-
PDF
- Split View
-
Views
-
Cite
Cite
Steven R Cohen, Sierra Hewett, Patrick Baraf, Sarah Jiwon Crowley, Michael Atlan, Facelift With Power-Assisted Dissection: A Preliminary Report, Aesthetic Surgery Journal, Volume 41, Issue 6, June 2021, Pages 641–651, https://doi.org/10.1093/asj/sjaa213
Close - Share Icon Share
Abstract
Subcutaneous elevation of the skin has remained a key component in all facelift techniques.
The aim of this preliminary report was to introduce the ABC facelift as a 3-step method addressing photodamage, soft tissue laxity, and areas of bone and volume loss.
The procedure consists of: (A) anatomic and regenerative adipose grafting prior to skin elevation; (B) the use of a Baraf elevator for takedown of perpendicular subcutaneous fibers following hydrodissection of the skin flaps with tumescent solution; and (C) cautery dissection of the superficial muscular aponeurotic system (SMAS) and platysma in the neck.
Thirty-four patients (31 females; 3 male), aged 50 to 77 years at the date of procedure, underwent an ABC facelift. Dissection of the skin flaps and SMAS elevation were faster than with traditional methods, averaging 10 to 15 minutes per hemiface. Bleeding was reduced (average estimated blood loss, 12 mL) and the skin flaps appeared better perfused with less venous engorgement and ecchymosis than achieved with sharp scissor dissection. In general, patients appeared to have shorter postoperative recovery courses and less social downtime secondary to bruising and edema.
The ABC facelift addresses facial laxity, volume loss, and skin aging with 3 simple steps: anatomic and regenerative fat grafting, combined with power-assisted dissection of the skin and cautery elevation of the SMAS. The use of more advanced hydrodissection tools to achieve further improvements in layer separation is currently being investigated.

Facelift surgery began in the early 1900s after Hollander lifted the facial skin to improve the corners of the mouth and jowls of a Polish aristocrat.1 Since that time, subcutaneous elevation of the skin has remained a key component of all facelift techniques and is generally carried out with sharp scissor dissection. Recent reports of scissor-free dissection with progressively larger-diameter dilators2 as well as water-assisted dissection3 have demonstrated improved blood supply in the skin flaps and decreased hematoma formation. Manipulation of the superficial muscular aponeurotic system (SMAS) began in 1968,4 and was promoted by Skoog4,5 and later developed into its various techniques by a number of surgeons.6-10 Most surgeons address the SMAS with a range of techniques, from plication to deep plane. Although fat grafting was introduced in 1893,11 large-volume fat grafting at the time of facelift surgery was popularized by Guerrosantos,12 Marten,13 and our group14 in the early and mid-2000s. Rohrich15 focused our attention on the anatomy of facial fat compartments, rightfully redirecting facial fat grafting away from its use as a natural aesthetic filler and toward an anatomic reconstruction. Mendelson,15,16 Lambros,17 and others18,19 characterized the age-related changes that occur in specific anatomic regions of the craniofacial skeleton and its overlying soft tissue envelope. In 2001, Zuk et al20 published their landmark article, which characterized the stromal vascular fraction (SVF) within fat and showed that the multilineage cells (mesenchymal stem cells) found in fat were capable of differentiating into other tissue types. Shortly thereafter, Cohen and Holmes21 were first to treat patients with SVF-enriched fat grafts in an institutional review board–approved trial in 8 patients in 2003. Herein, the ABC facelift technique is described, fusing these newer techniques and concepts into a simple, 3-step method that decreases operative time for skin and SMAS elevation through the use of hydrodissection, a Baraf elevator, and cautery, while providing a relatively bloodless cavity from the tumescent solution. There is less traction during skin elevation and skin flap ischemia time is minimized—a property that could be extremely useful with smokers. Therefore, the ABC facelift provides 2 possible benefits: less skin ischemia time as the majority of the dissection is done before completion of the skin incision; and reduced skin traction and retraction times. The procedure utilizes the deep-plane,22,23 sub-SMAS approach, along with a platysmal window to better contour the neck. In addition to anatomic replacement of lost fat and areas of bone resorption, fat grafting provides regenerative effects in the skin and subcutaneous tissue, demonstrating improved circulation, and reversal of aging in collagen and elastin fibers.24 Bone losses that can be addressed with fat grafting are the subtle losses from the pyriform, the supraorbital rims, the mandibular body, the ramus and the orbital shown in computed tomography aging studies by Kahn and Mendelson.16,25 Previously, using this technique of anatomic and regenerative fat grafting, we reported improved facial volumes in patients undergoing facelifts 24 months after fat grafting.24,26
The ABC facelift involves 3 steps (Figure 1, Videos 1-3):
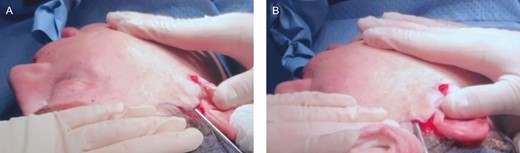
Intraoperative photographs of a 55-year-old female undergoing ABC facelift with lipoharvest from the abdomen and bilateral outer thighs. (A) Power-assisted, hydrodissection following adipose grafting. (B) Baraf elevator for takedown of perpendicular subcutaneous fibers.
Adipose grafting by an anatomic and regenerative approach called injectable tissue replacement and regeneration (ITR2—this involves regenerative, multiplanar reconstruction, and replacement of tissue losses).27
The use of a Baraf elevator to take down the remaining vertical fibroseptal bands and off-label power-assisted dissection (PAD) by hydrodissection for subcutaneous tumescent tissue separation (Figure 1, Videos 1, 2).28
Cautery elevation of the SMAS followed by use of a Trepsat spreader to approach the deep midfacial planes and lateral subplatysmal window with a platysmal sling, and vertical elevation of the SMAS to contour the neck (Video 3).
METHODS
This study began in February 2019 and concluded 12 months later in February 2020. During consultation, patients were evaluated based on the degree of severity of the 3 major phenotypic changes seen with facial aging: (1) photodamage; (2) subcutaneous deep and superficial fat compartment loss and bone loss and/or pre-existing skeletal deficiency; and (3) laxity. Exclusion and inclusion criteria were determined on the basis of the severity of each of the above 3 findings. Patients presenting with minimal degrees of severity were excluded and provided with an alternative treatment plan to address their aging concerns. Patients with deep and superficial fat loss, apparent bone resorption, photodamage, and areas of skin thinning were selected to undergo the ABC facelift. Institutional review board approval was not required. The Declaration of Helsinki was used as a guiding principle for this study, and patients provided written consent for all surgical procedures and anesthesia.
ABC Facelift Technique
Adipose Grafting by ITR2
The ITR2 procedure27,29 is a standardized method of fat grafting. This procedure:
Diagnoses the anatomic components of volume loss by evaluating the surface topography of the face (Supplemental Figure 1).
Addresses specific anatomic losses of these different tissues, including skin, facial fat in the deep and superficial compartments, and bone.
Replaces these anatomic losses of fat with autogenous fat grafts, categorized as millifat (1.8- to 2.4-mm parcel size) for structural replacement of bone and deep fat losses, microfat (1- to 1.2- mm parcel size) for superficial fat replacement, and nanofat (≤500-µm parcel size) for dermal and epithelial replacement and/or regeneration (Figure 2). The nanofat is delivered by cannulas, needles, microneedles, and/or as a compounded biocreme.24
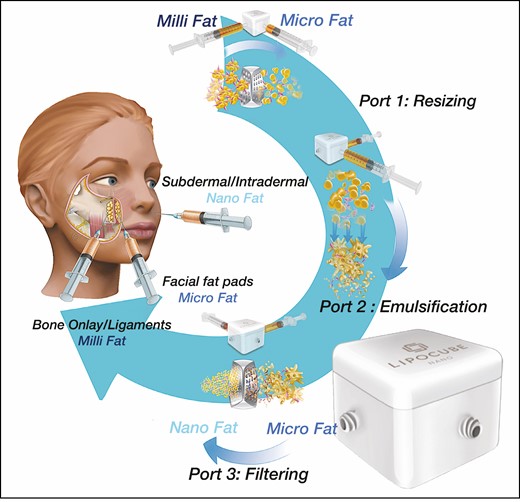
ITR2 for anatomic fat grafting in the ABC facelift uses mechanical dissociation of millifat harvested with a 1.8-mm × 1-mm hole cannula and processed with a small “lab-in-a-box” (Nanocube; Lipocube, Inc., London, UK) into microfat (1-mm parcel size) and cell-optimized nanofat (500-μm parcel size). Fat processed with the Nanocube retains the fibrous tissue matrix with regenerative stromal vascular fraction cells. ITR2, injectable tissue replacement and regeneration.
More detailed information on the ITR2 fat-grafting method is given in Cohen et al.29 Fat grafts are placed by a retrograde threading technique directly into the tissue planes and specific fat pad compartments. In our experience, grafted fat remains fixed to these tissue planes and does not behave like a liquid that spills out with dissection. Rather, in our clinical experience, large-volume fat grafting following the facelift procedure is more prone to collect under the flap.
Baraf Subcutaneous Skin Elevation and PAD with Tumescent Hydrodissection
The facelift is performed immediately following ITR2 injection of millifat and microfat, but before nanofat microneedling, sharp needle intradermal fat grafting injection, and/or nanofat biocreme topical application. Once millifat and microfat fat have been injected into the deep and superficial compartments, respectively, the preauricular and postauricular incisions are marked. When the distance between the hairline and lateral brow is wide, it is best to preserve this distance by keeping the incision along the anterior border of the sideburn. When the distance between the hairline and lateral brow is narrow, and the sideburn is long, or if the patient is a male, the incision can be made in the hair.
The proposed incision is injected with 0.25% bupivicaine with 1:200,000 epinephrine. It should be noted that our clinic does not include lidocaine in the tumescent solution used for hydrodissection to avoid any adverse affect on fat-grafting outcomes. Instead, epinephrine fluid is mixed with lactated Ringer’s solution in a 1:1000 ratio and infiltrated with a MicroAire (Charlottesville, VA) spatulated cannula (3-hole, 15 cm long, 3.0-mm diameter with a port length of 1.5 mm) which is introduced in a vibratory fashion through the 3 small incisions along the proposed facelift incision line (Figure 1A, Video 1). One site is located at the sideburn, a second site is located in front of the earlobe, and the third site is placed at the junction of the hair and skin in the postauricular region. These incisions are opened with a no. 15 blade.
Through each of the small incisions, a small amount of subcutaneous dissection with a scissor or microcautery is performed to ensure one is in the correct subcutaneous plane. The tumescent fluid is injected subcutaneously by reciprocation and tumescent hydrodissection with the MicroAire cannula at a reciprocation speed of 4000 cycles/min and a flow rate of 80 mL/min via a Byron E-Z pump (Mentor, Inc., Santa Barbara, CA) to create numerous subcutaneous tunnels (Figure 3). The skin is undermined 1 to 2 cm above the zygomatico-orbital retaining ligament to the mandibular retaining ligament and anteriorly to roughly a line dropped perpendicular to the lateral canthus. In the neck, depending on the extent of skin redundancy and the status of the submental anatomy, in some cases, a submental incision was made. In the majority of cases, the platysmal window extended to the anterior border of the platysma, and the skin dissection approached the midline in the neck. This is not a composite approach like Hamra’s, but a combination of Mendelson and Jacono’s approach. The deep plane is entered at the junction of the mobile and fixed SMAS, which is lower and more anterior than the high SMAS. Given that fat is injected into the central, deep cheek region, the high SMAS may not be needed for cheek augmentation. The SMAS of the midface is contiguous with the platysma in the neck, which is dissected transversely along the junction of the posterior submental border and lower neck. It is then transversely divided.
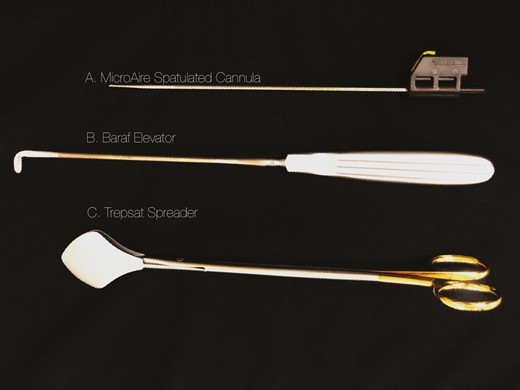
The instruments used in the ABC facelift technique. (A) MicroAire spatulated cannula (3-hole, 15 cm long, 3.0-mm diameter with a port length of 1.5 mm). (B) Baraf elevator. (C) Trepsat spreader.
Once the tunneling is complete, and 150 mL of tumescent fluid has been placed on each side of the face, a Baraf hockey-stick elevator (Pouret Medical, Clichy, France) is then inserted through the 3 small incisions and used to take down the remaining vertical subcutaneous attachments, thus opening up a subcutaneous cavity with no excessive tension related to the use of retractors. The incisions are then connected with a no. 15 blade anteriorly and a no. 10 blade posteriorly, elevating the skin to expose the bloodless cavity and the underlying SMAS (Figure 1B, Video 2). The few remaining bands are easily taken down with a scissor.
Cautery SMAS Elevation
The SMAS is incised with electrocautery and proceeds along the attached/loose SMAS junction approximately 1 cm in front of the tragus and is continued into the neck just anterior to the sternocleidomastoid muscle border and the fixed platysmal auricular fascia. Dissection of the SMAS continues until reaching the anterior border of the parotid (Figure 4, Video 3). The cautery is set at 15 to 20 joules and its “spray” functions as a nerve stimulator, notifying the surgeon when they are close to facial nerve branches. The surgical assistant watches for facial movement to prevent potential damage from nerve injury. Electrocautery of the SMAS is discontinued once facial musculature activation is seen, signaling close proximity to the nerve. Gentle elevation of the remaining SMAS into the deep spaces is performed with a Trepsat elevator (ASSI, Westbury, NY) (Figure 3). Once the looser areolar layer between the SMAS and the deep planes of the face is reached, a Trepsat spreader is inserted to gently free up the remaining SMAS, entering the deep premasseteric and prezygomatic planes/spaces of the face.30 In the neck, the Trepsat elevator is placed under the platysma window laterally and gently spread until the anterior border of the submandibular gland or platysma is reached (Video 3).
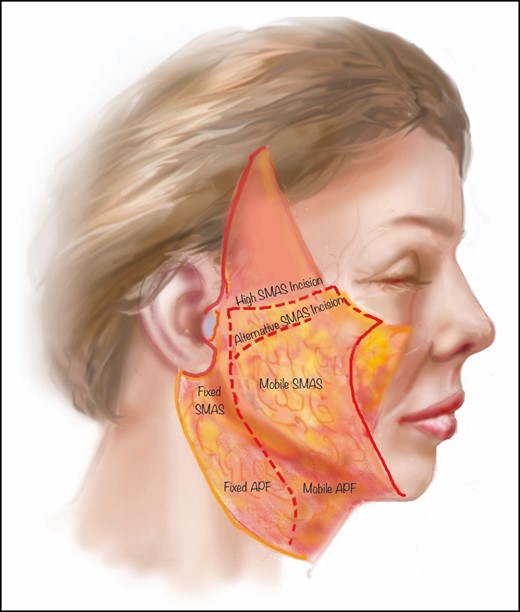
Schematic representation of SMAS cautery dissection. SMAS, superficial muscular aponeurotic system; APE, auricular platysmal fascia.
The SMAS is then elevated vertically with either a DeBakey forceps or an atraumatic clamp while inspecting the effect on the neck and nasolabial folds. In the caudal portion of the neck, the platysma is carefully divided with cautery in a transverse fashion. Pulling the platysma vertically as a sling permits tightening and contouring of the neck, while reducing most of the mildly protrusive submandibular glands and defining the inferior mandibular border (Video 3). The platysma is transected horizontally along its inferior border, while gently lifting it vertically and assessing the submental angle. The SMAS/platysma flap is sutured with a 3.0 V-Loc suture. Redundant SMAS is trimmed (Video 3).
Once the SMAS is sutured, the opposite side SMAS is addressed. Then, returning to the right side, 3 Kocher clamps are placed on the skin, one at the tragus, a second equidistant from the tragus to the earlobe attachment to the postauricular skin, and a third on the redundant postauricular skin. The skin is pulled in a vertical and slightly horizontal vector in the same direction of the long axis of the ear. The skin is trimmed perpendicular to the incision line with Iris scissors and temporarily inset at the junction of the posterior skin and hairline. Next, excess skin is trimmed along the sideburn (or more rarely in the hair), and staples are temporarily used to close the incision. Following this, the skin is redraped, again without tension, and trimmed along the preauricular incision, temporarily placing a staple above and below the tragus. The retroauricular skin is trimmed after sweeping it toward the ear incision and marking it with a pen. Once the skin flaps are trimmed on the right, the left side is dealt with in the same manner (Video 3).
At this point, the cavities on the right and left side are inspected for bleeding. Bleeding is controlled with microcautery or bipolar cautery. Fibrin sealant was previously studied by Saltz31 and was shown to reduce hematoma rates while not interfering with healing. Therefore, when the cavity is completely dry, ARTISS tissue glue (Baxter International, Inc., Deerfield, IL) is sprayed and the flaps are gently compressed for 1.5 minutes. The wounds are closed with a 4-0 Monocryl for the deep layers, 3-0 subcuticular Prolene for the postauricular incision, 6-0 nylon for the preauricular incision, and 5-0 fast-absorbing for the hair and/or sideburn. If a fractional laser is utilized, laser treatment is performed before the fat grafting and the facelift. Nanofat is delivered by microneedling and/or intradermal injection and the patient is placed in a headwrap dressing and discharged to the recovery room.
Figure 5 shows a 70-year-old woman who underwent an ABC facelift. Note the well-profused skin flaps immediately following the procedure. Figure 6 shows preoperative and 1-year postoperative photographs of a 62-year-old female who underwent an ABC facelift.

Intraoperative photograph of a 70-year-old female following suturing of the SMAS flap and skin during an ABC facelift. Note the appearance of the skin flaps, which demonstrate little bruising or venous engorgement at the conclusion of the case.

(A, C, E, G, I) Preoperative and (B, D, F, H, J) 1-year postoperative photographs of a 62-year-old woman who underwent an ABC facelift.

Ancillary Procedures
When fractional 1927-nm laser resurfacing is performed, it is done before the fat grafting and facelift surgery. In patients requiring fractional CO2 or other ablative lasers, our preference is to postpone the laser treatment until 3 months after surgery, except around the perioral rhytids, which if severe, can be treated with the fractional CO2 laser during the facelift surgery. In these cases, the fractional 1927-nm laser might be used on the skin of the face, neck, and chest.
Other ancillary procedures often performed in conjunction with face and neck lift include upper and lower blepharoplasty, temporal and/or minimally invasive brow lift, and lip-lift procedures. Genioplasty with fat, implants, or osteotomy is generally done after the facelift. The temporal and/or minimally invasive brow lift is performed after the fat grafting to the temple, forehead, and lateral supraorbital rim and prior to the upper eyelid surgery. Once completed, the upper eyelid surgery is performed, followed by lower eyelid surgery. Increasingly with periorbital fat grafting, the lower lid is treated by pinch blepharoplasty alone. When intraorbital fat is still present, either a transcutaneous or transconjunctival approach is performed and the fat is carefully removed or repositioned into the nasojugal groove. Once the lower eyelid incision is closed, a transcutaneous lateral canthopexy is carried out in most patients. The double-armed 5.0 vicryl suture is retrieved through the upper eyelid and sutured to the inner lip of the lateral orbital periosteum. Following this, if indicated, corrugators are removed through the upper eyelid incision and then the incision is closed.
A lip lift is performed last and after the pyriform aperture fat grafting, subcutaneous fat grafting, upper and lower lip fat grafting, and intradermal fat nanofat grafting. The vertical height of the lip is measured and generally marked at 14 to 15 mm from the peak of Cupid’s bow to the nostril sill and base of the columella. A gullwing type excision is performed. The wound is closed with deep 5.0 Monocryl and interrupted 6.0 nylon for the skin.
Postoperative Management
In our practice, patients are offered a home nurse for the first 24 hours. Having someone with expertise to spot a hematoma at its onset enables the surgeon to assemble his or her team and address this in an urgent manner. Most patients benefit from oral pain medication for a couple of days. Patients are encouraged to resume as many activities as they are comfortable with, apart from vigorous exercise. Direct application of ice is avoided to the flaps and areas of fat grafting. Patients who return on postoperative day 1 and have more pronounced edema are given a Medrol dose pack (methylprednisolone, Pfizer). Preauricular and submental sutures are removed on postoperative days 5 to 6. Postauricular sutures are removed on postoperative days 8 to 10.
RESULTS
Thirty-four consecutive patients underwent the ABC facelift technique. Patients are seen on a continuous basis. To date, average follow-up time is 6 months (range, 2 weeks to 12 months). With the exception of 3 males, all patients were females and the mean age at the time of procedure was 62 years (range, 50-77 years). The average volume of adipose grafted was 44.0 mL (range, 9-94.5 mL). The average volume of millifat was 31.4 mL (range, 0-61 mL), microfat 9.2 mL (range, 0-35 mL), and nanofat 3.4 mL (range, 0-44.5 mL). Nanofat was delivered in 3 different ways: (1) sharp needle intradermal fat grafting injection for radial wrinkle lines of the lips and neck; (2) microneedling (Hydra Roller, Skin Aesthetics Force, London, UK) for the entire face, neck, and chest; and (3) as a compounded biocreme for topical application at home following surgery.
One patient had minor epidermolysis at the junction of the postauricular incision and hairline that healed uneventfully. One patient underwent revision of the neck for significant neck laxity associated with severe sun damage and loss of elasticity. A small retroauricular late, liquefying hematoma was drained (2 mL) 3 weeks after the procedure. No instances of facial nerve injury occurred. Small tears occurred in the SMAS during elevation in 3 patients and were easily repaired.
Discussion
The ABC facelift with PAD provides a number of benefits to both the surgeon and the patient. The mnemonic provides a simple reminder of the main steps of the procedure: A, adipose grafting; B, Baraf elevator and PAD for skin elevation; and C, cautery elevation of the SMAS. Adipose grafting with ITR2 allows for anatomic replacement of decaying tissues with 3 sizes of fat graft parcel, ie, millifat, microfat, and nanofat. The fat is grafted into the anatomic areas of loss through 18-gauge needle incisions. The nanofat is grafted with 20-gauge cannulas, 27-gauge needles, microneedling devices, and lastly, is compounded with a liposomal transport agent, which is a transdermal topical vector that is large enough to carry nanofat and arnica into the dermis.24,27
PAD of the skin along with the Baraf elevator creates a clear, reproducible, uniform subcutaneous dissection plane with greater visibility of the underlying facial anatomy for subsequent electrocautery elevation of the SMAS and platysma. Traction is eliminated during skin flap elevation and perfusion remains largely intact during this part of the operation. Bleeding is reduced by the use of tumescent solution with epinephrine. The use of cautery for SMAS elevation and lateral platysmal elevation serves as a “nerve stimulator,” to keep a safe distance from facial nerve branches, while further reducing bleeding. Once the assistant and surgeon see evidence of muscular movement (lip twitch, etc) during cautery dissection, a Trepsat elevator is placed into the loose areolar tissue and used to enter the deep planes of the face and for subplatysmal dissection in the anterior neck. Conversely, SMAS dissection with scissors provides no warning, and hence the nerve can be inadvertently cut.
Components of tumescent fluid include epinephrine and lactated Ringer’s or normal saline, thereby acting as a vasoconstriction agent. A number of authors have recognized the benefits of using tumescent fluid for local anesthesia during facelifts. Latrenta32 reported that the use of tumescent fluid during rhytidectomy provides added benefits such as avoidance of general inhalational agents, reduced operative bleeding, reduced postoperative bruising, and improved technical ease of facial liposculpture during dissection. Recently, water-assisted liposuction (WAL) was applied to facial skin flaps in rhytidectomy as a type of safe alternative to manual dissection and showed improved facial sculpting outcomes with greater patient satisfaction.3 The authors considered the WAL method to be a helpful tool for preparing a clearly visible surgical dissection plane and for facilitating subsequent sharp scissor dissection by minimizing soft tissue trauma while separating the tissue layers. False and true retaining ligaments seem unaffected by the WAL technique and were easily identified and dissected sharply. This effect helps to reduce soft tissue trauma and may contribute to the observed reduction of postoperative hematoma formation and swelling. The authors observed no facial skin necrosis, skin sloughing, or hematoma formation. Furthermore, little intraoperative bleeding occurred during sharp scissor dissection. These authors thought that the constant water jet–assisted infiltration of Klein solution is helpful to maintain the anesthetic effect of lidocaine and the vasoconstricting effect of adrenaline over a prolonged period of time. Furthermore, the high-pressure infiltration flow of 60 mL/min during the WAL procedure seems to ensure the penetration of the Klein solution into deeper layers of the SMAS and into the dermal flap. This may be the reason why the WAL procedure led to only mild postoperative hematoma formation and swelling.
The concept of skin undermining or detachment of layers without the use of scissors has been described previously by da Luz et al.2 They described skin elevation in which skin detachment was achieved with tumescent fluid and progressively enlarged dilators. Wall33 also mentioned tissue layer separation in his paper on SAFElipo. Subcutaneous fat separation involving vibration after infiltration of the tumescent fluid was infiltrated was considered a key component of his procedure to emulsify the fat, making it easier to remove as well as redistribute.
In the ABC facelift, adipose tissue is grafted with 3 size parcels: millifat for deep compartment and structural grafting; microfat for superficial fat losses; and nanofat as a regenerative product placed intradermally and compounded into a biocreme.29 Our approach is based on the topographic assessment of all areas of bone, fat, and skin volume loss and has been shown in combination with facelift to achieve a better facial volume at 24 months than at 1 month after the procedure.22 This finding may indicate that by replacement and/or maintenance of the functional matrix of the face, aging is prolonged and decline of the tissues is partially reversed, slowing the rate of decay.26
Tumescent hydrodissection with a spatulated MicroAire cannula creates numerous subcutaneous tunnels, and produces less tissue trauma than conventional methods while reducing blood loss. The Baraf elevator is able to easily release the remaining perpendicular subcutaneous ligaments, creating a nearly bloodless cavity after the skin incision is completed with no need for skin traction, thereby creating a well-vascularized skin flap that reduces skin flap necrosis even in patients who smoke. Dissection of the SMAS with electrocautery ensures the safety of facial nerves by signaling the surgeon of their proximal location prior to cutting the nerve. Deep-plane facelift with platysmal myotomy serves to better contour the neck while providing longer-lasting results than subcutaneous facelifts alone.22,23 No issues have occurred in patients undergoing secondary facelifts, but the procedure is performed with great caution and care.
Limitations
Given the nature of this preliminary study, further training and clinical experience by other surgeons will need to be gained for this technique to become more widespread. The limitations of this study are much the same as for all facelift studies. Little can be concluded regarding long-term outcomes and often we are left with photodocumentation and clinical experience to select methods that work best in our hands. Although this is a small clinical series, the technique has worked in both primary and secondary face and neck lifts. Possible limitations include penetration of the skin or SMAS during cannula insertion, which can also occur with scissors or other forms of dissection. As with all surgical techniques, gentle handling of the tissue is required. Inadvertent penetration of the SMAS could occur, which is why the proper plane is initially established by sharp dissection under direct visualization through the 3 small incisions. Most surgeons are comfortable with liposuction in the neck and are used to guiding the cannula in the subcutaneous plane,
Conclusions
The ABC facelift addresses facial laxity, volume loss, and skin aging with 3 simple steps: (1) anatomic and regenerative fat grafting; (2) power-assisted skin hydrodissection with tumescent solution; and (3) cautery dissection of the SMAS and the use of a Trepsat elevator for deep plane and platysma window entry. The length of operative time has been reduced, and patients experienced less social downtime compared with our prior experience with scissor dissection. The use of more advanced tools for hydrodissection to achieve further improvements in layer separation is currently being investigated.
Disclosures
Dr Cohen has stock options with Millennium Medical Technologies (Carlsbad, CA); is a shareholder in the Mage Group; receives royalties from Lipocube, Inc. (London, UK); and is an investigator for Allergan (Dublin, Ireland). Dr Atlan was a former consultant for Allergan, Sebbin (Boissy l'Aillerie, France), and Motiva (Houston, TX). Dr Baraf, Dr Crowley, and Ms Hewitt declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
Author notes
Dr Baraf is a plastic surgeon in private practice in Paris, France.
Dr Crowley is a resident at a private plastic surgery practice in Paris, France.



