregularity (1%). In all, 96% of the analyzed patients (n = 192) were satisfied with their treatment. There was a 40% reduction in patient dissatisfaction from the first 100 (5%) to the last 100 patients (3%). Nine (4.5%) of the initial 100 patients had retreatment of selected areas. The final 100 patients sampled did not have any retreatments, perhaps reflecting increased experience with this procedure. Selected examples of a variety of patients and areas treated can be seen in Figures 5 to 8 and Supplemental Figures 1, 2.
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Complications . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| None | 35 (70%) | 38 (76%) | 73 (73%) | 44 (88%) | 43 (86%) | 87 (87%) | 79 (79%) | 81 (81%) | 160 (80%) |
| Swelling | 5 (10%) | 15 (28%) | 18 (18%) | 5 (10%) | 15 (15%) | 18 (9%) | |||
| Nodules/lumps | 2 (4%) | 8 (16%) | 10 (10%) | 4 (8%) | 3 (6%) | 7 (7%) | 6 (6%) | 11 (11%) | 17 (8.5%) |
| Contour deformity | 1 (2%) | 0% | 1 (1%) | 1 (2%) | 0% | 1 (1%) | 2 (2%) | 0% | 2 (1%) |
| Hyperpigmentation | 0% | 0% | 0% | 1 (2%) | 0% | 1 (1%) | 1 (1%) | 0% | 1 (0.5%) |
| “Didn’t work”/dissatisfied | 3 (6%) | 0% | 3 (3%) | 2 (4%) | 3 (6%) | 5 (5%) | 5 (5%) | 3 (3%) | 8 (4%) |
| Subsequent surgery | 0% | 0% | 0% | 1 (2%) | 1 (2%) | 2 (2%) | 2 (2%) | 0% | 2 (1%) |
| Repeat BodyTite | 9 (18%) | 0% | 9 (9%) | 9 (9%) | 0% | 9 (4.5%) | |||
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Complications . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| None | 35 (70%) | 38 (76%) | 73 (73%) | 44 (88%) | 43 (86%) | 87 (87%) | 79 (79%) | 81 (81%) | 160 (80%) |
| Swelling | 5 (10%) | 15 (28%) | 18 (18%) | 5 (10%) | 15 (15%) | 18 (9%) | |||
| Nodules/lumps | 2 (4%) | 8 (16%) | 10 (10%) | 4 (8%) | 3 (6%) | 7 (7%) | 6 (6%) | 11 (11%) | 17 (8.5%) |
| Contour deformity | 1 (2%) | 0% | 1 (1%) | 1 (2%) | 0% | 1 (1%) | 2 (2%) | 0% | 2 (1%) |
| Hyperpigmentation | 0% | 0% | 0% | 1 (2%) | 0% | 1 (1%) | 1 (1%) | 0% | 1 (0.5%) |
| “Didn’t work”/dissatisfied | 3 (6%) | 0% | 3 (3%) | 2 (4%) | 3 (6%) | 5 (5%) | 5 (5%) | 3 (3%) | 8 (4%) |
| Subsequent surgery | 0% | 0% | 0% | 1 (2%) | 1 (2%) | 2 (2%) | 2 (2%) | 0% | 2 (1%) |
| Repeat BodyTite | 9 (18%) | 0% | 9 (9%) | 9 (9%) | 0% | 9 (4.5%) | |||
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Complications . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| None | 35 (70%) | 38 (76%) | 73 (73%) | 44 (88%) | 43 (86%) | 87 (87%) | 79 (79%) | 81 (81%) | 160 (80%) |
| Swelling | 5 (10%) | 15 (28%) | 18 (18%) | 5 (10%) | 15 (15%) | 18 (9%) | |||
| Nodules/lumps | 2 (4%) | 8 (16%) | 10 (10%) | 4 (8%) | 3 (6%) | 7 (7%) | 6 (6%) | 11 (11%) | 17 (8.5%) |
| Contour deformity | 1 (2%) | 0% | 1 (1%) | 1 (2%) | 0% | 1 (1%) | 2 (2%) | 0% | 2 (1%) |
| Hyperpigmentation | 0% | 0% | 0% | 1 (2%) | 0% | 1 (1%) | 1 (1%) | 0% | 1 (0.5%) |
| “Didn’t work”/dissatisfied | 3 (6%) | 0% | 3 (3%) | 2 (4%) | 3 (6%) | 5 (5%) | 5 (5%) | 3 (3%) | 8 (4%) |
| Subsequent surgery | 0% | 0% | 0% | 1 (2%) | 1 (2%) | 2 (2%) | 2 (2%) | 0% | 2 (1%) |
| Repeat BodyTite | 9 (18%) | 0% | 9 (9%) | 9 (9%) | 0% | 9 (4.5%) | |||
| . | Site 1 . | Site 2 . | Combined . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Complications . | First 50 . | Last 50 . | Combined . | First 50 . | Last 50 . | Combined . | First 100 . | Last 100 . | Combined . |
| None | 35 (70%) | 38 (76%) | 73 (73%) | 44 (88%) | 43 (86%) | 87 (87%) | 79 (79%) | 81 (81%) | 160 (80%) |
| Swelling | 5 (10%) | 15 (28%) | 18 (18%) | 5 (10%) | 15 (15%) | 18 (9%) | |||
| Nodules/lumps | 2 (4%) | 8 (16%) | 10 (10%) | 4 (8%) | 3 (6%) | 7 (7%) | 6 (6%) | 11 (11%) | 17 (8.5%) |
| Contour deformity | 1 (2%) | 0% | 1 (1%) | 1 (2%) | 0% | 1 (1%) | 2 (2%) | 0% | 2 (1%) |
| Hyperpigmentation | 0% | 0% | 0% | 1 (2%) | 0% | 1 (1%) | 1 (1%) | 0% | 1 (0.5%) |
| “Didn’t work”/dissatisfied | 3 (6%) | 0% | 3 (3%) | 2 (4%) | 3 (6%) | 5 (5%) | 5 (5%) | 3 (3%) | 8 (4%) |
| Subsequent surgery | 0% | 0% | 0% | 1 (2%) | 1 (2%) | 2 (2%) | 2 (2%) | 0% | 2 (1%) |
| Repeat BodyTite | 9 (18%) | 0% | 9 (9%) | 9 (9%) | 0% | 9 (4.5%) | |||

A 53-year-old female patient whose neck was treated with FaceTite. (A) Pretreatment. (B) Posttreatment—1 month.
DISCUSSION
The liposuction finesse offered by bipolar RFAL has completely changed our approach to lipocontouring. Prior to its use, we limited liposuction to younger patients without significant skin laxity, and to the treatment of traditional areas such as the abdomen, flanks, and outer thighs. We frequently treated these larger areas under general anesthesia.
In this largest series to date, our average patient age was 51 years with the youngest being 18 years and the oldest being 84 years. Two-thirds of patients were treated under local anesthesia and oral sedation. Generally, 1 to 2 areas were treated at a time. It was surprising for us to note that many patients elected to have multiple bipolar RFAL procedures in which small areas were treated under local anesthesia, instead of 1 larger procedure with multiple areas treated under general anesthesia. Many patients started with 1 area to see whether they liked the results before proceeding to have additional areas treated.
Approximately one-third of patients were treated under general anesthesia, and many of these patients had additional procedures such as breast augmentation performed concurrently. The high percentage of patients treated under local anesthesia appears to be a paradigm shift, with older patients having minimally invasive procedures, and our impression was that these were often new patients who had not previously considered liposuction due to age or aversion to general anesthesia.
The benefits of bipolar RFAL are readily apparent, and we believe this influenced our patients’ decisions to undergo this treatment. Many patients who were eventually treated with bipolar RFAL were initially consulted for noninvasive procedures (eg, CoolSculpting, SculpSure, Velashape, or Vanquish), but chose bipolar RFAL due to a reduced number of treatments per area, no risk of hypertrophy, and the additional skin tightening provided by the technique. It should be noted again that most small-area RFAL patients returned to exercise at 3 days postprocedure with limited use of compression garments—additional reasons, we surmise, for the increased acceptance of bipolar RFAL. Finally, in contrast to laser energy, which generates heat through selective photothermolysis (eg, by targeting a pigment chromophore), bipolar RF works by delivering RF energy directly to the tissue18,19 and is therefore effectively “color blind.” Although it is possible for thermal energy to result in hyperpigmentation, no patient in this series experienced skin color changes from the energy placed.
The mechanism of bipolar RF is through the controlled delivery of thermal energy to the dermis and subcutaneous fibroseptal network (FSN).16,18,20,21 The resistance of tissues to the flow of RF energy results in the generation of heat.18,19 RF energy has been shown to cause thermally induced contraction of collagen and restructuring of collagen fibers.11,18,20,22 When thermal energy is delivered to the dermis, it results in skin tightening,7,16,18,22,23 and when delivered to the FSN it produces volumetric contraction.16,20 These changes have been shown to occur at around 70°C for the subcutaneous tissues of the septofascial network and FSN,11,16 and optimally between 39°C and 42°C for the skin in order to avoid thermal injury. In prior work, the effective temperature for tightening was seen to be 47°C by thermal camera surface measurements.7 There is a correlation between the bipolar RF external probe measurement of 42°C and the thermal camera measurement: these are 2 different ways to measure the same reading, from a “top-down” or “bottom-up” perspective.
The advantages of tightening technology are obvious: avoiding the laxity that occurs with traditional liposuction, and contouring and tightening body areas that are already lax. The areas treated in this large series varied from traditional liposuction areas (eg, necks, abdomen, flanks, and thighs) to nontraditional areas (eg, jowls, axillary rolls, arms in older patients, banana rolls, and calves). The smaller probes were especially useful in treating small areas.
The question arises as to what advantages bipolar RFAL possesses compared to monopolar RFAL such as ThermiTite (Thermi, Irving, TX) and to LAL. In our opinion, having used both technologies, bipolar RFAL offers simplified external temperature monitoring and more power (and thus faster treatment) when compared to the original generation of monopolar technology. Additionally, the bipolar nature of the RF energy delivered spares nerves by only treating the tissue in between the electrodes (Figure 2). Compared to LAL, bipolar RFAL is performed with a less complex, more solid-state device, with fewer moving parts and fewer service issues—this is particularly relevant if the device is to be transported from office to operating room. Like laptops, solid-state devices contain circuit boards which are not prone to damage from movement. Lasers are complex instruments with mirrors and light pathways that are very dependent on calibration. Movement can easily alter the precision of these devices, which may then require servicing upon a change in location.
Complications of energy-based devices are mostly due to excessive energy—ie, creating a burn or an area of fibrosis. Laser liposuction, in particular, produced many reports of burns, which in our opinion were due to inadequate temperature monitoring. With bipolar RF there is constant temperature monitoring and therefore the risk of burns is much lower than with previous techniques. A review of the incidences of AEs for every energy device mentioned in this article would be interesting but is outside the scope of this paper.
In this series we elected to compare an initial group of patients to a later group to see if there was a learning curve to avoiding complications, and in fact we did see a decrease in AEs from 21% to 19% (although this did not reach statistical significance). Most of these AEs were self-limited nodules or swelling. There were only 2 true burns in this large series, minor arm burns which healed uneventfully. These were thought to be caused by the use of the 40-W handpiece to treat very thin women for skin tightening of the arms. We subsequently learned to move this handpiece a bit more rapidly and this eliminated any further issues. It was decided not to quantify the middle 545 patients as there were no major complications and the minor AEs of swelling, nodules, etc, of this middle group did not add any value to this paper. The low incidence of complications may also be due to the senior authors’ expertise as both have had many years of experience with energy-based devices.
Novices to energy-based liposuction need to be aware that complications of bipolar RF beyond those of SAL are avoidable with proper technique and deserve mention. An “end hit,” or “end dermal hit,” occurs when the tip of the internal probe is thrust into the dermis at a perpendicular angle during treatment. It is most often seen when treating around a convex contour, such as a bony prominence. Care must be taken to recognize the contour in these areas and focus on passing the internal electrode parallel to the skin. Manual retraction of the skin is useful to maintain a flat surface (like the process of making a flat surface for a dermatome during a split-thickness skin graft). When an “end hit” occurs, it can usually be felt as resistance in the handpiece as the internal probe abruptly stops within the dermis on a pass. The “end hit” can be seen on the skin surface as a small weal (Figure 9). Treatment is immediate application of ice, and we always have a sterile glove filled with ice cubes on the field for this purpose. If treated promptly, there are no long-term consequences. If untreated, however, the “end hit” could result in a full-thickness burn.
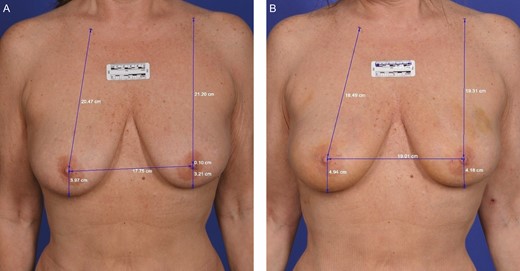
A 61-year-old female who received FaceTite treatment to circumferential breast with calibrated measurements. (A) Pretreatment. (B) Posttreatment—3 months.
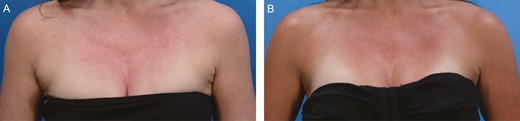
A 48-year-old female with axillary “bra fat” treated with liposuction and FaceTite. (A) Pretreatment. (B) Posttreatment—3 months.
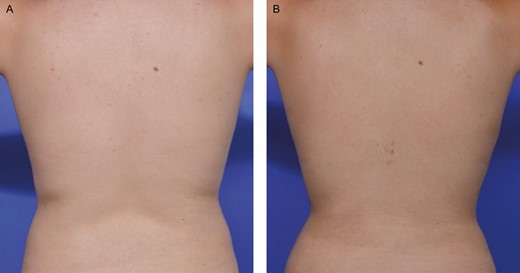
A 61-year-old female whose back and flank were treated with VASER and BodyTite. (A) Pretreatment. (B) Posttreatment—3 months.

Dermal end hit—immediate intraoperative appearance (arrow) in a 42-year-old female.
Another AE seen with bipolar RF are hardened areas or nodules. Although this complication was rare in our series (8.5%), we did obtain a biopsy of one such lesion, which was consistent with fat necrosis. If these “hard areas” (or nodules) indeed represent fat necrosis, then this underscores the importance of evacuating liquified fat after bipolar RF.
All suction lipectomy procedures may cause contour irregularities and result in the need for further surgical or nonsurgical contouring; however, AEs were extremely rare in this series. It should be noted that both senior authors had extensive experience with energy devices prior to using bipolar RFAL, and this may have contributed to the lack of AEs. However, both senior authors have trained many physicians with this technology and have kept in contact with the physicians they trained, and minimal issues have been reported. Our recommendation still stands that proper training is essential, but the learning curve is short, and bipolar RFAL technology is very safe.
One limitation of bipolar RFAL is its potential inability to achieve maximal skin tightening. The physician or patient may feel their results are adequate for a minimal incision procedure, but expectations should be tempered to not expect “surgical” (ie, excisional) tightening from the device. Another limitation is consistency from patient to patient. Although we have shown very good results in our photographs, there is variability in most tightening technologies, and even surgeries, due to differences in age, sun damage, dermal thickness, genetic factors, and unknown reasons. Fortunately, by setting proper expectations during preoperative consultation, and with adequate patient selection from experience, the vast majority of patients are satisfied with the results. We have learned from this series that patient selection is key to achieving successful outcomes—that patients with hanging skin, who are truly in need of surgical excision, will never tighten to the point of not needing surgery. Conversely, marginal patients without hanging skin who would surely sag from traditional liposuction will maintain their tissue integrity with the addition of RF. In other words, this technology tightens them enough to provide a nice appearance without causing worsening of their skin laxity. Younger patients with good elasticity have universally excellent results.
The limitations of this study include its retrospective design and lack of objective outcome data (such as volumetrics or measurements of 2-dimensional skin tightening). The homogeneity of our sample population was limited by including patients treated at 2 centers, but this larger group is more representative of the overall population undergoing these procedures. We also did not perform a pre hoc power analysis prior to making statistical comparisons between groups. However, this study was not designed to experimentally assess the technology used, but rather to provide a thorough clinical review of our experience with the device.
CONCLUSIONS
We have shown that the combination of bipolar RF and focused liposuction can produce impressive results under both general and local anesthesia. The limitations of our study include its retrospective design and lack of quantitative outcome metrics. Nonetheless, we believe our experience in this largest series reported to date can serve as an indicator to surgeons seeking to achieve similar results. Bipolar RF can be used to achieve elegant outcomes in patients with mild to moderate skin laxity and focused adiposity, enabling surgeons to achieve finesse in lipocontouring.
Disclosures
Dr Pozner and Dr DiBernardo are paid research investigators and speakers for InMode (Lake Forest, CA, USA) (the manufacturer of the devices discussed in this article) and have stock options. Dr DiBernardo is also a paid trainer for InMode. Dr Cook does not have a financial interest in any of the products, devices, or drugs mentioned in this article.
Funding
No funding was received for this article. The manufacturer had no control over study design, data collection, or authorship of the article.
REFERENCES
Author notes
Dr Cook and Dr Pozner are plastic surgeons in private practice in Boca Raton, FL, USA.
Dr DiBernardo is a plastic surgeon in private practice in Montclair, NJ, USA.



